Spine
History
Question the athlete and witnesses of injury. Study the videotape if available in acute injury.
Understand the demands of sport, exercise, and occupation.
Pain
Character.
Location and radiation.
Relationship to exercise or activity.
Alleviating or relieving factors.
Neurological symptoms
Numbness, pins and needles.
Weakness.
Past history
Spinal problems.
Orthopaedic problems.
Family history
Spinal problems.
Some signposts to the aetiology include: medical (insidious and persistent, worse in morning), mechanical (intermittent and associated with activity), disc herniation and nerve impingement (radiates to lower leg or foot), tumour (night pain), relief from aspirin (osteoid osteoma).
Problems that show familial predisposition: disc disease, ankylolising spondylitis, Reiter’s syndrome, other spondylolarthropathies.
Red flags in history of patient with back pain
Require consideration of pathology that might be life-threatening or require urgent intervention:
Less than 10yrs of age.
First episode of back pain and over 60yrs old.
Unexplained weight loss.
Chronic cough.
Night pain.
Inter-menstrual bleeding.
Altered bowel function.
Altered bladder control.
Visual disturbance, balance problems, upper limb dysaesthesias.
Past history of cancer or corticosteroid use.
Bilateral weakness of lower extremities.
Examination
Inspection
With patient standing
From behind: check level of shoulders, lateral curvature/scoliosis, normal alignment, lengths of lower limbs (level of posterior superior iliac spines), or hair tufts over spine.
From side: check increased kyphosis, decreased lordosis.
NB Scoliosis may be due to unilateral muscle spasm, or nerve root irritation due to disc herniation.
Palpation
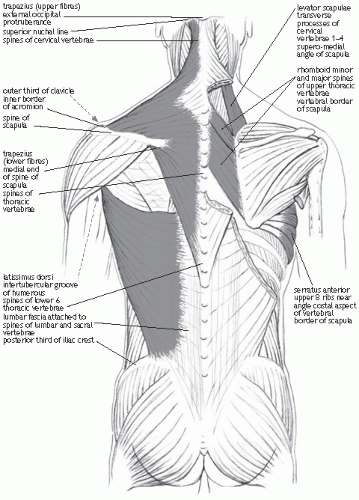
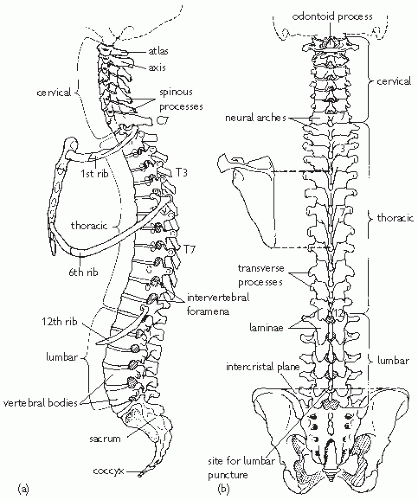
Palpate each spinous process, sacroiliac joints, facet joints for tenderness, muscle spasm, and consider the anatomy (Figs. 16.1 and 16.2).
Active and passive movement
Restriction of spinal movement may be due to muscle spasm as a result of pathology in one or more functional unit. Note pain during any of the movements tested.
Lumbar flexion (normal 40° to 60°) occurs by reversing the lordosis. During re-extension the lumbar lordosis is regained in the final 45°. NB Toe touching with straight legs is influenced by hip mobility, hamstring tightness—so not useful. However, this may be confirmed by measuring the increased distance between marked points over the spinous processes with flexion (Schrober’s test).
Lumbar extension (normal 20-30°) is painful with facet joint or pars interarticularis pathology—called ‘posterior element pain’. This can be due to posterior disc pathology or closing of the foramen of nerve roots.
Lumbar lateral flexion (normal 20°) is painful with ipsilateral facet joint pathology or lateral disc protrusion (radicular pain), but is often a non-specific sign.
Lumbar rotation occurs with thoracic rotation (normal 90°) and is assessed with pelvis and hips fixed (held by examiner or sitting).
Neurological examination
Sensory: light touch over back and abdomen, legs, perianal sensation.
Lower limb reflexes (L4 knee, S1 ankle), superficial anal reflex: touching perianal skin causes contraction of sphincter and external anal muscles (S2, S3, and S4).
Motor: squat and return to standing, walk on heels (weak ankle dorsiflexors exposed—L4) and then toes (weak triceps sura exposed—L5). Muscle strength testing for nerve root assessment (L1—hip flexion, L2—hip flexion, L3—knee extension, L4—foot dorsiflexion, L5—hallus extension, foot eversion, S1—knee flexion and foot plantar flexion). Sphincter tone and contractility.
Special tests
Sciatic and femoral nerve tension tests
Principle
Stretching the dura and nerve root to produce leg pain. Positive will produce the patient’s radicular symptoms.
Sciatic nerve tests
Straight leg raise.
Lasegue test: patient supine with hips flexed to 90°. Knee slowly extended.
Bowstring sign: examiner presses in popliteal fossa and causes increased pain in leg.
Slump test: patient sits ‘slumped’. Progressive increase in tension by flexing neck, extending knee, and dorsiflexing foot.
Notes
Ankle dorsiflexion and neck flexion should aggravate radicular pain or decrease angle of straight leg raise.
False positive: pain with less than 30° of straight leg raise (SLR), production of back pain with no leg pain.
Femoral nerve test
Prone
Knee flexed to 90° and hip extended—a positive test is recorded if there is pain in the thigh with hip extension.
One-legged hyperextension and Fitch test
In those with posterior element pathology, pain is reproduced in the back when the patient hyperextends, while standing on one leg. The Fitch test includes rotation, as well as one-legged hyperextension and may be more sensitive.
Gillet test of sacro-iliac joint
Examiner places thumb on PSIS and the other thumb on the midline of sacrum at similar level in standing patient. They observe the relative movements of the thumbs as the patient flexes the hip more than 90°. The inominate bone is expected to rotate posteriorly and, hence, the thumb on PSIS should move caudally. The contralateral inominate movement can also be assessed and should not move caudally.
Schrober’s Test
A mark is made at the level of the posterior iliac spine on the vertebral column (level of L5). The examiner places one finger 5cm below this mark and another finger 10cm above the mark. The patient is then instructed to touch his toes. If the increase in distance between the two fingers on the patients spine is less than 5cm then this indicates restricted lumbar flexion.
Investigations
Guided by history and examination
General problem—degenerative changes appear in asymptomatic from early age.
X-rays
Routine AP and lateral specialized oblique.
Advantages cheap, low radiation dose, define bones.
Disadvantages do not define soft tissues.
AP—check spinous process, 2 transverse processes, 2 pedicles, 2 laminae, and 2 facet joints (vertical in lumbar spine) at each level, assess alignment.
Lateral—see bodies of vertebrae, disc spacing increasing from L1-L4, lumbar intervertebral foraminae alignment will give smooth curve of posterior aspects of the bodies forming the lumbar lordosis.
Oblique—for facets joints and pars interarticularis.
See ‘Scottie Dog’—neck is pars, nose is transverse process, eye is pedicle, ear is superior articular process, front legs are inferior articular process. Collar = spondylolysis.
Bone scan
Technetium-labelled injection is taken up in areas of increased osteoblastic activity demonstrating increased metabolic activity in bone. Detected by gamma camera. Reveals stress fractures (i.e. spondylolysis), but also epiphyses and metaphyseal bone plates of young.
Advantage: high sensitivity.
Disadvantage: low specificity, radiation dose.
Single photon emission computer tomography (SPECT)
Gives more precise anatomical localization of ‘hot spot’ than bone scan.
Use to locate spondylolysis.
Computer tomography
Allows visualization of bony configuration and good visualization of paraspinal soft tissues.
Advantage: good to detect fractures and impingement of spinal canal, evaluate spinal tumours.
Disadvantages: radiation dose, slices may miss pathology.
Myelography
An injection of radio-opaque dye into the spinal canal reveals an outline of the spinal cord and nerve roots on subsequent plain X-rays. This can reveal nerve root compression, though not its cause (i.e. prolapsed disc, osteophyte or tumour).
Magnetic resonance imaging
Provides excellent visualization of soft tissues—including discs.
Can assess impingement of nerve roots.
May see haemorrhage from ligamentous injury.
Can detect atrophy in paraspinal muscles.
Detects changes in the spinal cord, such as syringomyelia.
Advantage—no radiation.
Disadvantage—cost.
Discography
Injection of radiopaque dye into the disc space under pressure—pain response assessed.
Acute spinal injury
History and examination
Consider forces involved and take history from the patient and witnesses. Review video if available.
Examine carefully to exclude injuries that could produce instability (threaten neurological structures).
Immobilizing the spine
Though ‘airway’ is a priority in an unconscious player, the cervical spine should be protected by employing a jaw thrust in preference to the head tilt-chin lift maneouvre. Inadequate immobilization in transporting player from pitch could worsen clinical condition!
When to immobilize?
Pain in spine secondary to high velocity injury.
Any neurological signs.
Severe spinal pain (for comfort).
Transportation should be on a spinal board by trained personnel to ensure immobilization in position athlete was found. In general, equipment such as helmets should only be removed by those trained to do so.
Cervical spine injury and potential instability should be presumed in anyone who is unconscious after head injury. The cervical spine will need assessment by cervical spine X-ray and CT of entire neck.
Acute injuries of the back in sport
Muscular strains (see Fig 16.1).
Ligamentous sprains.
Contusions.
Fractures: transverse processes, ribs (NB beware renal injury with injury at costovertebral angle—assess abdominal tenderness and haematuria and consider intravenous pyelogram or renal ultrasound) posterior elements—generally stable and not associated with neurological damage.
Compression fractures of the vertebral bodies: unless trauma was extreme, are usually pathological (i.e. often osteoporotic in elderly athletes).
Fracture dislocations: high-energy injuries (e.g. diving, car racing) with high risk of spinal cord injury.
Thoracic disc herniation: occurs occasionally in athletes, as in the general population (1.6 per 1000), but is not associated with athletic activities— lateral herniation presents with chest wall pain in dermatomal pattern and central herniation with lower extremity spasticity and paraparesis.
Lumbar disc disease.
Management of musculoligamentous injuries of the back
Sprains and strains of the back are common. They do not require radiological evaluation if the clinical findings do not indicate other causes. Cold therapy should be used for 48-72h and muscle spasm may be controlled by anti-spasmodics. Rehabilitation is important and aims to restore normal muscle strength and firing patterns. Tight muscles, typically hamstrings and hip flexors, may need to be stretched to prevent recurrence.
Disc disease
Disc disease is a continuum from degeneration to herniation. There is a loss of water content with age and this permits more stress to be transferred to the annulus fibrosis, which may develop radial tears. These have the potential for herniation,
Disc degeneration
A desiccated disc with tears may give local pain.
History
Pain often precedes activity, but may be aggravated by it.
Findings may be similar to central musculoligamentous injuries.
Investigations
Not indicated in most minor cases. However:
Plain radiographs may show loss of disc height in advanced cases and there may be associated facet joint arthrosis.
MRI reveals loss of disc water content, small disc bulges, and annular tears.
Treatment
Medication: adequate analgesia and anti-spasmodics.
Ice: provides an analgesic effect.
Heat: improved mobility.
Rehabilitation to improve muscle strength and firing to decrease the load on the disc.
Address hamstring or hip flexor tightness
Intradiscal electrothermal annuloplasty (IDET)—if tears are apparent in the disc, thermal coaglulation has been achieved by a probe inserted into the disc. The benefits of this treatment are not yet proven.
Disc herniation
In disc herniation (or ‘slipped disc’), the nucleus pulposis extrudes through a tear in the annulus fibrosis most commonly at L4/L5 and L5/S1. They occur most often in the 5th decade of life, although up to 2% occur in those under 18yrs. Such herniation may press on the nerve root causing leg pain (called ‘sciatica’), numbness and weakness. Pain may also be generated by the release of inflammatory molecules (e.g. tumour necrosis factor-alpha) and is known as ‘chemical radiculitis’.
Cervical disc herniation occurs most often in the lower cervical spine and is a cause of pain in neck, arm, or head. Numbness and weakness may occur. Thoracic disc herniation is rare, but may be a cause of chest or abdominal pain.
History
Initially symptoms suggestive of disc degeneration, then a ‘pop’ in the back with more acute intense back pain.
Buttock and leg pain develops over the next 48h.
Leg pain aggravated by sitting.
Leg pain improved by lying.
Leg pain worsened by coughing, sneezing, lifting, and straining.
Leg numbness and weakness, tingling or numbness
Examination
Patients may stand with a list away from the side of the leg pain.
Flex asymmetrically away from side with leg pain with active lumbar movement.
Muscle weakness. (Signs depend on level of herniation.)
Sensory (numbness) loss. (Signs depend on level of herniation.)
Diminished or absent reflexes. (Signs depend on level of herniation.)
Sciatic or femoral nerve tension signs:
Reduced SLR.
Lasegue positive.
Bowstring positive.
Slump test positive.
Investigations
MRI is the investigation of choice, though CT and CT myelography have previously been useful. MRI can demonstrate the four stages of disc herniation:
Degeneration.
Protrusion.
Extrusion.
Sequestration.
Proximity of disc bulge to neural structures can be assessed.
Treatment
Medication: analgesia and anti-spasmodics.
Bed rest when severe pain significantly restricts movement.
Generally encourage activity as soon as the patient can cope with it.
Back extension exercises may be useful.
Epidural injections may help with pain control, but do not improve neurological deficit.
Rehabilitation of flexibility and strength must be complete before return to sport
Prognosis
Most improve significantly with conservative management over 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree