Abstract
Objective
To analyse postural stability and the single-leg hop for distance in subjects 2 years after anterior cruciate ligament reconstruction (ACLR), in comparison with an age- and activity-matched control group.
Design and setting
Subjects reported to a sports medicine or athletic training research laboratory for testing.
Subjects
Twenty-six subjects having undergone ACLR and 26 age- and activity-matched controls were selected to participate in this study. An arthroscopically-assisted, central, one-third bone-patellar tendon procedure was used to repair the ACLs.
Measurements
One-leg stance postural stability was measured with the NeuroCom Balance Master ® platform system. We recorded the single-leg hop for distance as an objective measure of function.
Results
We found a significant difference ( p < 0.05) between the ACLR and control subjects in terms of the one-leg stance sway velocity (knee fully extended) on the operated side.
Conclusions
After ACLR (mean time postoperatively: 24 ± 1 months), single-leg hop for distance score was normal, when compared with the contralateral limb. Our results indicate that 2 years after surgery, single-limb postural stability in the ACLR group differed significantly from that in the control group. The persistence of poor stability control may be correlated to an impairment in proprioception.
Résumé
Objectif
Évaluer l’équilibre postural et le saut en longueur monopodal chez des footballeurs à recul moyen de deux ans de la reconstruction du LCA.
Population
Vingt-six sportifs victimes de la reconstruction LCA et 26 sujets indemnes de toutes antécédents pathologiques ont participé à cette étude. La technique chirurgicale est de type Kenneth Jones.
Protocole
L’équilibre postural en appui monopodal est réalisé sur Balance Master Neurocom ® avec deux variantes : genou tenu et genou en flexion à 20°. Le test monopodal en longueur « one-leg hop » est choisi pour la mesure de la performance fonctionnelle.
Résultats
Une différence statistiquement significative est obtenue en faveur du membre opéré, lors de l’équilibre postural monopodal genou en extension ( p < 0,05).
Conclusions
À recul moyen de 24 mois de la reconstruction du LCA, nos footballeurs ont une symétrie fonctionnelle entre les deux membres. En revanche, il y a la persistance d’un déficit postural lors de l’évaluation monopodale sur plate-forme. Ce résultat comparable à la littérature semble être corrélé à la perte de la sensibilité proprioceptive en conséquence à la chirurgie du LCA.
1
English version
1.1
Introduction
Injury to the anterior cruciate ligament (ACL) results in mechanical and functional instability . Athletes often find it difficult to recover full function after an ACL injury and surgery is frequently indicated .
ACL injury leads to loss of mechanoreceptor feedback and loss of reflex muscle contractions . Furthermore, ACL injury often results in perceived instability of the knee joint and leads to decreased static stability .
After ACL rupture or reconstruction, the main goal of rehabilitation is to improve dynamic stability (despite the decrease in mechanical stability) and restore knee function by enhancing neuromuscular control; this can be achieved by developing muscle strength, coordination and proprioceptive abilities .
Neuromuscular training programmes for patients with ACL reconstruction (ACLR) seek to improve muscle activation, increase dynamic joint stability and relearn the movement patterns and skills used during activities of daily living and sports activities .
After ACL injury or reconstruction, muscle strength is commonly evaluated with isokinetic dynamometry. Moreover, a strength test battery (which includes knee extension, knee flexion, and leg-press muscle power tests) can clearly reveal leg muscle power deficits in ACLR patients .
Postural control corresponds to a person’s ability to control the body’s position in space while maintaining stability and orientation and can be assessed using measurements of balance in stance .
Technological advances have now made it possible to evaluate postural control very accurately. During static posture, the key measure used to calculate balance is “centre of pressure” (CoP) oscillation.The Balance Master ® system (from NeuroCom International, Inc, Clackamas, OR, USA) is designed to assist the assessment and treatment of balance and mobility perturbations in subjects, regardless of whether these impairments and functional limitations have resulted from orthopaedic or surgical interventions. The system can be used with high-level ACLR patients who are refining the rapid loading and unloading movements needed to return to their sport.
There are several jump tests and jump test batteries for assessing knee function in patients with ACL damage or reconstruction . The vertical jump, hop for distance, drop jump followed by double hop for distance, square hop and side hop all have high test–retest reliability . It has been reported that a test battery including a vertical jump, a hop for distance and a side hop can clearly discriminate between hop performance of the injured and uninjured leg in patients with ACLR .
The purpose of the present study was “to analyse postural stability and single-leg hop” measurements in post-ACLR subjects and compare them with an age- and activity-matched control group.
1.2
Materials and methods
1.2.1
Subjects
Postural stability and functional performance were evaluated in 26 soccer players having undergone a single ACLR (mean ± S.D. age: 22 ± 3.11; height: 172.8 ± 4.17 cm; weight: 72.1 ± 7.15 kg) and a control group comprising 20 age- and activity-matched subjects (age: 23.96 ± 2.02 years; height: 180.2 ± 0.06 cm; weight: 78.37 ± 9.58 kg).
All recruited patients had undergone the same type of ACLR (arthroscopically-assisted central bone-patellar tendon–bone graft) and had returned to competitive activity (after an average time interval of 8 months ± 2 weeks). The mean time since surgery was 24 months ± 1 week. All subjects gave their written, informed consent to participation in the study.
1.2.2
Inclusion criteria
Subjects were selected to participate only if they met the following criteria:
- •
only one surgical intervention for a torn ACL, with no concomitant tear of the posterior cruciate ligament;
- •
no evidence of collateral ligament repair at the time of surgery;
- •
no history of surgery or traumatic injury to the contralateral knee;
- •
no history of surgery or traumatic injury to the ankle joint on the reconstructed side;
- •
no history of surgery or traumatic injury to either hip joint;
- •
no history of a medical problem that had limited activities within the 6 weeks prior to testing;
- •
a full return to their previous competitive level;
- •
no complaints concerning instability.
1.2.3
Test procedures
Subjects were asked to take part in a testing session. Before testing, subjects signed the informed consent form. The test order for the postural stability and single-leg hop tests was randomized to avoid learning or fatigue effects. The testing session started with a 5-minute warm-up. Subjects were then instructed to perform several lower body flexibility exercises.
1.2.4
The Balance Master ® system
The Balance Master ® provides objective assessment and retraining of the sensory and voluntary motor control of balance with visual biofeedback. The system uses a fixed, 18′′ × 60′′ dual force plate to measure the vertical forces exerted through the patient’s feet.
The long force plate enhances assessment and training capabilities.
The interactive technology and clinically proven protocols allow the clinician to objectively assess patients performing a range of tasks, from essential activities of daily living through to high-level athletic skills. The objective data aid in the design of effective treatment and/or training programmes focused on the specific sensory and motor components underlying a patient’s functional limitations.
The goal in managing balance and mobility disorders is the minimization of disability and improvement of functional performance. However, patients with similar pathologies frequently present with significant differences in impairments and functional limitations. In view of these differences, patients with similar pathologies respond differently to a given treatment.
NeuroCom offers a comprehensive library of assessment protocols for quantifying the impact of impairments on a patient’s ability to perform balance and mobility tasks required for safe and effective function in daily life. In short, the protocols provide the information required for accurate diagnosis of balance dysfunction and effective clinical management.
All NeuroCom assessments are compatible with the World Health Organization (ICDIH-2) and Nagi disablement frameworks and have been validated by extensive scientific and clinical research.
The unilateral stance quantifies postural sway velocity with the patient standing on either the right or left foot on the force plate, with the eyes open and then with the eyes closed. Each trial lasts for 10 s.
The force plate is set into the platform base. The subject stands on the dual force plate and faces the monitor. Force sensors under the force plate measure the vertical forces exerted through the patient’s foot. A cable carries this information from the dual force plate to the computer.
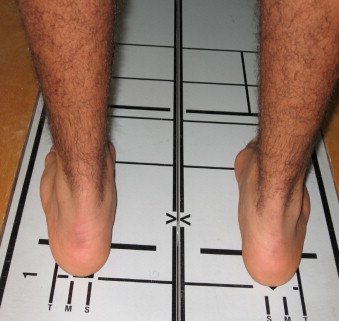
The patient stands on the force plate with his/her feet positioned so as to align each medial malleolus with the wide line and the outside border of the heel with the height-appropriate line ( Fig. 1 ).
1.2.5
Platform test procedure
The test procedure consisted of static assessments. We assessed single-limb (right and left) stance postural stability. Subjects were allowed two practice trials.
The assessment quantifies postural sway velocity while the athlete stands calmly on one foot on the force plate. The relative absence of sway in the “hold still” position indicates better stability.
The single-leg stance assessment consisted of four sets of three trials, normally conducted in the following order:
- •
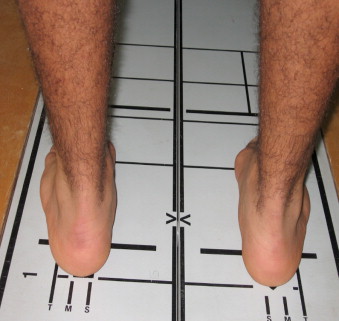
knee fully extended (left, right) (EXT) ( Fig. 2 a );
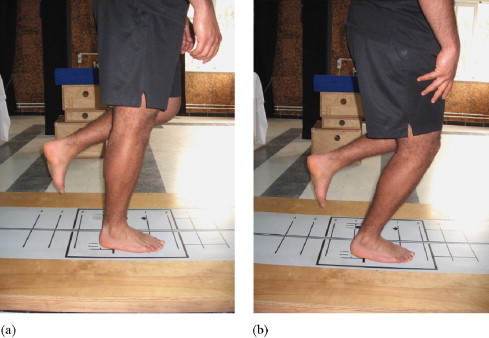
Fig. 2
(a,b) The single-leg stance. a: knee fully extended; b: knee flexed 20°.
- •
knee flexed at 20° (left, right) (FLEX) ( Fig. 2 b).
This assessment quantifies the postural sway velocity of each leg. The sway velocity (in degrees per second) is given for all three trials. Subjects were allowed a 1-minute rest between tests.
1.2.6
The single-leg hop for distance test
The single-leg hop for distance is a commonly used functional measurement designed to test both strength and confidence in the tested leg; it correlates positively with muscle strength . The first leg to be tested was chosen at random. The single-leg hop was performed three times with each leg. Subjects were asked to hop as far as possible from a predetermined line and to land on the same leg. The use of arm swing was not discouraged, as subjects were asked to perform with maximal effort. The best of the three tests was recorded in centimetres and used as the dependent score .
1.2.7
Statistical analyses
The injured leg (right/left) in the ACLR subjects was matched with the same-side leg in the uninjured subjects. We used Wilcoxon and Mann-Whitney non-parametric tests. Pearson’s test was used to study multiple correlations and detect any links between the assessment modes. All statistical tests were considered significant at the p less than 0.05 level.
1.3
Results
We found a significant difference ( p < 0.05) between ACLR and control subjects for the single-limb stability sway velocity (knee fully extended) on the operated side ( Table 1 ).
| Group | Leg | EXT | FLEX |
|---|---|---|---|
| ACLR | Operated | 0.95 ± 0.2 a | 0.83 ± 0.13 |
| Non-operated | 0.85 ± 0.17 | 0.81 ± 0.14 | |
| Control | Dominant | 0.79 ± 0.18 | 0.82 ± 0.15 |
| Non-dominant | 0.82 ± 0.19 | 0.79 ± 0.12 |
The single-leg hop test did not reveal any differences between the ACLR and control subjects.
1.4
Discussion
Our main finding was that 2 years after ACLR, operated subjects had deficits in postural stability but no deficits in the hop test. To the best of our knowledge, there are few published studies of post-ACLR postural stability . Other researchers have evaluated static postural stability or/and dynamic postural stability . Our findings are in agreement with those of Tookuni et al. , who found that leg dominance does not significantly influence the balance of healthy individuals and that unilateral ACL damage affects the balance in single-foot stance on both sides (but is more obvious on the operated side).
Impaired postural stability has been demonstrated in ACL-deficient patients who complain of the knee “giving way”. Moezy et al. suggested that ACL injuries not only cause instability and disability in a high percentage of ACL-deficient athletes but also reduce proprioceptive ability and postural stability. Postural sway may be increased by proprioception loss in ACL injuries.
Post-ACLR proprioceptive impairments have been reported . In subjects 11 to 26 months postsurgery, Lephart et al. demonstrated a significant kinaesthetic impairment in the ACLR knee (compared with the non-operated knee), from a starting position of 15° and moving into both flexion and extension.
Knee stability depends on the interaction between the joint’s geometry, soft tissue resistance, body weight and applied muscle loads. Whereas bone structure and meniscal characteristics do not provide a high level of knee stability, the directional properties of ligaments, capsules and soft tissues all significantly contribute to this factor. Compressive forces (resulting from body weight and muscle activity) provide additional strength and prevent ligament overload when the knee is subjected to excessive loads during more aggressive activities .
In addition to the knee’s mechanical stability, nerve receptors within the joint also play a role. The neuromuscular control system sensors (mechanoreceptors), found in joints, skin and muscle inform the central nervous system of changes in position, motion perception and joint tension . Through the use of a specific training programmes, information from other knee structures can compensate for a lack of information from the ACL mechanoreceptors .
The ACL’s proprioceptive neurophysiological function has been considered to be as important as its biomechanical role in maintaining joint stability . Much research work suggests that the ACL receptors and the receptors in other knee structures have a fundamental role in maintaining the dynamic joint stability, based on existing reflex paths between the knee and the thigh muscle systems. In the studies by Zätterström et al. and O’Connell et al. , no differences were seen between injured limbs and non-injured limbs; the authors suggested that this was due to bilateral problems in individuals with a unilateral ACL injury. Likewise, Henriksson et al. did not see significant differences for ACLR patients. Hence, one should not necessarily consider the non-injured lower limb to be normal and the latter should not be neglected in rehabilitation programmes.
Zätterström et al. explained the balance problems in terms of “biomechanical factors” (such as muscle laxity or atrophy) and proprioceptive impairments in individuals with ACL injuries . The relative influences of biomechanical and proprioceptive factors were not evaluated in the present study.
Henriksson et al. noted that even in individuals with laxity on the injured side (compared with the non-injured side), there is no interleg difference in postural oscillation.
A system exhibiting a small excursion of the centre of mass (CoM) or CoP has been considered to be more stable than a system exhibiting a larger excursion . However, recent research has argued against this interpretation of postural instability. For example, ACL-deficient patients may exhibit less postural sway than healthy younger persons, under certain conditions. Measurements that examine only spatial aspects of postural movements may be inadequate for determining overall postural stability .
1.4.1
The single-leg hop for distance test
The single-leg hop for distance test was chosen as an objective functional measurement that would stress the knee joint while also allowing us to evaluate strength and confidence in the tested leg. Subjects having undergone ACLR hopped farther with the non-operated limb than with the operated limb but this difference was not statistically significant; this observation suggests that at an average of 24 months postreconstruction, this measure of functional performance was within the normal range.
Single-leg hop for distance scores are commonly expressed as a limb symmetry index, calculated as the mean score for the operated limb divided by the mean score for the non-operated limb and multiplied by 100.
Noyes et al. assessed the sensitivity of four types of single-leg hop tests (the single-leg hop for distance, the timed hop, the triple hop for distance and the crossover hop for distance) in a group of ACL-deficient patients. The authors considered a limb symmetry score below 85% to be abnormal. In a similar study, Wilk et al. examined the relationship between isokinetic testing and functional testing in a group of ACLR patients. They compared three functional tests: the single-leg hop for distance, the single-leg timed hop, and the single-leg crossover. We chose to assess only the single-leg hop for distance test because of time and fatigue considerations.
We did not find any difference between the single-leg hop scores on the operated and non-operated legs in the control group, which is consistent with Jerre et al. and Nyland et al. .
In summary, the difference in postural stability may be explained by the specific nature of the exercise and, possibly, by compensation by other lower extremity muscle groups. The ability to perform a single-leg hop seems to depend on the strength of the quadriceps muscle and requires coordinated activation of the lower leg muscle system . The single-leg hop requires maximal contraction of the supporting muscles.
1.4.2
Limitations
One limitation of our study was that it was not possible to account for differences in the subjects’ various rehabilitation programmes. All the ACLR subjects were asked to say how long they had participated in a physical therapy programme; the average time was 8 to 10 weeks. Hence, we could not account for the differences in rehabilitation programmes or check individual compliance with these programmes.
It would be interesting to further investigate postural stability and functional tests:
- •
before the reconstruction process;
- •
by control for the operated subjects’ rehabilitation after surgery.
1.5
Conclusion
After ACLR (mean time interval: 24 ± 1 months), subjects displayed a significant loss in single-limb postural stability when assessed with the NeuroCom “Balance Master” system. There was significant asymmetry between dominant and non-dominant limbs. It appears that the persistence of instability control was correlated with proprioception impairment.
The postural sway test with the Balance Master has been shown to be effective for measuring postural control in individuals with ACL injuries. Leg dominance does not influence postural control in young, healthy individuals. Use of the non-injured leg in individuals with unilateral ACL injuries as the control side should be considered with caution and should be taken into account in rehabilitation programmes.
2
Version française
2.1
Introduction
La rupture du ligament croisé antérieur (LCA) entraîne une instabilité mécanique et fonctionnelle . Pour les sportifs, la chirurgie est souvent indiquée .
La reconstruction du LCA induit de nombreux changements histologiques et physiologiques. Tous ces changements ont une influence sur la performance que les sportifs sont capables de fournir. Il a été démontré que la proprioception est perturbée se traduisant souvent par la perception de l’instabilité de l’articulation du genou et conduit à une diminution de la stabilité statique .
La rééducation postopératoire a pour objectif d’améliorer la stabilité dynamique et la restauration fonctionnelle du genou par le renforcement du contrôle neuromusculaire, réalisé par le travail de la force musculaire, la coordination et la sensibilité proprioceptive .
Le travail neuromusculaire avec des sujets victimes de la ligamentoplastie du LCA vise la sollicitation musculaire, l’amélioration de la stabilité dynamique et la reprise des mouvements utilisés au cours des activités quotidiennes et des activités sportives .
À la suite d’une déficience affectant unilatéralement les structures sensorimotrices impliquées dans la régulation de la station debout, cette symétrie risque d’être fortement perturbée .
La posture d’un individu est l’agencement des différents segments corporels les uns par rapport aux autres. La posture orthostatique étant la station debout érigée, position fondamentale de l’espèce humaine. L’équilibre est un état stable de la posture à un moment donné. C’est l’aptitude au maintien de la posture en dépit des circonstances (externes ou internes) qui tendent à la perturber , pouvant être évaluée en utilisant les mesures de l’équilibre postural .
Le besoin de mesurer quantitativement l’équilibre en appui monopodal ou bipodal et les répercussions de la ligamentoplastie du LCA du genou sur le contrôle postural est essentiel à l‘évaluation et le suivi des sportifs . Les progrès technologiques ont permis aujourd’hui d’évaluer le contrôle postural par l’exploration et la quantification des déplacements du centre de pression lors des différentes postures.
Neurocom Balance Master ® , utilisé initialement dans l’évaluation des troubles de l’équilibre d’origine neurosensorielle, s’est développé au cours des dernières années dans le but d’apporter à l’expertise clinique des éléments de mesure reproductibles des paramètres d’équilibration. Il permet d’étudier l’équilibre postural statique et de reproduire certaines situations dynamiques de la vie courante et de l’activité sportive basées sur la mise en charge et la décharge des membres inférieurs .
Le saut, permettant l’évaluation fonctionnelle, est un mouvement que l’on pratique régulièrement dans le sport et est également représentatif de la récupération de la fonction du membre inférieur . En effet, certains tests : saut, saut vertical, saut en longueur et one-leg hop permettent de quantifier les déficits fonctionnels entre membre sain et membre opéré chez des sportifs après reconstruction du LCA .
Le but de notre étude est l’évaluation posturale et fonctionnelle unilatérale chez des sportifs à deux ans de recul après reconstruction LCA.
2.2
Matériels et méthodes
2.2.1
Population
L’effectif total est au nombre de 52 sportifs répartis également en deux groupes. Un groupe expérimental (GLCA) ayant eu une ligamentoplastie du LCA par la technique Kenneth Jones (âge : 22 ± 3,11 ans, taille : 172,8 ± 4,17 cm, poids : 72,1 ± 7,15 kg) et un groupe contrôle (GC) (âge : 23,96 ± 2,02 ans, taille : 180,2 ± 0,06 cm, poids : 78,37 ± 9,58 kg) indemne de tout antécédents pathologiques articulaires ou musculaires au niveau des membres inférieurs.
Les sujets sont des sportifs évoluant dans la nationale A et suivant des entraînements quotidiens au sein de leurs clubs respectifs.
2.2.2
Critères de participation
Le groupe LCA est composé de sportifs selon les critères suivants :
- •
une rupture isolée du LCA ;
- •
l’absence de complication postopératoire ;
- •
pas d’antécédents de chirurgie ou une blessure traumatique au genou controlatéral ;
- •
pas d’antécédents chirurgicaux ou traumatiques de la cheville sur le côté opéré ;
- •
pas d’antécédents de chirurgie ou de traumatisme au niveau de la hanche ;
- •
pas de problème médical dans les six semaines avant l’évaluation ;
- •
un retour à leur niveau antérieur de la pratique sportive ;
- •
l’absence d’instabilité articulaire.
2.2.3
Procédures de l’évaluation
Les sujets sont soumis à deux types d’évaluations. Avant de commencer, les sujets ont rempli un formulaire de consentement. La passation des tests est randomisée. La session a débuté par cinq minutes d’échauffement suivi d’exercices de souplesse du bas du corps.
2.2.4
Balance Master ®
Description : le Balance Master ® fournit une évaluation objective du contrôle sensoriel et moteur volontaire de l’équilibre avec biofeedback visuel.
Le système utilise une double plate-forme de 18′′ × 60′′ pour mesurer les forces verticales exercées par les pieds lors de l’appui. Le test d’équilibre calcule la position du centre de pression relatif aux coordonnées de la plate-forme en utilisant la valeur de la taille du sujet testé. Puis il fournit une vitesse de balancement du centre de gravité en degré par seconde : plus cette vitesse est faible, plus le sujet est stable.
La technologie interactive et clinique des protocoles permet au clinicien d’évaluer objectivement les sujets accomplissant des tâches essentielles qui sont issues de l’activité de la vie quotidienne ou/et des compétences des activités sportives de haut niveau.
Ce système offre des protocoles d’évaluation qui quantifient l’impact des défaillances ou des pathologies articulaires sur des tâches nécessaires à la sécurité et l’efficacité motrice au cours de l’activité quotidienne. Tous les tests d’évaluation sont compatibles avec l’Organisation mondiale de la santé (ICDIH-2) et sont validés par des recherches scientifiques et cliniques.
Le système comprend une plate-forme de force liée à un microordinateur grâce à des capteurs. Il est composé de :
- •
d’une plate-forme de forces de forme rectangulaire (45 cm × 150 cm), détectant et mesurant les forces de réaction des pieds au sol dans les trois axes ;
- •
de quatre capteurs à jauges de contraintes ;
- •
d’un amplificateur pour les signaux analogiques recueillis à partir des capteurs.
Un ordinateur relié à la plate-forme de force permet d’analyser les données, de les traiter et de les stocker.
Plusieurs accessoires peuvent être associés (cube en bois ou en mousse, planches de différentes formes et hauteurs, plateaux instables) en fonction du type de l’épreuve.
Grâce au logiciel de traitement en liaison directe avec la plate-forme de force les données obtenues s’expriment pour la majorité des tests en termes de vitesse d’oscillation du centre de gravité exprimée en degrés par seconde.
Les tests débutent par l’installation du sportif sur la plate-forme ( Fig. 1 ). Le sujet se met debout sur la plate-forme en alignant chaque malléole interne avec les lignes larges et le bord postérieur du talon à la hauteur de la ligne appropriée.