Snapping Scapula Syndrome
Jon J. P. Warner
Matthew F. Dilisio
Bassem T. Elhassan
DEFINITION
Scapulothoracic crepitus first was described by Boinet4 in 1867.
It is characterized by painful scapular motion with associated crepitus during scapulothoracic motion, with or without a clear history of injury or trauma.20,21
Snapping scapula syndrome has also been referred to as scapulothoracic bursitis, retroscapular creaking, superior scapular syndrome, retroscapular pain, washboard syndrome, and rattling of the shoulder blade.8,14,20,21,28
The associated audible crepitus, which can be tactile in most instances, has been described by Milch and Burman21 as a tactile-acoustic phenomenon, possibly generated secondary to an abnormality in the scapulothoracic interval.
This crepitus is divided into three classes based on the volume of the sound produced.20
ANATOMY
The scapulothoracic articulation consists of the interface between the anterior aspect of the scapula and the ribs in the posterior aspect of the convex thoracic chest wall (FIG 1).
The mean superomedial angle of the scapula is has been estimated to be 139 to 154 degrees and the average thickness of the superior poles is a mean1,17,36 of 3.4 to 3.9 mm.
The osseous anatomy of the scapula is variable.1 The scapulothoracic articulation is cushioned by several muscles, specifically the subscapularis and the serratus anterior. The serratus anterior has both a broad origin on the chest wall and a broad insertion along the majority of the ventral surface of the medial scapula (FIG 2).
A bare area devoid of muscular attachments has been described between the origins of the subscapularis and serratus anterior averaging 22.3 × 10.8 mm and has been implicated as a possible source of pathologic scapulothoracic impingement.5
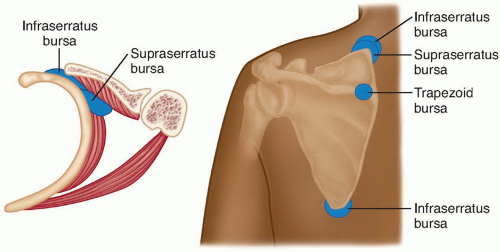
FIG 1 • Four different bursae are shown—two infraserratus, one supraserratus, and one trapezoid bursae.
In addition, two major and four minor bursae have been described in the scapulothoracic articulation13,14,37 (see FIG 1).
The two major bursae are the infraserratus bursa, located between the serratus anterior muscle and the chest wall, and the supraserratus bursa, located between the serratus anterior and the subscapularis muscles.
The four minor bursae are distributed as follows: two at the superomedial angle of the scapula, one at the inferior angle of the scapula, and one at the medial base of spine of the scapula, underlying the trapezius muscle.
PATHOGENESIS
Incongruence of the scapulothoracic articulation has been postulated to be the main cause of the snapping scapular syndrome, which may or may not be associated with osseous anomalies of this region.25,31
Maltracking or dynamic compression of the scapulothoracic articulation has been postulated as an etiology of this syndrome because it leads to irritation of the bursa secondary to pathologic contact between the ribs and the superior angle of the scapula.9,37
This maltracking is considered to be a soft tissue cause of snapping scapula syndrome, which has been reported in cases of subscapularis atrophy secondary to glenohumeral fusion and long thoracic nerve palsy.21,38
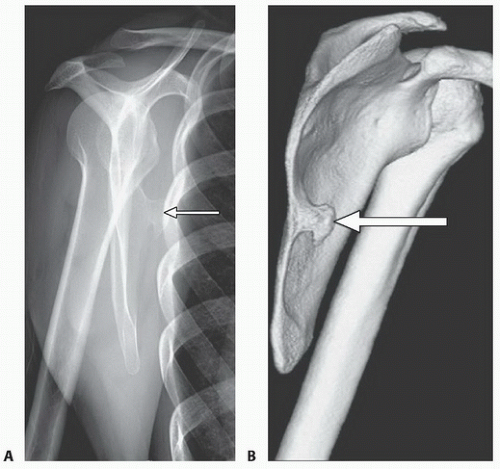
Osseous causes of snapping scapula syndrome are rare. These include scapular osteochondromas and exostoses (FIG 3), anterior angulation of the scapula, scapular fracture, scapular tubercle of Luschka, skeletal abnormalities of the vertebrae (omovertebral bone), and abnormal angulations and tumors of the ribs.20,21,35
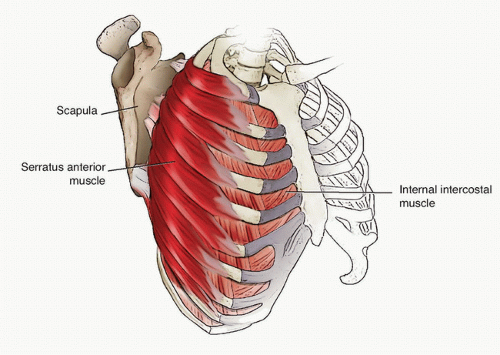
FIG 2 • The serratus anterior has both a broad origin on the chest wall and a broad insertion along the majority of the ventral surface of the medial scapula.
Several osseous anatomic variants on the ventral surface of the scapula have been implicated as a potential cause of snapping scapula syndrome.
The tubercle of Luschka is a ventral osseous prominence at the superomedial angle of the scapula, which was found in 3% of cadaveric specimens. A teres major tubercle was found in 43.2%, and a teres major process was found in 6.8%.36
NATURAL HISTORY
Patients with snapping scapula syndrome usually complain of pain around the shoulder girdle.
This pain most often is secondary to bursitis in the scapulothoracic articulation at the superomedial border. Constant motion irritates the soft tissues, leading to inflammation and a cycle of chronic bursitis and scarring.
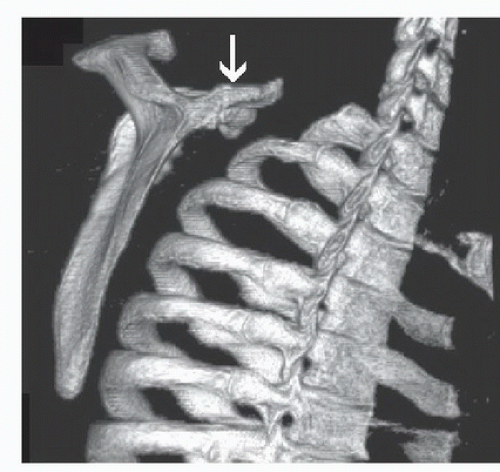
FIG 3 • An osteochondroma (arrow) of the superomedial angle of the scapula may, rarely, be the cause of snapping scapula syndrome.
The chronic inflammation of the bursae will lead to fibrotic, scarred, and tough bursal tissues that can lead to mechanical impingement and pain with motion, resulting in further inflammation.
Once the patient reaches this level of chronic bursal inflammation, the symptoms rarely subside by themselves without trial of rest and physical therapy.
In many cases, especially when the cause of snapping is skeletal, surgical intervention becomes essential to manage this problem.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with scapulothoracic bursitis report a history of pain in the shoulder or neck with overhead activities for months or years and often have a history of repetitive overuse in work or recreation or a history of trauma.12
Alternatively, some patients report a history of relatively painless shoulder crepitation that has only recently become painful.
A history of neck injury, shoulder injury or fracture, or previous shoulder surgery should be ruled out.
Audible or palpable crepitus may accompany the symptoms with scapulothoracic motion.
Patients can often reproduce their symptomatic crepitation on command, which often involves exaggerated shrugging of the shoulders.
Some patients report a family history of the disorder and have bilateral symptoms.
Improvement of symptoms by lifting the scapula off the chest wall helps localize the source of pathology to the scapulothoracic articulation.
Alternatively, the scapula assistance test (SAT) may improve the patient’s symptoms by increasing the posterior tilt of the scapula in cases of snapping scapula syndrome due to dyskinesia. This test is performed by the examiner manually placing inferomedial directed pressure on the scapular body in an attempt to manually correct/assist scapular maltracking. A positive test is an improvement in the patient’s symptoms with this maneuver.11 A positive SAT often indicates that a
patient’s symptoms may significantly improve with intensive physical therapy to correct scapular dyskinesia.
Diagnosis is confirmed if significant relief or even elimination of the pain occurs when local anesthetic and corticosteroids are injected in the scapulothoracic bursa under the superomedial border of the scapula.
The examiner also must assess soft tissue tightness, muscle strength, and flexibility around the involved shoulder.
Altered scapula motion is often due to tightness in the scalene muscles, pectoralis minor, or pectoralis major. Dyskinesia and winging can be caused by weakness in the serratus anterior or lower trapezius. Finally, upper trapezius hypertrophy may contribute to altered scapular kinematics due to anterior tilting of the scapular body on the chest wall.11
In patients with winging of the scapula, a careful neuromuscular examination should be performed to differentiate true winging from compensatory pseudowinging that might originate from a painful scapulothoracic articulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree