In this systematic review, we present a comprehensive and up-to-date systematic review of the literature as it relates to the efficacy and effectiveness of spinal manipulation or mobilization in the management of cervical, thoracic, and lumbar-related extremity pain. There is moderate quality evidence that spinal manipulation is effective for the treatment of acute lumbar radiculopathy. The quality of evidence for chronic lumbar spine–related extremity symptoms and cervical spine–related extremity symptoms of any duration is low or very low. At present, no evidence exists for the treatment of thoracic radiculopathy. Future high-quality studies should address these conditions.
This article focuses on spinal manipulative therapy (SMT) and mobilization (MOB) as primary procedures often incorporated with physical therapy and physiotherapeutic modalities in the treatment of radicular signs and symptoms. In North America, SMT/MOB is performed by chiropractors, osteopaths, and physical therapists, with chiropractors accounting for more than 90% of all claims submitted for SMT.
For the purposes of this review, SMT/MOB is defined as an external force applied to the patients by the hand, an instrumental device, or a piece of furniture (eg, table or plinth), resulting in movement and/or separation of the joint articular surfaces with high or low velocity of joint movement.
Spine-related arm or leg pain is defined as the constellation of symptoms characterized by unilateral or bilateral radiating pain originating in the cervical or lumbar region and traveling into the extremity with or without neurologic signs. For the purpose of this article, spine-related extremity pain includes radiculopathy (loss of sensation, myotomal strength, or muscle stretch reflex), radicular pain (pain in the normal distribution of a spine nerve), and nonradicular radiating pain (pain radiating from the spine into the extremity in a nondermatomal pattern). The pathophysiologic basis for spine-related extremity symptoms is based on 3 proposed mechanisms, (1) biomechanical compression, (2) biochemical/inflammatory mechanism, and (3) neovascularization.
Epidemiology
Back-related and neck-related extremity conditions account for greater work loss, recurrences, and costs than uncomplicated low-back and neck pain. A review of epidemiologic studies and prevalence estimates of lumbar radiculopathy found the prevalence rates to vary from 1.2% to 43%. Studies that define sciatica as low-back pain (LBP) with leg pain below the knee place the prevalence at 9.9% to 25%. Furthermore, the lifetime prevalence of surgery for those with lumbar radiculopathy is 10% compared with 1% to 2% for those with LBP. Cervical spine disorders have been estimated to affect 9% to 12% of the general population. The average annual age-adjusted incidence rates for cervical radiculopathy have been documented as 83.2 per 100,000. Thoracic disk disease and herniation account for less than 2% of all spinal disk surgeries and 0.15% to 4% of all symptomatic spinal disk herniations.
Methods
This review included randomized controlled trials published before August 10, 2010 in English with no restrictions on methodological quality. A comprehensive search strategy developed by the Cochrane Back Group was used in the following databases: Medline, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Index to Chiropractic Literature, Mantis, and PEDro (Physiotherapy Evidence Database). Studies were included if they listed spine-related extremity symptoms (leg or arm pain, paresthesia, or numbness) as an inclusion criteria, used a spine-related extremity–specific outcome measure (eg, leg or arm pain), or specifically reported results for patients with spine-related extremity symptoms. Studies not specifying spine-related extremity symptoms as inclusion criteria were analyzed separately. Other inclusion criteria for this review included use of SMT and/or MOB of the spine as the primary therapy in at least one intervention group, alone or in combination with other active treatments. Studies in which the effects of manual treatment could be isolated were analyzed separately from those studies in which the effects of the manual treatment could not be isolated. Acceptable comparison groups included no treatment, placebo, and any other type of active intervention. Only patient-reported outcome measures were evaluated. The primary outcome measures for the review were pain, disability, and global perceived effect. Studies not performing between-group analyses for the measured outcomes were not included in the review. Short-term outcomes were defined as occurring within 3 months of the study therapy onset and long-term outcomes were defined as occurring at or after 6 months. The short-term outcome closest to the cessation of treatment was used as the primary short-term outcome for analysis. Actual scores (not change from baseline scores) for the relevant time points were used for analysis when available.
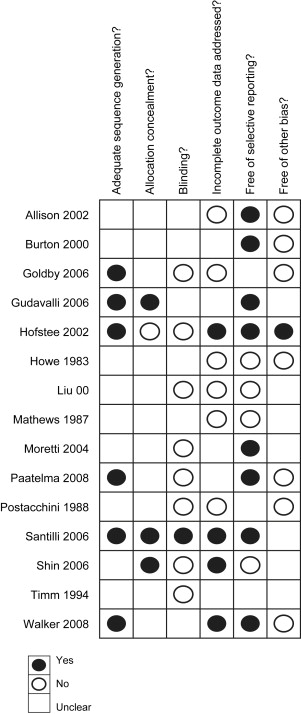
Studies were assessed for quality by 2 reviewers using the risk-of-bias assessment recommended by the Cochrane Collaboration. For a study to be considered low risk of bias, none of the 6 domains recommended by Cochrane (randomization, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, other) may be rated “no” and no more than 2 may be rated “unclear.” Because of the inherent complexities involved in blinding manual treatments, trials that did not blind providers or participants were rated unclear, provided that study personnel were unlikely to influence outcome assessments. For a study to be considered moderate risk of bias, a combination of one no and one unclear or 3 unclear ratings were permitted. All studies failing to meet the criteria for low or moderate risk of bias were rated as high risk of bias. The quality of the body of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach. Using the GRADE approach, high-quality evidence is defined as randomized clinical trials with low risk of bias that provide consistent, direct, and precise results for the outcome. The quality of the evidence was reduced by one level for each of the 6 domains not met (study design, risk of bias, consistency of results, directness, precision, publication bias). If only studies with high risk of bias were present for a given outcome, the quality of evidence was decreased by 2 levels for the risk of bias domain.
All continuous outcomes were analyzed using mean differences after converting to a 0 to 100 scale. Dichotomous outcomes were analyzed for statistical significance using odds ratios. Because of the problems involved with the clinical interpretation of odds ratios, dichotomous outcomes were presented in the tables as absolute risk differences. Statistical pooling was done in the case of 2 or more studies with comparable interventions, study groups, outcomes, and follow-up time points. The pooling methods were either fixed or random effects models, as indicated. Statistical heterogeneity between the studies was assessed using the χ 2 and I 2 statistic (proportion of variation between studies because of heterogeneity). If the null hypothesis of homogeneity was rejected ( P <.1 or I 2 >40), the pooled mean difference using a random effects model was calculated. In the case of statistical homogeneity, a fixed effect model was used. When statistical pooling was deemed inappropriate because of clinical heterogeneity, results were reported separately for individual trials. Direction of effect was reported as superior or inferior if the results were statistically significant. Results that failed to reach statistical significance were reported as similar unless the magnitude of effect was greater than 10 points (on a 0–100 scale), which resulted in the direction of effect being reported as favorable or unfavorable.
Results
Our search identified 631 potential studies of which 16 randomized trials with a total of 2132 participants fulfilled the inclusion criteria for the review. A list of excluded trials is provided in Table 1 . Of these trials, 5 investigated the effectiveness of SMT and/or MOB for cervical spine-related extremity symptoms and 11 investigated that for lumbar-related extremity symptoms. No trials investigating thoracic spine–related extremity symptoms were identified.
| Excluded Study | Reason |
|---|---|
| Andersson et al, 1999 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Arkuszewski, 1986 | Quasi-RCT |
| Blomberg et al, 1992/1994 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Brodin, 1983/1982 | Included neck pain with or w/o arm symptoms, but no subgroup findings or arm pain–specific outcomes were reported |
| Bronfort, 1989 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Bronfort, 1996 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Bronfort et al, 2000 | No between-group analysis performed |
| Bronfort et al, 2004 | No between-group analysis performed |
| Coppieters et al, 2003 | Study included only 1 treatment w/o immediate follow-up |
| Delitto et al, 1993 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Dziedzic et al, 2005 | Included neck pain with or w/o arm symptoms, but no subgroup findings or arm pain–specific outcomes were reported |
| Erhard et al, 1994 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Evans et al, 1978 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Ferreira et al, 2007 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Hemmila et al, 1997/2002 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Hoving et al, 2002 | Included neck pain with or w/o arm symptoms, but no subgroup findings or arm pain–specific outcomes were reported |
| Hurwitz et al, 2002 | Included neck pain with or w/o arm symptoms, but no subgroup findings or arm pain–specific outcomes were reported |
| Hurwitz et al, 2002 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Meade et al, 1990 | Excluded participants with suspected radiculopathy |
| Nwuga, 1982 | No patient-reported outcomes; quasi-RCT |
| Ongley et al, 1987 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Persson et al, 1997 | Manipulation/mobilization was not used on all patients in the treatment group |
| Seferlis et al, 1998 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Siehl et al, 1971 | No patient-reported outcomes; quasi-RCT |
| Young et al, 2009 | Manipulation/MOB used in both treatment groups |
| Zaproudina et al, 2009 | Included LBP with or w/o leg symptoms, but no subgroup findings or leg pain–specific outcomes were reported |
| Zylbergold et al, 1981 | Inclusion criteria did not specify if participants required leg symptoms |
Of the included studies, 11 listed spine-related extremity symptoms as inclusion criteria, with 5 of the studies requiring magnetic resonance imaging–confirmed disk herniation or neurologic signs for inclusion. Five of the trials included mixed populations of patients with and without spine-related extremity symptoms; 2 of these studies reported separate subgroup analyses, and the remaining 3 reported data on spine-related extremity–specific outcomes (eg, leg or arm pain). SMT was used in 9 studies, MOB in 5 studies, and a combination of SMT/MOB in 2 studies. Of these studies, 4 focused on patients with acute symptoms, 7 on those with chronic symptoms, and 3 on those with a mix of acute and chronic symptoms. One study did not specify condition duration. Comparison therapies included no treatment, placebo, heat, transcutaneous electrical nerve stimulation, ultrasonography, bed rest, corset, traction, chemonucleolysis, education, and exercise. The specific effect of SMT/MOB could be isolated in 13 of the 16 trials. Overall, the quality of the trials included in the review was poor. Only 1 of the included trials met the criteria for low risk of bias ( Fig. 1 ). All but 2 of the trials were too dissimilar in terms of patient characteristics, outcome measures, treatments, and comparisons to allow for statistical pooling.
Cervical Spine-Related Extremity Symptoms
We identified 5 trials investigating cervical spine–related extremity symptoms that met the inclusion criteria ( Table 2 ). All were rated as being at high risk of bias. Three trials isolated the effect of SMT/MOB, whereas 2 trials included combinations of therapies. Howe and colleagues found that a nonsignificant higher proportion of patients receiving SMT plus medication experienced short-term neck, shoulder, and arm pain improvement compared with patients receiving medication alone. Allison and colleagues observed a small, nonsignificant improvement in neck pain and disability in patients receiving MOB and home exercise compared with patients receiving no treatment in the short term. Walker and colleagues found a small nonsignificant improvement in upper extremity pain in patients receiving SMT/MOB plus home exercise compared with usual care plus placebo ultrasonography in the short and long term. Shin and colleagues reported SMT to be superior to traction for neck pain in the short term. Moretti and colleagues observed SMT to be superior to exercise and massage in the short term for pain.
| Trial (Risk of Bias) | Study Groups (Number of Patients) | Treatments (n) | Results |
|---|---|---|---|
| Howe et al, 1983 (high), acute | G1: SMT-MD + medication (26) G2: medication (26) | 1–3 |
|
| Allison et al, 2002 b (high), chronic | G1: MOB-PT + home exercise (9) G2: no treatment (10) | — |
|
| Walker et al, 2008 c (high), chronic | G1: SMT/MOB-PT + home exercise (50) G2: usual care + placebo ultrasonography (48) | 6 6 |
|
| Shin et al, 2006 b (high), unknown duration | G1: SMT (13) G2: traction (13) | 12 12 |
|
| Moretti et al, 2004 (high), mixed duration | G1: SMT-PT (40) G2: exercise, massage (40) | 2–3 2 |
a P <.05 for unadjusted pairwise comparisons.
b Studies listed radiculopathy as an inclusion criteria (neurologic signs or magnetic resonance imaging confirmed).
c Studies included mixed population of patients with and without arm pain.
The evidence for SMT and/or MOB for cervical spine–related extremity symptoms is very low in quality for all included comparison therapies. Thus, conclusions regarding effectiveness cannot be made ( Table 3 ).
| SMT and/or MOB | Comparison Intervention | Duration | Outcome | Short Term | Long Term | ||
|---|---|---|---|---|---|---|---|
| Direction of Effect | Quality of Evidence a | Direction of Effect | Quality of Evidence a | ||||
| SMT + medication (Howe et al, 1983) | Medication | Acute | Pain (% improved for neck & arm) | Similar | Very low | NA | No evidence |
| MOB + home exercise (Allison et al, 2002) | No treatment | Chronic | Pain | Similar | Very low | NA | No evidence |
| SMT + home exercise (Walker et al, 2008) | Usual care + placebo | Chronic | Pain (arm) | Similar | Very low | Similar | Very low |
| SMT (Shin et al, 2006) | Traction | Unknown | Pain (neck) | Superior | Very low | NA | No evidence |
| SMT (Moretti et al, 2004) | Exercise + massage | Mixed | Pain | Superior | Very low | NA | No evidence |
a GRADE definitions: high, further research is very unlikely to change our confidence in the estimate of effect; moderate, further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low, further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low, any estimate of effect is very uncertain.
Lumbar Spine–Related Extremity Symptoms
Eleven trials were identified on lumbar spine–related extremity symptoms, which met the inclusion criteria ( Table 4 ). Only 1 of the studies was rated as being at low risk of bias and 2 rated as moderate risk ; the remaining 8 trials were considered to be at high risk of bias. Ten studies isolated the effect of SMT/MOB; one included a combination of SMT and MOB. Santilli and colleagues showed SMT was superior to sham SMT for leg and back pain in the short and long term. Coxhead and colleagues found that SMT was superior to traction, exercise, and corset for pain in the short term. Mathews and colleagues observed SMT to be superior to heat for the percentage of improved patients in the short term. Burton and colleagues reported SMT to be superior to chemonucleolysis for back pain and disability in the short term and nonsignificantly better in the long term. Timm found MOB to be superior to passive modalities and no treatment but inferior to exercise for disability in the short term. Goldby and colleagues showed MOB plus general exercise to be inferior to both stabilization exercise and education for leg pain in the short and long term. Paatelma and colleagues found a nonsignificant improvement in leg pain among patients receiving SMT/MOB plus home exercise compared with education in the short and long term. Paatelma and colleagues also found a small, nonsignificant improvement for exercise compared with SMT/MOB plus home exercise for leg pain in the short term, but the groups were similar in the long term.
| Trial (Risk of Bias) | Study Groups (Number of Patients) | Treatments (n) | Results |
|---|---|---|---|
| Coxhead et al, 1981 (high), chronic | Factorial design, all combinations of 1. SMT-PT, back school, diathermy 2. Traction, back school, diathermy 3. Exercise, back school, diathermy 4. Corset, back school, diathermy | 5–10 |
|
| Mathews et al, 1987 (high), acute | G1: SMT-PT (132) G2: heat (101) | <106 |
|
| Burton et al, 2000 b (high), chronic | G1: SMT-DO (20) G2: chemonucleolysis (20) | 6–18 | |
| Santilli et al, 2006 b (low), acute | G1: SMT-DC (53) G2: sham SMT-DC (49) | 20 20 | |
| Postacchini et al, 1988 c (high), mixed duration | G1: SMT-DC (35) G2: mediation (35) G3: massage & diathermy (31) G4: bed rest (14) G5: back school (16) G6: placebo ointment (32) | 11–17 10–15 14–21 8 d 4 7–14 |
|
| Timm, 1996 (high), chronic | G1: MOB-PT (50) G2: heat, TENS, ultrasonography (50) G3: exercise, low technology (50) G4: exercise, high technology (50) G5: no treatment (50) | 24 24 24 24 | |
| Goldby et al, 2006 c (high), chronic | G1: MOB-PT, exercise (89) G2: exercise, stabilization (84) G3: education (40) | 10 10 1 | |
| Gudavalli et al, 2006 c (moderate), chronic | G1: MOB-DC (19) G2: exercise (19) | 8–16 8–16 |
|
| Paatelma et al, 2008 c (high), mixed duration | G1: SMT/MOB-PT, home exercise (45) G2: exercise (52) G3: education (37) | 6 6 1 | |
| Hofstee et al, 2002 b (moderate), acute | G1: MOB-PT, exercise, hydrotherapy (83) G2: bed rest (84) G3: education (83) | 8–16 7 d 1 | |
| Liu & Zhang, 2000 (high), mixed duration | G1: SMT (62) G2: traction (50) | — 28 |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





