Slipped Capital Femoral Epiphysis
David A. Spiegel
B. David Horn
CLINICAL PRESENTATION
Slipped capital femoral epiphysis (SCFE) represents a displacement of the proximal femur relative to the capital femoral epiphysis, which occurs through the physis. Both anatomic and biomechanical abnormalities may render the physis more susceptible to shear stresses, including retroversion of the hip, a posterior inclination at the proximal femoral physis, and weakening of the perichondrial ring associated with the adolescent growth spurt. Mechanical factors are also felt to play an important role, as most patients are above the 95th percentile for weight. A slipped epiphysis most commonly occurs in boys from 13 to 15 years of age and in girls from 11 to 13 years of age. Bilateral involvement will occur in 25% to 60% of patients. The incidence is approximately 1/100,000 and may well be increasing given the fact that childhood obesity has become a public health concern in the United States.1
While SCFE may be seen in association with endocrinopathies and metabolic disorders, the vast majority of patients will have a normal endocrinologic evaluation. An underlying endocrinopathy should be suspected when the diagnosis is made in a thin patient or when the age is atypical for a slipped epiphysis (<10 years or >16 years). Underlying diagnoses associated with a slipped epiphysis include hypothyroidism, growth hormone deficiency (with or without replacement therapy), panhypopituitarism, hypogonadism, and renal disease (secondary hypoparathyroidism). Patients who have received pelvic irradiation are also susceptible.
An early diagnosis is essential, and referred pain is one cause of delay in diagnosis.2,3 Patients commonly present with pain in the groin, but the discomfort may also be referred to the thigh or the knee. The pain is dull in character, worsened by activity, and progressive in nature. A small subset of patients will present with the acute onset of severe pain, often following a minor injury. In these cases, the slipped epiphysis may be likened to an acute physeal fracture. Most patients have an externally rotated gait even before developing a slipped epiphysis, and external rotation or out-toeing will be increased further in the presence of a slipped epiphysis.
There have been two schemes used to classify SCFE. The clinical classification of stable versus unstable is perhaps most useful. Patients with a stable SCFE are able to bear weight (with or without crutches), and those with an unstable SCFE are unable to bear weight.4 While patients classified as stable have approximately a 1% risk of avascular necrosis, those with an unstable slip (approximately 5%) have a much higher risk of avascular necrosis (15%-47%). Avascular necrosis is commonly complicated by premature joint degeneration. A temporal classification has also been proposed, including acute (<3 weeks duration of symptoms), chronic (>3 weeks duration), and acute on chronic (recent exacerbation of symptoms that have been present for weeks to months). The long-term outcome relates to the degree of displacement (malalignment at the junction of the femoral head and neck) at the time of stabilization or at closure of the physis and whether or not complications such as chondrolysis or avascular necrosis occur. Patients with residual deformity may develop impingement (metaphyseal prominence strikes the acetabulum), resulting in pain and/or mechanical symptoms such as popping or locking.5 Those with moderate to severe malalignment will develop early osteoarthritis, often in the third or fourth decade.
CLINICAL POINTS
The condition most commonly occurs in adolescent, African American boys who are above the 95th percentile for weight.
When affected, girls are often younger than boys.
Patients present with pain in the groin, thigh, or knee and may walk with a limp or be unable to bear weight.
Etiology is multifactorial and involves both mechanical and biologic factors
PHYSICAL FINDINGS
Patients are usually obese and ambulate with an externally rotated gait. Those who are able to ambulate will shift their body weight over the involved hip (or hips) during stance phase, and the degree of external rotation is greater on the affected side in those with unilateral involvement. On bench examination, there is a decrease in flexion, abduction, and internal rotation relative to the normal side. The extremity will roll into external rotation with progressive flexion of the hip, and there is discomfort with internal rotation. Both hips should always be assessed, as 20% of patients will present with bilateral disease. Patients with an unstable slip, in addition to the inability to bear weight, may present with the limb held in flexion, abduction, and external rotation and may resist any attempts to move the extremity. Patients with residual deformity and impingement at the head-neck junction may have pain on provocative testing (flexion, adduction, and internal rotation).
STUDIES (LABS, X-RAYS)
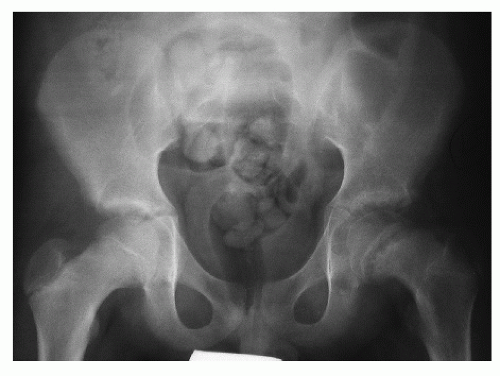
Laboratory studies are not routinely indicated in the evaluation of slipped epiphysis, unless atypical clinical findings are present. Most cases of SCFE can be diagnosed with plain radiographs, although occasionally an magnetic resonance imaging will identify edema within the physis when there is a “pre-slip.” The earliest finding is widening and irregularity of the physis. On the anteroposterior (AP) radiograph, a line drawn parallel to the superior femoral neck (Klein line) should intersect the lateral portion of the capital femoral epiphysis (Fig. 58-1A). A slipped epiphysis is suspected when this finding is not observed. The degree of displacement is best appreciated on the lateral view (ideally, a true lateral), and there will be a prominence of the anterior femoral neck at the junction of the epiphysis and the neck. This prominence may become smoother over time due to remodeling (Fig. 58-2). While the typical radiographic appearance of a SCFE involves posterior and medial displacement of the epiphysis, rarely a “valgus” slipped epiphysis is observed in which the epiphysis is posterior and lateral (Fig. 58-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree