Abstract
Purpose
The perception of verticality results from the integration of vestibular, visual and somatosensory information. Spinal cord injured patients with complete paraplegia have total somatosensory deafferentation below a certain metameric segment. In our study, we were interested in the implication of somatosensory signal in the construction of verticality and in the possible effect of somatosensory loss on spatial representation.
Method
We analysed haptic and postural aspects of perceived verticality in 14 spinal cord injured patients with complete paraplegia and in an age- and gender-matched group of 13 controls. We also conducted a structured interview on the existence of vertigo or postural instability in daily life.
Results
The spinal cord injured patients perceived verticality without any significant directional bias in the orientation of the vertical but with a greater uncertainty than control subjects, both in haptic and postural modalities. If paraplegic did not report vertigo, half described an altered spatial perception without vision.
Conclusion
The present results confirm the importance of sensory input from the trunk and the lower limbs in the perception of the vertical. However, visual and vestibular information appear to compensate for somatosensory deafferentation.
Résumé
Objectif
La perception de la verticale résulte de l’intégration d’informations vestibulaires, visuelles et somesthésiques. Chez les blessés médullaires complets, il existe une déafférentation somesthésique totale sous un niveau métamérique donné. Dans cette étude nous analysons la contribution de la somesthésie à la construction d’une représentation de la verticale, ainsi que les éventuelles conséquences d’une déafférentation somesthésique sur la représentation de l’espace chez le blessé médullaire.
Méthode
Analyser les verticales subjectives haptique et posturale de 14 paraplégiques complets et 13 sujets témoins appariés en âge et genre. Réaliser une interview structurée de l’existence de vertige ou d’instabilité posturale en vie quotidienne.
Résultats
Les paraplégiques perçoivent la verticalité sans biais directionnel significatif dans l’orientation de la verticale posturale mais avec une plus grande incertitude que les sujets témoins pour les verticales haptique et posturale. Si les paraplégiques ne se plaignent pas de vertige, la moitié d’entre eux rapporte une perception spatiale altérée sans la vision.
Discussion–conclusion
Ces résultats réaffirment l’importance de l’entrée sensorielle du tronc et des membres inférieurs dans la perception de la verticale. Cette déafférentation somesthésique est en grande partie compensée par les informations visuelles et vestibulaires.
1
English version
1.1
Introduction
Spatial orientation with respect to gravity is essential for maintenance of an upright posture, locomotion and most motor activities. Three different sensory systems – the vestibular, visual and somatosensory systems – regulate these complex behaviours . The afferent information is integrated and then processed in the brain stem and the cerebral cortex .
Abnormal perception of the body’s spatial orientation (and notably its verticality) can be observed after various types of central or peripheral nervous system injury or damage to the vestibular system . For example, patients with a hemisphere stroke can present impaired verticality perception, with contralesional bias in their postural vertical (PV) and visual vertical (VV) . Dissociation of the two parameters may occur . In contrast, patients with a brain stem stroke may present ipsilesional bias affecting the VV but retain normal perception of the haptic vertical (HV) . Similarly, patients with peripheral vestibular damage present an ipsilesional orientation bias that affects the VV but not the PV .
Although there is a consensus on the primordial role of the somatosensory system in perception of the vertical , the details of this mechanism have not yet been elucidated. How do somatosensory perturbations affect the perception of verticality? In two patients presenting moderate to severe hemi-hypoaesthesia induced by cortical damage (thalamic stroke and right parietal stroke) Anastopoulos et Bronstein evidenced a 4–5° bias in the PV towards the side of sensory loss. No significant disturbance of the PV in patients presenting spinal ischemia or polyneuropathy has been reported . In addition to orientation bias, some patients present a certain degree of uncertainty in their verticality perception .
Spinal cord injured patients with complete paraplegia are characterized by somatosensory deafferentation below a certain metameric segment. We wondered what the effect of this deafferentation on the perception of verticality might be and how it might then affect activities of daily living. In subjects with history of falls , it has been shown that a tilted PV was linked to postural disability.
The objectives of the present study were as follows:
- •
to analyze the somaesthetic perception of verticality in spinal cord injured patients;
- •
to establish how somatosensory graviception contributes to construction of the subjective postural vertical;
- •
to study the possible clinical consequences of impaired perception of verticality in spinal cord injured patients.
1.2
Materials and methods
1.2.1
Selection of study participants
We investigated the perception of verticality in 14 patients with complete paraplegia, in comparison with an age-, weight-, height- and gender-matched group of 13 healthy control subjects ( Table 1 ). All volunteers gave their informed consent to participation in the study. The paraplegic patients had to meet the following inclusion criterion: a complete spinal cord lesion (whether caused by trauma or not) with total sensory deficiency below a defined lesional level. Patients with other central or peripheral nervous system lesions, vestibular damage or claustrophobia were excluded from the study. The lowest normal metameric segments in the paraplegic study participants were as follows: T4 (four patients), T5 (two patients), T6 (three patients), T7 (one patient), T8 (one patient) and T12 (three patients). All patients were right-handed and medically stable. The mean ± standard deviation time since the spinal cord injury was 93.5 ± 51 months.
| Healthy controls ( n = 13) | Paraplegics ( n = 14) | P | |
|---|---|---|---|
| Age (years) | 39.15 ± 10.34 | 41.64 ± 10.83 | 0.44 |
| Weight (kg) | 70.31 ± 13.44 | 76.07 ± 14.83 | 0.26 |
| Height (cm) | 173.92 ± 6.88 | 175.92 ± 6.03 | 0.48 |
| Gender (women/men) | 2/11 | 2/12 | 0.92 |
1.2.2
The structured questionnaire
In order to evaluate any perceived impairments in subjective spatial positioning, the spinal cord injured patients filled out a structured questionnaire comprising the following five questions:
- •
Do you sometimes feel dizzy?
- •
In the sitting position, does your perception change when you open or close your eyes?
- •
Do you ever lose your balance?
- •
Do you ever feel unstable during transfers?
- •
Do you have difficulty positioning your trunk in space?
1.2.3
Assessment of the perception of verticality
For each subject, we measured the postural and haptic verticals. The subject sat in complete darkness inside a gimbal. The various tests were performed in a pseudo-random order, in order to avoid sampling bias.
1.2.3.1
The postural vertical
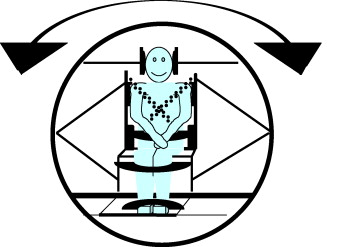
The subjective PV was measured in a specially adapted gimbal ( Fig. 1 ) according to the wheel paradigm . The subject’s head and trunk were restrained. The initial step in the procedure consisted in manually tilting the subject by –50° or 50° in the sagittal (roll) plan. The gimbal was then slowly rotated (1.5–2° per second) back towards the other side. The subject was told to indicate the moment at which he/she had returned to the vertical position. An integrated digital inclinometer enabled continuous monitoring of the system’s tilt. The PV was described in terms of the difference between the subject’s perceived vertical and the gravitational vertical. By convention, leftward deviations were given a negative sign and rightward deviations were given a positive sign. Ten measurements (five tilts to the left and five to the right) were successively performed in a pseudo-random order. The orientation and the uncertainty of the PV were then calculated. The orientation was defined as the mean of the ten measurements and the uncertainty corresponded to the scatter (i.e. the standard deviation).
1.2.3.2
The haptic vertical
The subject sat in the gimbal in complete darkness but was free to move his/her head. A wooden frame with an affixed metal rod was presented to the subject. The set-up as a whole was fixed to a support that enabled the frame’s height and orientation to be adjusted. The subject had to use his/her dominant hand to set the rod to a vertical position. Ten measurements were performed (five from left to right and five from right to left). The HV was defined as the angle difference between the subject’s tactile perception of verticality and the gravitational vertical. By convention, leftward deviations were negative and rightward deviations were positive.
1.3
Statistical analysis
A descriptive statistical analysis was performed for all recorded variables. Inter-variable correlations were tested using Spearman’s non-parametric correlation coefficient. Groups, subjective verticality modes and body tilts were compared in an analysis of variance (ANOVA) or by using non-parametric T test of mean values. The statistical significance threshold was set to P = 0.05. Parameter values are expressed as the mean ± standard deviation.
1.4
Results
1.4.1
The structured questionnaire
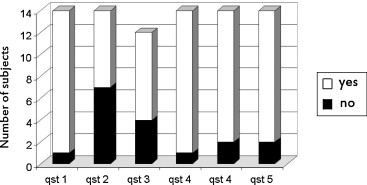
Even though most of the paraplegic subjects did not feel dizzy or unstable or have any difficulty in positioning their trunk in space with their eyes open, half reported poor balance and perception of body orientation in “eyes closed” situations ( Fig. 2 ). This result suggests that paraplegic patients use visual components to compensate for their somatosensory deafferentation.
1.4.2
Perception of verticality in the sitting position
The results for perceived verticality in the sitting position are given in Table 2 . We first compared the paraplegic patients and the control subjects by using a non-parametric T test. Although the mean orientation parameters did not differ significantly, the uncertainty in the PV was greater in the paraplegic group. We then completed our analysis of the uncertainty by performing an ANOVA with two factors: group and verticality mode (HV and PV). We observed greater uncertainty in the paraplegic group ( F (1.25) = 5.42, P < 0.03) and greater uncertainty for the HV than for PV ( F (2.25) = 29.94, P < 0.001). There was no interaction between the group and verticality mode factors ( F (2.25) = 0.23, P = 0.63). These findings suggest that even though paraplegic patients do not have systematic bias in their perception of verticality, their degree of certitude on the direction of the vertical is lower than in controls.
| Healthy controls n = 13 | Paraplegics n = 14 | P | |
|---|---|---|---|
| Haptic vertical | |||
| Orientation (°) | −0.35 ± 0.84 | 0.38 ± 0.83 | 0.10 |
| Uncertainty (°) | 1.73 ± 0.80 | 2.39 ± 1.27 | 0.19 |
| Postural vertical | |||
| Orientation (°) | 0.45 ± 1.02 | 0.22 ± 1.26 | 0.12 |
| Uncertainty (°) | 0.60 ± 0.46 | 1.05 ± 0.74 | 0.05 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







