Abstract
Spinal fractures in patients with ankylosing spondylitis may be the result of minor trauma. These fractures may lead to severe neurological deficits, and they are difficult to detect using standard radiography. Often, CT-scans and MRI are required for diagnosis.
Résumé
Les fractures rachidiennes dans la spondylarthrite ankylosante apparaissent dans le cadre de traumatismes mineurs. Elles sont à l’origine de complications neurologiques particulièrement graves. Leur reconnaissance est souvent difficile sur les clichés standard et nécessite le recours au scanner et à l’IRM.
1
English version
1.1
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory rheumatic disease, which, if not treated appropriately, exposes patients to syndesmophyte formation and spinal deformation. The natural evolution of AS leads to a rarefaction of the osseous trabeculation in vertebral bodies and diffuse spinal stiffness. Rather than strengthening the spine, this diffuse stiffness exposes the spine to risks of transdiscal fractures, and more rarely, transcorporeal factures, that may be the result of minor trauma that sometimes goes undetected . These fractures can sometimes lead to severe neurological injuries, signaling the evolution of the disease . Our objective is to reiterate, through this case report, the advantages of diagnosing these fractures early on, thus permitting early and appropriate treatment of the patient.
1.2
Observation
A 70-year-old patient had been monitored for AS for 40 years. When diagnosed, the patient had a total seven out of 12 points according to the Amor criteria (1990) for spondyloarthropathy: inflammatory lower back pain, left-right alternating pain in the buttocks and grade-4 bilateral sacroiliitis, with an improvement in less than 48 hours when treated with nonsteroidal anti-inflammatory drugs (NSAIDs). This patient was hospitalized for a mixed-type left sciatica of the L5 vertebra, associated with radicular claudication, that had limited the patient’s walking perimeter to 50 m for 6 months, without vesicosphincterian disorders. This situation was the result of the patient falling and landing on his back.
The clinical exam showed a cervical vertebra limited in all planes, exaggerated dorsal kyphosis, 2 cm chest expansion, lumbar spine stiffness with a Schöber index of 0.5 cm, and a positive Lasegue’s sign of 60° on the left side. The neurological exam did not reveal any sensory motor disorders or anomalies of osteotendinous reflexes. Blood tests showed a sedimentation rate of 45 mm in the first hour and a C-reactive protein (CRP) level of 11 mg/l.
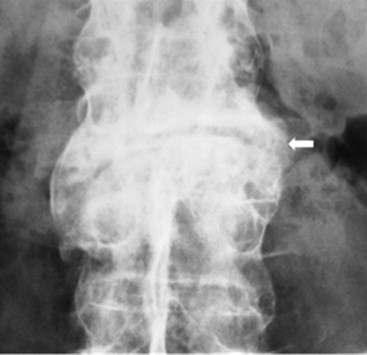
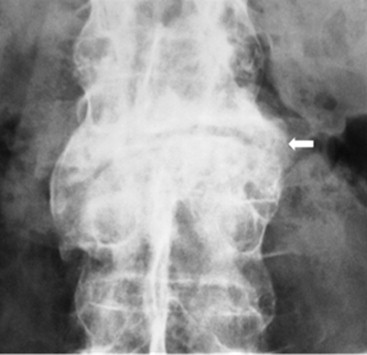
Standard X-rays revealed a bamboo spine at the level of the lumbar vertebrae, with a visible fracture line in the L4 vertebra and the L3-L4 disc (see Fig. 1 for the reconstructed images), grade-4 bilateral sacroiliitis, and bone demineralization. The bone mineral density (BMD) results revealed osteopenia. A lumbar CT-scan confirmed the presence of a transcorporeal and transdiscal bony solution of continuity in the L4 vertebra and the L3-L4 disc with significant corporeal bone restructuration extending towards the posterior arc ( Fig. 2 A and B). This had the effect of narrowing the central spinal canal, and was associated with staged disc calcification, interspinal ligaments, yellow ligaments, staged syndesmophytes, and the absence of pathological contrast in the perivertebral soft tissue after a contrast agent had been injected.
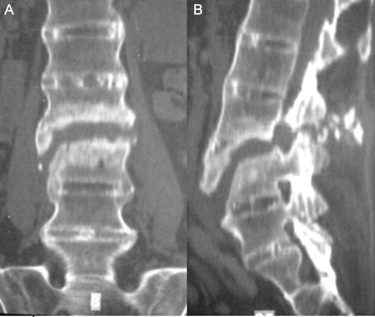
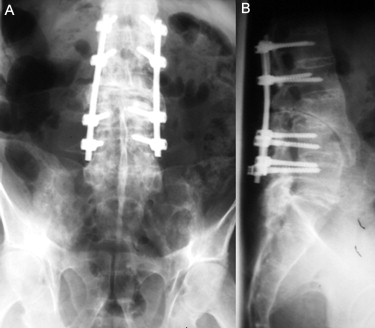
Since there were no neurological complications and the MRI revealed signs of a fracture with pseudarthrosis, surgery was not chosen. The patient was prescribed analgesics, NSAIDs, corticotherapy (prednisone 30 mg per day), and a thermoplastic (Néofract) corset. The condition evolved into persistent left sciatica of the L5 vertebra with claudication, which became hyperalgesic. This situation led to surgery, consisting of a posterior fusion of L1 to L5 using four screws and two rods associated with a posterior bone graft from the right posterior iliac crest ( Fig. 3 A and B). The immediate postoperatory effects were simple. The condition evolved toward persistent pain in the left crural nerve, which improved when treated with analgesics and NSAIDs. There were no neurological deficits, and the fracture was healed 14 months after the operation.
1.3
Discussion
The incidence of spinal fracture in patients with AS is difficult to evaluate. It varies according to the author: eight cases in 5 years for Murray and Persellin , one out of 300 cases for Hannequin et al. and 61 out of 1071 cases for Feldtkeller et al., among which 15 cases occurred without any trauma . Most fractures occur in severe cases of AS with a completely ankylosed spine at an average age of 50 . The risk of fracture following trauma increases with the time since the AS diagnosis , occurring an average of 20 years after the onset on the disease. The vertebral fractures occur more frequently in cases of AS with peripheral involvement than in cases with isolated axial involvement .
AS increases the risk of vertebral fractures, unlike extravertebral fractures, which AS doesn’t influence at all . In fact, spinal fractures in patients with AS are equivalent to those in osteoporotic long bones . Spinal fractures can occur after minor trauma or even without any trauma . This observation underlines the importance of systematically searching for fractures in cases of AS with even minor trauma or when faced with a recent exacerbation of spinal pain . These fractures are cervical in 75% of the cases , dorsal in 15% of the cases and lumbar in 10 to 15% of the cases . The cervical fractures predominate at the lower levels, from C5 to C7 in 72% of the cases . The dorsal fractures occur most frequently in the T6 to T12 vertebrae; likewise, the lumbar fractures occur most frequently at the level of the L4-L5 intervertebral disc .
Pathophysiologically, hyperextension injuries are the most common and the most dangerous . The ankylosed spine fractures similar to a long bone . The factors that influence the occurrence of a transdiscal fracture are: (1) a moderately osteoporotic spine whose discs are partially ossified and (2) a hyperextension injury . In contrast, transcorporeal fractures are influenced by: (1) an extremely osteoporotic spine whose discs are completely ossified and (2) a hyperflexion injury . The type of fracture most often encountered is the horizontal transdiscal fracture (59 to 77.5% of the cases). The solution of continuity concerns the disc and the syndesmophytes, and often extends to the posterior arc . Elsewhere, the fractures are corporeal . More rarely, the fractures concern only the posterior arc or only one syndesmophyte . Fractures at several levels are seldom reported .
The neurological complications observed in cases of spinal fractures in patients with AS are characterized by their high frequency (69 to 75%) and their severity, which is related to their high instability . They are frequently observed in cases of fractures of the three spinal columns (84 to 91% of the cases) . A spinal cord injury was detected in 47% of the cases, and was found alongside a cervical spine fracture in 88% of the cases . The neurological deficit can be acute or delayed , and is correlated to the secondary spinal cord trauma extending as far as contusion, compression or section . Spinal cord compression can be generated by a slipped disc, an avulsion fracture or an epidural hematoma .
Spinal fractures in AS patients can be difficult to identify with standard X-rays due to spinal ossification, osteoporosis, minor fracture displacement , poor visibility of the disc spaces and the difficulty of exploring certain regions of the spine, especially the cervicothoracic region . The diagnosis of this type of fracture is facilitated by performing a CT-scan (using 3D multiplanar reconstructions) and an MRI . Some authors recommend using a multidetector CT-scan machine with multiplanar reconstruction for detecting occult fractures .
The advantages of using MRI lie in their ability to evaluate fracture and pseudoarthrosis complications, ligament and soft tissue injuries, and medullary repercussions . In fact, MRI help to detect the signal anomalies from the posterior column, which, when associated with discal and corporeal anomalies, play a key role in diagnosing this kind of fracture . The main advantage of using MRI is that it helps to assess the spinal canal and its contents since spinal fractures, which are quite unstable, can lead to very serious neurological complications . However, MRI also has limitations: for example, limited visualization and interpretation of bone splinters and the interference caused by the metal artifacts . Moreover, it is important to point out that, for patients with advanced AS who have a vertebral deformation (e.g., the cervical spine blocked in hyperflexion), it would be unrealistic to attempt to perform a CT-scan or an MRI .
Whether surgical or orthopedic, the treatment is determined in terms of the stability of the fracture and the existence of neurological signs . The indications for surgical treatment are vertebral instability or the existence of neurological complications . Surgery is used to stabilize the spine using an anterior and/or posterior fixation .
The treatment of fractures-dislocations of the cervical spine in patients with AS is particularly difficult . These injuries typically concern the anterior and posterior elements of the vertebrae; they generate major spinal instability and are frequently responsible for neurological deficits . Surgical treatment is made difficult by the rigidity of the spine and the osteoporosis that is often associated . Different treatment strategies have been proposed in the literature, including anterior, posterior or combined anterior-posterior fixation, associated or not with various methods of external immobilization . Regular X-ray monitoring is needed to confirm that the injuries have healed .
Postoperative monitoring of patients with an initial neurological complication has shown an improvement with respect to the patient’s neurological deficits in 88% of the cases and post-surgery stabilization in 12% of the cases . Extreme prudence is required when moving the patient due to the risk of displacing the fracture site . Patient education in terms of the fragility of their spine and the need to avoid even minor trauma is key to preventing spinal fractures in patients with AS .
1.4
Conclusion
Spinal fractures in patients with AS have their own characteristics. Rheumatologists, rehabilitation specialists and radiologists must know these characteristics and look for them in patients whose pain symptoms change, even without trauma. The potential for serious neurological complications justifies the use of CT-scans and/or MRI to remedy the deficiencies of standard X-rays.
Conflicts of interest statement
No conflicts of interest.
2
Version française
2.1
Introduction
La spondylarthrite ankylosante (SA) est un rhumatisme inflammatoire chronique, exposant en l’absence de prise en charge adéquate à la formation de syndesmophytes et l’installation de déformation vertébrale. L’évolution naturelle de la SA aboutit à une raréfaction de la trabéculation osseuse des corps vertébraux et à une raideur diffuse du rachis. Cette dernière, loin de le consolider, l’expose à un risque de fracture transdiscale et plus rarement transcorporéale apparaissant dans le cadre de traumatismes mineurs passés parfois inaperçus . Ces lésions fracturaires peuvent se compliquer de lésions neurologiques parfois gravissimes, marquant un tournant évolutif de la maladie . Il s’agit donc de rappeler, à travers une observation, l’intérêt du diagnostic de ces lésions, permettant une prise en charge précoce et adaptée du patient.
2.2
Observation
Il s’agit d’un patient âgé de 70 ans, suivi depuis 40 ans pour une SA dont le diagnostic a été retenu devant des lombalgies inflammatoires, une douleur fessière à bascule, une sacroiliite bilatérale stade 4 et l’amélioration sous anti-inflammatoires non stéroïdiens (AINS) en moins de 48 heures, soit un total de sept points selon les critères d’Amor de 1990. Il a été hospitalisé pour une lombosciatique de trajet L5 gauche de type mixte associée à une claudication radiculaire avec limitation du périmètre de marche à 50 m évoluant depuis six mois, sans troubles vésicosphinctériens, apparue suite à une chute de sa propre hauteur avec réception sur le dos. L’examen clinique a montré un rachis cervical limité dans tous les plans, une exagération de la cyphose dorsale, une ampliation thoracique à 2 cm, une raideur du rachis lombaire avec un indice de Schöber à 0,5 cm, un signe de Lasègue positif à gauche à 60̊. L’examen neurologique n’a pas mis en évidence de déficit sensitivomoteur, ni d’anomalies des réflexes ostéotendineux. La biologie a montré une vitesse de sédimentation à 45 mm à la première heure et une C-réactive protéine (CRP) à 11 mg/L. Les radiographies standard ont mis en évidence un aspect de colonne bambou au rachis lombaire avec visualisation d’un trait de fracture intéressant le corps vertébral de L4 et le disque L3-L4 avec des images de reconstruction ( Fig. 1 ), la présence d’une sacroiliite bilatérale stade 4 et d’une déminéralisation osseuse. L’ostéodensitométrie a révélé une ostéopénie. La tomodensitométrie (TDM) lombaire a confirmé la présence d’une solution de continuité osseuse transcorporéale et discale intéressant le corps vertébral de L4 et le disque L3-L4 avec importants remaniements osseux corporéaux et de l’arc postérieur ( Fig. 2A et B ), rétrécissant le canal central en regard, associée à des calcifications discales étagées, des ligaments interépineux et des ligaments jaunes, des syndesmophytes étagés et l’absence de prise de contraste pathologique des parties molles périvertébrales après injection de produit de contraste. Devant l’absence de complications neurologiques et les signes d’une fracture au stade de pseudarthrose à l’imagerie, l’indication chirurgicale n’a pas été portée et le patient a été mis sous antalgiques, AINS, corticothérapie (prednisone) à la dose de 30 mg/j, en plus de la prescription d’un corset en néofract. L’évolution s’est faite vers la persistance de la lombosciatique L5 gauche claudicante devenue hyperalgique, ayant amené à réaliser un traitement chirurgical consistant en une synthèse postérieure de L1 à L5 par quatre vis et deux tiges, associée à une greffe postérieure à partir de la crête iliaque postérieure droite ( Fig. 3A et B ). Les suites opératoires immédiates étaient simples. L’évolution s’est faite vers la persistance d’une cruralgie gauche améliorée sous traitement antalgiques et AINS, l’absence de déficit neurologique et la consolidation de la fracture au bout de 14 mois après l’intervention.