Stepwise Approach to Ankle/Pilon Trauma and External Fixation
John J. Stapleton
Vasilios D. Polyzois
Thomas Zgonis
Introduction
External fixation for management of acute ankle trauma is utilized for early skeletal stabilization followed by staged internal fixation or as a means for definitive fracture reduction. Temporary spanning external fixation can be applied in an efficient and simple manner to stabilize the majority of ankle and/or tibial pilon fractures. Open ankle fractures and high-energy tibial pilon fractures consistently present with a poor soft tissue envelope that typically requires fracture stabilization with a temporary external fixation device until definitive osteosynthesis is performed if feasible. Definitive open reduction and internal fixation (ORIF) can only be performed in a staged procedure and when there is adequate resolution of the soft tissue injury. Ankle and tibial pilon fractures involve a spectrum of injury patterns from simple to complex with various associated injuries and/or comorbidities. For these reasons, the care of these patients requires an individualized treatment plan. The authors present a rational stepwise approach to applying a spanning external fixation device, utilizing external fixation in combination with internal fixation, and also demonstrate common techniques for application of complex circular external fixation devices for rare cases that are not amenable to definitive ORIF.
Indications/Contraindications
The extreme versatility of external fixation is advantageous and indicated for high-energy ankle/pilon trauma. The primary indication for utilization of an external fixation device to manage high-energy ankle/pilon trauma is an open or compromised soft tissue envelope. Generally, it is believed that for high-energy comminuted tibial pilon fracture patterns, a two-stage approach is preferred. External fixation is used to achieve osseous stability and fracture reduction while promoting healing of the soft tissues. External fixation is also indicated for fracture patterns that require or would benefit from limited internal fixation in conjunction with external fixation to avoid extensile skin incisions. Another indication of external fixation for ankle/pilon trauma is the requirement to off-load any plastic flap coverage even if internal fixation was performed. External fixation is also indicated for management of neuropathic ankle/pilon trauma and for selected geriatric patients.
Contraindications of external fixation for these types of injuries are limited. Patients with low energy rotational ankle/pilon fractures without associated soft tissue injury may better benefit from an early definitive ORIF. A delay in definitive fracture reduction of a low energy ankle fracture and/or rotational tibia fracture can be challenging to reduce if the timing for surgery has been prolonged by applying an external fixation device. For these reasons, the surgeon has to carefully assess the fracture pattern and soft tissue envelope while considering the patient’s comorbidities when deciding who will benefit from external fixation versus a single-stage ORIF.
Preoperative Considerations
Initial Fracture Reduction/Utilizing a “Spanning” External Fixator
The principles of utilizing a spanning external fixator for management of high-energy and/or open ankle/pilon trauma are to restore bone and joint alignment, to preserve the soft tissue envelope, and to prevent neurovascular compromise. Once the osseous alignment and stability are achieved with the application of a spanning external fixator, tissue perfusion and lymphatic drainage is facilitated that promotes healing of the injured soft tissue envelope. The external fixation device needs to be designed and applied in a manner that is outside the zone of injury. Strategic insertion of half-pins is positioned away from the osseous segment that may require placement of internal fixation in staged procedures. Inserting plates and screws over bone segments that had previous half-pins are avoided if possible as this may potentially serve as a nidus for infection. In addition, the external fixation device needs to be constructed to sufficiently reduce and stabilize the osseous segments while allowing adequate exposure to any wounds that may require frequent wound assessments, dressing changes, and/or staged soft tissue coverage procedures.
Internal Fixation with External Fixation for Ankle/Pilon Trauma
A common approach to the surgical management of ankle/pilon fractures is to utilize a spanning external fixator as previously described until the soft tissue edema subsides and soft tissue injuries are addressed. Once the soft tissue envelope improves, the majority of ankle/pilon fractures are surgically managed with internal fixation. This can be accomplished with limited insertion of internal fixation, standard ORIF through extensile incisions, or insertion of internal fixation with percutaneous plating (Clinical Case I).
Clinical Case I
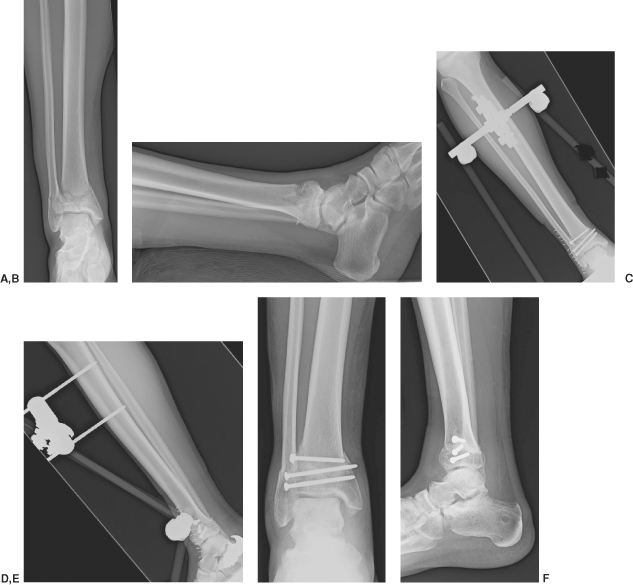
Preoperative anteriorposterior (A) and lateral (B) radiographic views of a pilon fracture that presented with fracture blisters medially over the tibia. Ten-day postoperative radiographic views (C, D) demonstrating the application of a spanning external fixator and open reduction with limited fixation through an anterior-lateral approach. The external fixator was removed at 6 weeks postoperatively and the patient was placed in a short leg cast for an additional 2 weeks and a walking boot for another 2 weeks. Final postoperative radiographic views at approximately 3 months demonstrating a well-healed tibia and fibula with anatomic alignment (E, F).
 |
Certain case scenarios benefit from internal fixation in conjunction with external fixation. This technique may be optimal when staged procedures need to be performed to reduce the tibia and the fibula, when flap coverage is performed in conjunction with internal fixation, when limited internal fixation is performed due to a poor soft tissue envelope, when geriatric ankle/pilon fractures present with poor bone quality, and in the presence of diabetic neuropathic ankle/pilon fractures (Clinical Cases II and III).
An ORIF of the fibula is usually performed only if the fracture pattern of the tibia is addressed in a staged procedure utilizing a posterior-medial, anterior, or anterior-medial
approach. In these cases, a posterior-lateral approach to fixate the fibula is performed to preserve a wide skin bridge for later planned skin incisions (Clinical Cases IV and V). If the fracture pattern needs to be addressed through an anterior-lateral or posterior-lateral approach to the tibia, the fibula is not usually addressed during the initial surgery in which the spanning external fixator was applied and is fixated in conjunction with the tibia by utilizing one extensile incision and once the soft tissue envelope permits it.
approach. In these cases, a posterior-lateral approach to fixate the fibula is performed to preserve a wide skin bridge for later planned skin incisions (Clinical Cases IV and V). If the fracture pattern needs to be addressed through an anterior-lateral or posterior-lateral approach to the tibia, the fibula is not usually addressed during the initial surgery in which the spanning external fixator was applied and is fixated in conjunction with the tibia by utilizing one extensile incision and once the soft tissue envelope permits it.
Clinical Case II
Preoperative anteroposterior (A) and lateral (B) radiographic views of a pilon fracture with significant comminution and bone loss at the metaphyseal–diaphyseal junction of the distal tibia. Two weeks postoperative radiographic views (C, D) demonstrating staged ORIF of the fibula and spanning external fixation that was performed the day of the injury. A staged ORIF of the tibia with structural allogenic fibula graft was performed 4 weeks from the date of the injury at the time the spanning external fixator was removed. A short leg cast application was applied for additional 8 weeks and a walking boot for another 6 weeks. Final postoperative radiographic views at approximately 8 months demonstrating a well-healed tibia and fibula with minimal collapse of the medial aspect of the distal tibia. Despite anatomic alignment of the joint surface, mild posttraumatic arthritic changes were already evident (E, F).
 |
Clinical Case III
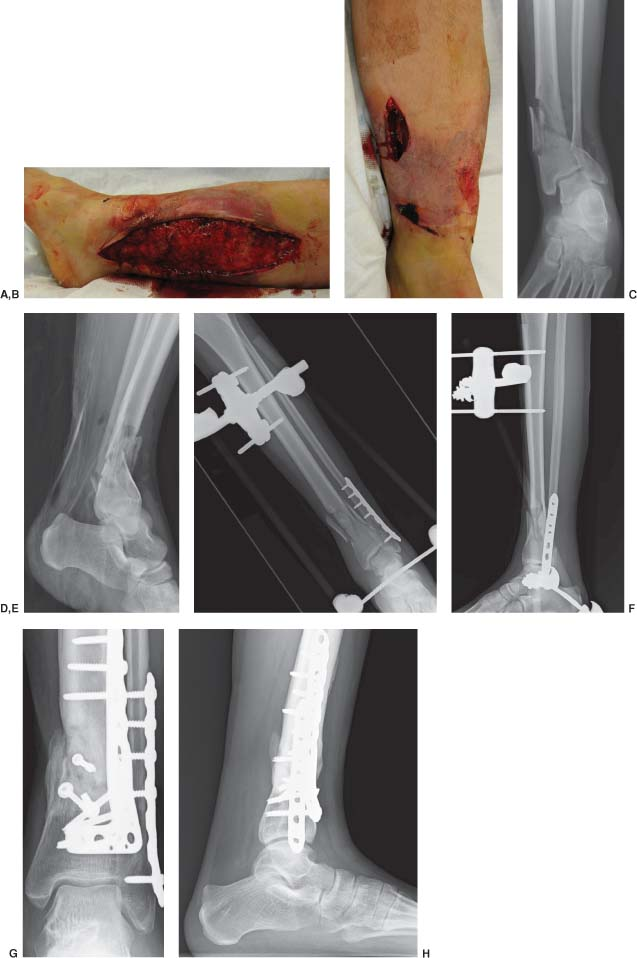
The patient originally presented with an open grade 3 distal tibia fracture and lower extremity compartment syndrome (A–D). Initial wound debridement, leg fasciotomies, and a delta-spanning external fixation was performed. Postoperative lateral radiograph showing the delayed ORIF of the fibula while maintaining the delta-spanning external fixator (E, F). Delayed ORIF of the tibia and a split thickness skin graft was finally performed to close the open fasciotomy wounds. Final postoperative radiographic views at approximately 6 months showing interval healing of the distal tibia fracture (G, H).
 |
Difficulty often arises when patients are treated for a tibial pilon fracture with an external fixator and open reduction of the fibula through a standard lateral approach and the fracture pattern requires a posterior or anterior-lateral approach to the tibia. This is commonly seen for displaced fractures of the lateral tibial plafond and posterior distal metaphysis of the tibia. Limited internal fixation of the tibia during the first surgical setting is usually avoided in contrast to the utilization of a spanning external fixation with or without fixation of the fibula.
External Fixation for Definitive Fracture Reduction
High-energy tibial pilon fractures can result in severe soft tissue compromise, neurovascular injury, compartment syndrome, and/or pulverized fracture patterns and may not always be amenable to reconstruction with internal fixation. External fixation may be the only reasonable means to achieve osseous stability and fracture reduction while permitting protective access to the soft tissue envelope. Case scenarios that require definitive fracture reduction with external fixation often require unique and variable external fixation designs that are patient and fracture pattern specific. The versatility of external fixation offers the surgeon the ability to manage difficult fracture patterns with poor soft tissue coverage.
Despite the various designs and configurations, this chapter discusses the importance of precise wire/half-pin insertion and techniques to adequately reduce the distal metaphysis to the diaphysis while restoring the alignment of the joint surface. A simple delta-spanning external fixator may be sufficient to stabilize and reduce severely comminuted tibial pilon fracture patterns through the principle of ligamentotaxis. The problems that commonly arise with a severely comminuted metaphysis of the tibia are the multiple defects of the articular surface that have little or no soft tissue attachments and cannot be reduced with ligamentotaxis. In addition, certain case scenarios do arise in which stabilization of the metaphysis and reduction to the diaphysis is not feasible through simple distraction of the ankle joint. Often, the only means of adequately reducing the metaphysis to the diaphysis requires the levering of a distal tibia external fixation ring or segment to the proximal tibia external fixation segment (Clinical Cases VI and VII).
The utilization of circular or hybrid external fixators that consist of a distal tibia ring is advantageous for these difficult high-energy fracture patterns that are not amenable to ORIF or reduction with an ankle joint–spanning external fixator. A temporary external fixator to stabilize the lower extremity may be considered first and before the definite placement of a circular external fixation is determined upon evaluation of the soft tissue
and other concomitant injuries. A computed tomography scan may be required to further determine appropriate placement of smooth wires and/or half-pins at the ankle joint level and if definitive fracture reduction with external fixation is required. Avoiding placement of circular external fixation devices at the distal tibial metaphysis to anatomically reduce severe tibial pilon fractures may also need to be considered at the first operative setting. This will allow insertion of internal fixation or other proposed methods of reduction if they were necessary in the treatment plan. In addition, if wire or pin site infections occur at the ankle joint level, a septic ankle joint can develop precluding any insertion of definitive internal fixation.
and other concomitant injuries. A computed tomography scan may be required to further determine appropriate placement of smooth wires and/or half-pins at the ankle joint level and if definitive fracture reduction with external fixation is required. Avoiding placement of circular external fixation devices at the distal tibial metaphysis to anatomically reduce severe tibial pilon fractures may also need to be considered at the first operative setting. This will allow insertion of internal fixation or other proposed methods of reduction if they were necessary in the treatment plan. In addition, if wire or pin site infections occur at the ankle joint level, a septic ankle joint can develop precluding any insertion of definitive internal fixation.
Clinical Case IV
Preoperative anteriorposterior (A) and lateral (B) radiographic views of a pilon fracture with significant comminution of the tibia plafond. Two weeks postoperative radiographic views (C, D) demonstrating ORIF of the fibula and a delta-spanning external fixator that were performed at the initial injury. Definitive ORIF of the tibia was performed at 3 weeks from the time of injury and at that time the temporary external fixator was removed. Final postoperative radiographic views at approximately 6 months showing a healed pilon fracture with good anatomic alignment (E, F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








