Stepwise Approach to Adult and Pediatric Foot and Ankle Malunions/Nonunions and External Fixation
Alexander M. Cherkashin
Mikhail L. Samchukov
John G. Birch
John J. Stapleton
Thomas Zgonis
Introduction
Management of foot and ankle deformities as a result of a malunion and/or nonunion is a clinical challenge. Most of these deformities arise from complex pathology and/or failed surgical intervention. Wound healing at the foot and ankle level is often challenging during traumatic and/or subsequent surgical procedures. Correction of severe deformities about the foot and ankle can cause devastating wound complications unless surgical measures are taken to diminish the stress and strain on the surrounding soft tissues. The utilization of internal fixation may not be feasible with a poor soft tissue envelope and contraindicated in the presence of infection. Circular external fixation is well suited for the management of complex deformities and/or bone loss with a poor soft tissue envelope and history or presence of infection. The technique of utilizing circular external fixation allows for skeletal or soft tissue correction either through acute or gradual corrections and revisional arthrodesis when indicated. Additionally, external fixation allows for percutaneous techniques, minimal incisions, or the closure of incisions without skin tension that would be present from otherwise underlying hardware. In certain complex scenarios, external fixators are utilized in conjunction with internal fixation to provide additional support to avoid hardware failure and residual deformity.
Indications/Contraindications
The ultimate surgical goal for managing these conditions is to address an ongoing infection if present, resect all nonviable bone and soft tissue, realign osseous deformities, and also provide adequate osseous stability to promote healing and regeneration of both the soft tissue and bone. The utilization of circular external fixation can be extremely helpful in addressing most midfoot and hindfoot/ankle malunions and/or nonunions and especially in the high-risk patient population.
Deciding which patients are proper candidates for revisional and reconstructive surgery with circular external fixation depends on multiple factors. Adequate discussion with the patient and patient’s family regarding the proposed surgery, risks, benefits, surgical and anesthesia complications as well as external fixation application, and estimated recovery time are required for a successful outcome. At times, patients may be more suitable to proceed with a limb amputation and prosthesis in the presence of severe local and systemic infection, multiple sites of osteomyelitis, severe peripheral vascular disease, and/or morbidly associated medical conditions.
Revisional foot and ankle surgery for these conditions is often indicated for failed open reduction and internal fixation (ORIF) cases. Breakage or loosening of retained hardware associated with an unstable or malunited fracture with pain and/or deformity is an indication for circular external fixation. The presence of infection or soft tissue loss may necessitate urgent surgery followed by staged surgical procedures to achieve functional limb salvage. Acute infections are usually managed with an initial surgical debridement and are followed by staged debridements with or without antibiotic spacers and external fixation. External fixation is indicated to stabilize an unstable fracture(s) and/or deformity and to relieve any strain on the soft tissue for subsequent closure.
The development of Charcot neuroarthropathy (CN) in diabetic patients with dense peripheral neuropathy and after failed operative fracture care is an entity that is very commonly seen among the diabetic population. Acute CN joints after failed ORIF techniques may be a limb-threatening condition especially in the presence of extensive soft tissue and bone loss. The utilization of circular external fixation may be advantageous in any stage of the previous failed surgery and help in stabilization or staged arthrodesis procedures.
Malunions and/or nonunions as a result of failed elective midfoot and hindfoot/ankle arthrodesis procedures can be successfully managed by the use of circular external fixation. In many cases, nonunions can present with a significant bone loss due to avascular necrosis or concomitant infection and osteomyelitis. Infected nonunions pose additional clinical
challenges and require staged surgical procedures with external fixation and before performing a definitive arthrodesis.
challenges and require staged surgical procedures with external fixation and before performing a definitive arthrodesis.
Circular external fixation is also beneficial in managing neuromuscular and paralytic malunions and/or nonunions. The residual deformities can be acutely or gradually corrected with external fixation and may be converted to an arthrodesis once alignment is achieved. Certain neuromuscular or paralytic hindfoot/ankle deformities can be corrected with a total talectomy, tibiocalcaneal arthrodesis, and circular external fixation. Bone grafting or bone transport procedures may also be necessary to address for the bone loss and/or limb length discrepancy in any malunion or nonunion case if acute compression is not possible.
Preoperative Considerations
Important factors that need to be considered in the preoperative period include and are not limited to patient’s age, ambulatory status, multiple comorbidities, noncompliance with treatment, severity and progressiveness of deformity, and associated compensatory and joint contractures. Deformity analysis is paramount when managing these conditions and each case may require a different surgical approach and treatment. A thorough history and physical examination along with pertinent laboratory, radiographic, neurologic testing, and medical imaging are necessary before the surgical reconstruction. Vascular studies may also be necessary in the diabetic population or in patients with chronic smoking history and peripheral arterial disease. At times, with severe foot and ankle contractures the topography of the vascular structures may be displaced secondary to multiplane deformities. Preoperative Doppler signals and skin markings if needed can address such anatomic variations in order to avoid any potential vascular injury. Appropriate medical and anesthesiology consultations are equally important during the preoperative period.
Additional complicating factors such as segmental bone loss, avascular segments of bone, infected bone with or without previous hardware also need to be considered. Segmental bone loss is evaluated in order to determine if structural or nonstructural bone grafting will suffice or if bone transport may be required. In addition, patients with long-standing malunions and/or nonunions may also present with associated painful hip and knee contractures, limb length discrepancies, neuralgia, and a poor soft tissue envelope that require consideration before any revisional surgery.
A thorough musculoskeletal examination of the entire lower extremity combined with radiographic imaging is necessary for defining the associated deformity. Computed tomography is useful to evaluate nonunions, degenerative joints, and multiplane deformities about the midfoot and hindfoot/ankle. Magnetic resonance imaging and nuclear imaging are beneficial in cases of osteomyelitis and/or in addition to the intraoperative bone biopsy and culture results.
Select osteotomies, arthrodesis procedures, ligamentous reconstruction, tendon lengthening, transfer or release are some of the major reconstructive options to address these complex conditions. The choice of opening or closing wedge- and dome-shaped osteotomies are based on the plane of deformity and associated length of the osseous segments in consideration with the surrounding neurovascular structures and soft tissue envelope at risk.
Planning for external fixation surgery is important not only in preparation for the treatment process, but as an important step in preventing and reducing possible complications. Acute correction of the deformity is always preferable, but cannot always be performed. If a distal tibial deformity is present, preoperative planning should evaluate the amount and level of the deformity in order to accurately position the external fixation hinges. The selected level of osteotomy should be at or close to the level of deformity. When a tibial deformity is located too distally, it becomes quite challenging to perform the osteotomy at the deformity level. In these cases, the external fixation hinges are placed at the level of deformity and the proposed osteotomy is performed at approximately 1.5 to 2 cm above the distal tibial fixation segment. In these case scenarios, translation at the osteotomy site must be considered. In other cases, a distal tibial dome osteotomy can be performed in order to minimize the effect of translation. If a tibial lengthening is intended, it is usually better to perform it through a separate proximal tibial osteotomy. Performing a proximal distraction osteogenesis is preferred in these cases in order to promote improved vascularity to the bone segments and to decrease the total time of the external fixator.
A pre-built external fixation device is always preferable if possible and can be tried on the patient as a part of the preoperative patient and family education process. This method can help the patient in understanding of the postoperative process and can also improve patient compliance. Preoperative external fixation assembly saves time in surgery, allows for additional validation of the treatment plan, and also assures that the external fixation hinges and angular distractors are functional. If this entire process is not feasible, it is highly recommended to pre-build the proposed circular external fixator in the operating room before inserting the necessary transosseous wires and half-pins. Circular external fixation pre-assembly helps to construct the external fixator according to existing deformities and allows using it as a template for transosseous wire and half-pin insertion.
Detailed Surgical Technique
Realignment Hindfoot/Ankle Osteotomies and Arthrodesis Procedures
Corrective osteotomy and/or joint resection combined with or without hindfoot/ankle arthrodesis can be achieved acutely or gradually with external fixation. The specific advantage of external fixation is that adjustments throughout the postoperative period can be performed to achieve the desired alignment.
The ability to deliberately translate the bone ends to achieve the desired alignment is critical. For this reason, the type of osteotomy or joint resection performed has to consider the shape of the deformed bone ends to permit translation while creating two stable bone surfaces to allow successful bone healing. Poor bone quality surrounding the pathologic entity may be a limiting factor where the corrective osteotomy may require placement at a different location to avoid the potential for nonunion. In certain scenarios where the osteotomy and/or joint resection are necessary to be performed at the pathologic site, bone grafting either initially if an acute correction
is performed or in delayed fashion for gradual correction will need to be considered.
is performed or in delayed fashion for gradual correction will need to be considered.
Anatomic alignment can be performed acutely and stabilized with temporary fixation until the external fixator is utilized or the external fixator can be partially assembled prior to the osteotomy and/or joint resection and then completed at the end of the procedure for the process of gradual deformity correction. For gradual corrections, the circular external fixator may be applied initially to mimic the associated deformity and gradually adjust it to a neutral position correcting the deformity.
For supramalleolar osteotomies, the proximal external fixation segment consists of two tibial rings “tibial block” and the foot plate along with a circular ring at the distal level of the tibial metaphysis are placed. The osteotomy can then be carried out with low-energy techniques to divide the bone. Such osteotomy can be performed with osteotome, multiple drill holes and osteotome, or with a Gigli saw. A combination of multiple drill holes with an oscillating drill bit and an osteotome to complete the osteotomy is usually preferred. After completion of the osteotomy, the surgeon can manipulate the distal external fixation segment consisting of the tibial ring and the foot plate while stabilizing the tibial block to ensure that the bone is osteotomized. The circular external fixator is then assembled around the osteotomy with hinges and/or motors for a traditional Ilizarov technique or by utilizing the dynamic strut constructs of the Taylor spatial frame (TSF). The TSF application becomes advantageous when translation and rotation needs to be performed in addition to multi-level angular corrections. Gradual corrections are usually performed approximately 7 to 10 days following the osteotomy with a recommended maximum distraction of 1 mm/day when indicated (Chapter 15).
Joint arthrodesis can be performed by applying uniform compression with the external fixator after anatomical osseous alignment and adequate joint preparation has been achieved. Articular joint surfaces need adequate resection and joint microfracturing with an osteotome or pre-drilling may help induce vascular ingrowth at the arthrodesis site. Joint compression arthrodesis can then be performed with a static circular external fixator or a TSF construct (Clinical Cases I–V).
Realignment Midfoot Osteotomies and Arthrodesis Procedures
Severe midfoot deformities that require correction with circular external fixation are often a result of malunion from high-energy trauma or from conditions such as CN. High-energy trauma and/or the development of CN after a midfoot fracture can result in severe malunion and/or nonunion that are associated with axial, sagittal, and horizontal plane deformities.
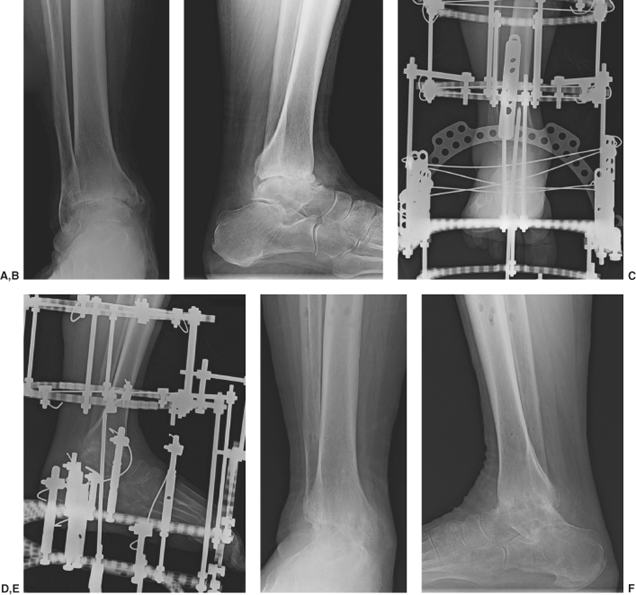
Clinical Case I
Preoperative anteroposterior (A) and lateral (B) radiographic right ankle views demonstrating posttraumatic arthritis of the ankle and subtalar joint that resulted from a malunion of a talus fracture. Patient underwent a tibiotalocalcaneal arthrodesis with a circular external fixation (C, D). The external fixator was removed at approximately 10 weeks. The patient was kept in a non–weight bearing cast for about 2 weeks with an additional weight bearing cast for another 4 weeks. Final radiographic views at 6-month follow-up showing successful alignment and union at the ankle and subtalar joints (E, F).
 |
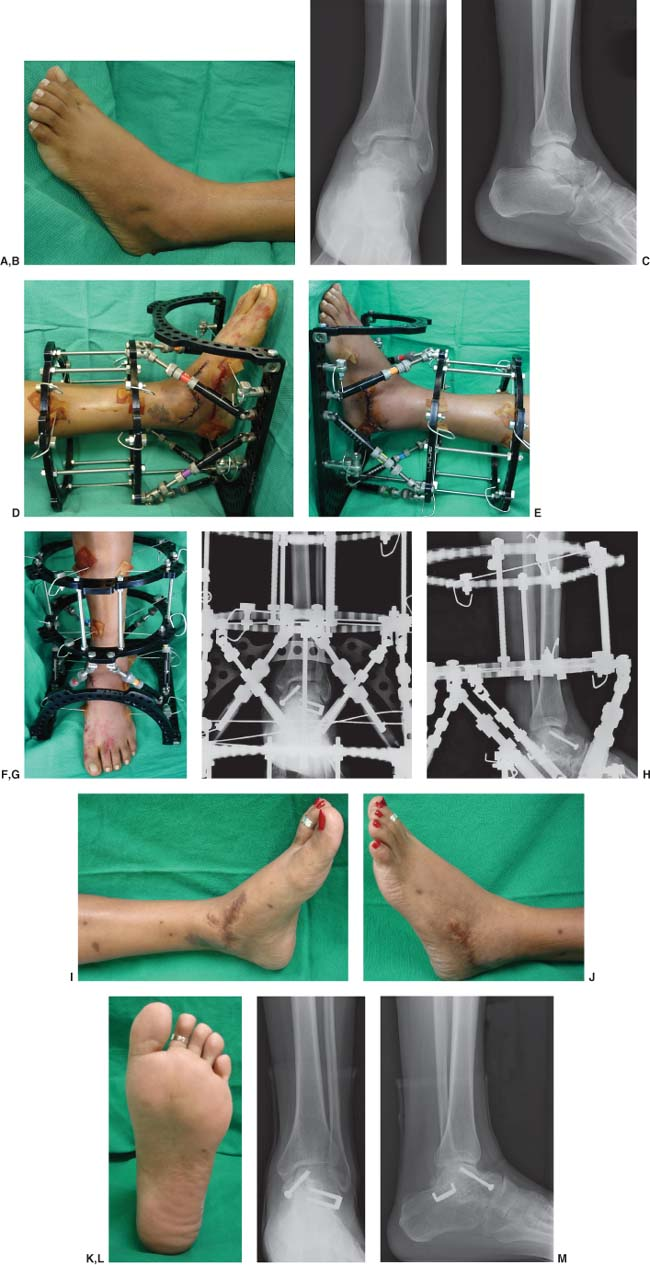
Clinical Case II
Preoperative clinical (A) and radiographic (B, C) views of a talar neck and body fracture with a severe malunion and deformity. Patient underwent an osteotomy and acute correction of the talus fracture with a primary subtalar joint arthrodesis and an application of a Taylor spatial frame for deformity and equinus correction (D–H). The external fixator was removed at approximately 8 weeks where a postoperative wound dehiscence was addressed. Final clinical (I–K) and radiographic (L, M) views at approximately 1-year follow-up.
 |
Clinical Case III
Preoperative radiographic views (A–C) demonstrating a severe talar varus malunion with avascular necrosis after a talus fracture/dislocation in a morbidly obese patient. Patient underwent re-alignment and pantalar arthrodesis with internal and circular external fixation (D, E). The external fixator was removed at approximately 12 weeks. The patient was kept in a non–weight bearing cast for about 2 weeks with an additional weight bearing cast for another 4 weeks. Final radiographic views at 2-year follow-up showing successful alignment and union at the pantalar arthrodesis (F–H).
 |
These types of deformities may require a tri-plane wedge resection across the entire midfoot or an osteotomy with gradual correction. Gradual midfoot correction may be beneficial in severe cases of rotational valgus and/or varus deformities. In cases of a midfoot wedge resection, preoperative planning based on weight bearing radiographs will determine the apex of the deformity and template for the osteotomy. Intraoperative guide wires may also be used along the bone segments of the proposed osteotomy in order to ensure correct positioning under the guidance of C-arm fluoroscopy. The osteotomy is usually performed with a large oscillating saw and/or osteotome. After the resected wedge of bone is removed, anatomic alignment is performed acutely and temporarily stabilized with two or more Steinmann pins. The circular external fixator can now be applied to stabilize and compress the midfoot osteotomy.
The foot and ankle positioning within the circular external fixator is paramount when applying the tibia rings and calcaneal fixation which are attached to the foot plate. It is important to establish a neutral ankle position in the sagittal plane as equinus positioning will lead to detrimental forces through the midfoot once the external fixator is removed. Proximal to the midfoot osteotomy or arthrodesis, a midfoot and/or talar transosseous wire can be inserted in order to stabilize the midfoot and hindfoot. Additional smooth transosseous wires are then inserted across the midfoot and/or forefoot.
The smooth wire distal to the osteotomy is then bent proximally about two to three holes on the foot plate. The surgeon and an assistant can then simultaneously straighten the wire by utilizing the pre-bent wire technique or dynamic tensiometers. This will provide equal compression across the osteotomy and arthrodesis site. Other common alternatives to compress a midfoot osteotomy
consist of a tibial block combined with a separate calcaneal half-ring and a full forefoot circular ring. This construct allows the insertion of multiple transosseous wires for stabilization of the midfoot osteotomy or correction of severe rotational midfoot and/or hindfoot deformities (Clinical Case VI).
consist of a tibial block combined with a separate calcaneal half-ring and a full forefoot circular ring. This construct allows the insertion of multiple transosseous wires for stabilization of the midfoot osteotomy or correction of severe rotational midfoot and/or hindfoot deformities (Clinical Case VI).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








