Shoulder Injuries
Acute Injuries
5.1 Acromioclavicular Separation
Prim Care 2004;31:857; Clin Sports Med 2004;22:387; Phy Sportsmed 2001;29:31; Arch Fam Med 1997;6:376; Med Sci Sports Exerc 1998;30:S26
Cause: Fall or direct trauma.
Epidem: Common injury in tackling sports (football, soccer, rugby) or wrestling.
Pathophys: Tearing of acromioclavicular joint capsule and/or coracoclavicular ligaments (lateral conoid and medial trapezoid).
Classification:
Grade 1: AC pain without separation; no ligament disruption.
Grade 2: Mild separation; AC joint capsule torn, but coracoclavicular ligaments intact.
Grade 3: Severe separation; AC joint capsule and coracoclavicular ligaments torn.
Grade 4: Grade 3 tear of ligaments with distal clavicle posteriorly displaced into the trapezius.
Grade 5: Grade 3 with severe upward displacement of the distal clavicle.
Grade 6: Grade 3 with the distal clavicle inferiorly displaced and trapped under the coracoid.
Sx: Fall on shoulder with arm adducted (at side); pain in the AC area with or without deformity.
Si: Tenderness and soft-tissue swelling over the AC joint with or without deformity positive cross arm test.
Cross arm test: Patient standing or sitting, arm elevated 90° and internally rotated 90°, examiner forces the arm across the chest (adduction):
Positive Test = pain isolated to the AC joint
Crs: Self-limiting pain with residual deformity.
Cmplc: Stinger/Burner (see 4.4), clavicle fracture (see 5.2), rotator cuff tear (see 5.4), AC OA (see 5.5), suprascapular nerve injury.
Diff Dx: Clavicle fracture (see 5.2), coracoid fracture, rotator cuff tear (see 5.4), shoulder dislocation (see 5.3), AC OA (see 5.5).
Lab: Consider EMG if suspicious for nerve injury.
X-ray: May be done with or without suspended weights on the arm, rule out coexisting fracture.
Rx:
Initial: ice, pain medications (NSAID and narcotics), sling for comfort.
Start pendulum ROM activities as early as pain will allow.
Shoulder rehab as pain resolves.
Referral to orthopedics for Grade 4, 5, and 6 injuries, fracture of distal or medial third clavicle or humerus, or patient unwilling to accept cosmetic deformity.
Referral to physical therapy for rehabilitation pain modalities in acute and early recovery period. See 22.1 for rehab exercises.
5.2 Clavicle Fracture
Phy Sportsmed 2003;31:30; Phy Sportsmed 1999;27:119; Arch Fam Med 1997;6:376; Clin Orthop 1989;245:89
Cause: Fall onto shoulder with arm at side (adducted) or direct blow.
Epidem:
Common in tackling sports—football, soccer, rugby.
1:20 in all fractures.
44% of shoulder injuries.
25% related to athletic activities.
Pathophys:
80% fractures are the middle third
Distal ½ 12-15%
Medial 1/3 rare
Sx: Fall on shoulder or struck by object, audible pop with pain, deformity, and crepitus.
Si: Loss of motion, gross deformity of clavicle, palpable crepitus, r/o upper extremity neurovascular injury (Brachial Plexus).
Crs: Usually benign in middle third fractures; lateral and medial third fractures with high complication rate.
Cmplc: Brachial plexus injury, delayed or nonunion, open fracture, deformity.
Diff Dx: Grade 3-6 AC sprain with significant clavicular displacement (see 5.1), stinger/burner (see 4.4), coracoid fracture, acromial fracture, sternoclavicular joint subluxation.
X-ray: classify fracture as medial/lateral/mid third fracture.
Rx:
Figure-of-eight brace for 4-6 wk.
Pain control (NSAIDs and narcotics).
Shoulder ROM as tolerated early (pendulum exercises).
Rehab, as pain improves.
Referral to orthopedics for proximal or distal third fractures, non-union, evidence of neurovascular injury, patient unwilling to accept cosmetic deformity.
5.3 Anterior Shoulder Dislocation
Ortho Clin North Am 2002;33:479; Phy Sportsmed 2002;30:41; Arch Fam Med 1997;6:376; Clin Sports Med 1997;16:669; Orthopedic Sports Med. Philadelphia WB Saunders 1994:580
Cause: Fall or direct blow to shoulder.
Epidem: Anterior dislocation occurs 95% of the time and will be the focus of this discussion; posterior dislocations associated with trauma or seizure; M>F.
Pathopys: The size of the glenoid and humeral head and ROM of the shoulder make it inherently unstable; tear of inferior and middle glenohumeral ligaments and tear or stretch of anterior joint capsule; the “dislocating position” is abduction and external rotation.
Sx: Fall onto or blow to arm that is abducted and externally rotated; h/o prior dislocation.
Si: Arm usually held at side adducted and internally rotated; may see or palpate a large infraacromial sulcus; check distal pulses; check neuro status, especially the sensory distribution of the axillary nerve (posterior deltoid area sensation).
Crs: After reduction age <30 with >80% chance of recurrent dislocation; risk of recurrent dislocation in the >40 y/o group is low; it is common to have rotator cuff tears with older patients.
Cmplc: Instability (recurrent dislocation) (see 5.6); Bankart lesion; adhesive capsulitis (see 5.8); axillary nerve injury; Hill-Sachs lesion; missed diagnosis; unable to reduce.
Diff Dx: Humeral fracture, rotator cuff tear (see 5.4), impingement (see 5.7), deltoid strain, biceps tendon subluxation, posterior dislocation.
X-ray:
Axillary or scapular Y view to dx dislocation:
Scapular “Y” is a lateral x-ray of the shoulder with the arms of the Y formed by the lateral view of the scapular body, and the wings or upper arms by the scapular spine posteriorly and the coracoid anteriorly; the glenoid with the overlying humeral head will be in the center.
r/o Bankart lesion: glenoid avulsion fracture from the joint capsule being pulled off seen best in axillary or scapular Y views (it is possible to have a soft tissue Bankart which cannot be see on x-ray).
r/o Hill-Sachs lesion: posterior humeral head depression from local avascular necrosis due to single or multiple dislocations, seen best with Stryker Notch or axillary views.
Rx:
Reduction
Rockwood technique or traction/countertraction Countertraction with a towel or strap in the axilla and supported by assistant across the table; gentle traction with internal and external rotation; traction may be made easier by a strap or towel around waist and the patient’s elbow flexed to 90° then lean back to provide gentle traction.
Stimson technique or “Hang” method Hang 10-15 lb from arm with patient prone and arm hanging over edge of table; weight should be taped or
strapped to the arm; if the patient holds the weight, it may increase extremity muscle tone and hinder reduction; leave patient hanging over edge of table undisturbed for 20 min.
Self-reduction
Usually work better with recurrent dislocators.
Sedation: IV benzodiazepines (must monitor); 15-20 cc intra-articular lidociane 1%.
Check x-rays and neurovascular status after reduction: confirm reduction, look for Bankart lesion, eval axillary nerve function.
Pain control measures, ice and sling immobilization.
Immobilization for short time based on pain (1-2 wk).
Even shorter immobilization for older patients.
Begin rehab to strengthen RC as soon as possible; work on isometrics then isotonics (see section 5.4); motion and rehab in frontal plain or across chest is fine; avoid the abducted/externally rotated position (throwing position).
Referral to orthopedics for inability to reduce, patient <35 y/o (greater chance of repeat dislocation), fracture (humerus, distal clavicle, or Bankart), or recurrent dislocation.
5.4 Rotator Cuff Tear
Prim Care 2004;31:789; Arch Fam Med 1997;6:376; J Bone Joint Surg 1989;71-A:499; Am Fam Phys 1996;54:127
Cause: Fall onto shoulder or acute eccentric strain with lift.
Epidem: More common in the >50 y/o population presenting with shoulder pain.
Pathophys:
Then tendons of these muscles form a continuous hood over the humeral head; the SS is the major initiator of abduction and the infraspinatus and teres minor are external rotators (ER).
The RC functions as humeral depressor to keep humeral head in glenoid as power muscles (deltoid, pectoralis major, latissimus dorsi, teres major) move the arm in gross motions.
Weakness and degeneration of the RC (from disuse or sport/occupational overuse) allows upward movement of the humeral head impinging the RC and bursa between the humeral head and acromion.
Sx: History of a fall or lift causing a significant increase in pain and weakness; usually in the dominant arm; h/o shoulder pain with overhead motion of short or long duration; h/o frequent overhead activities.
Si: Limited motion from weakness or pain; tenderness over anterior rotator cuff (shoulder) area; weak supraspinatus and external rotators; positive impingement signs; may have a positive drop arm test.
Drop arm test:
Patient standing; full abduct the shoulder then have the patient slowly lower the arm.
Positive test = arm suddenly drops to side at about 90° abduction or inability to hold the arm at 90° abduction with minimal downward force applied by the examiner.
Supraspinatus (empty can test) (Figure 5.1)
Shoulder abducted 90°, forward flexed 30°, and internally rotated (thumbs down); patient resists downward direct force; compare to opposite side.
External rotation (teres minor and infraspinatus):
Arm at side and elbow flexed to 90°; patient resists inward directed force; compare sides.
Internal rotation (subscapularis, pectoralis major, latissimus dorsi, teres major):
Shoulder neutral and elbow flexed to 90°; patient resists outward direct force; hard to isolate the subscap.
Subscapularis lift-off:
Arm maximally internally rotated with back of palm resting in the lower lumbar area; pt attempts to lift the palm of the hand out away from the back against resistance; compare to opposite presumed normal side.
Bear hug (Subscap Test): (Phy Sportsmed 2004;32:19)
Patient places palm of affected arm on opposite shoulder. Examiner attempts to displace the palm anteriorly while the patient resists. Positive test indicated by inability to hold the palm on the opposite shoulder or weakness as compared to the opposite side.
Impingement test (Figure 5.2)
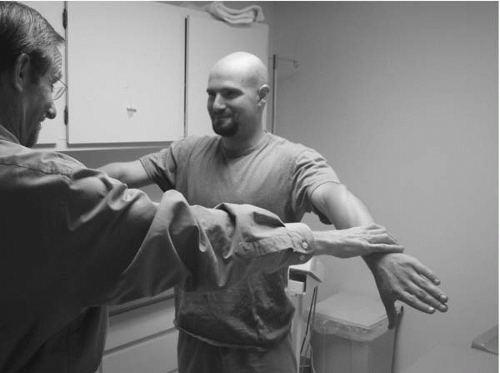 Figure 5.1 Supraspinatus Strength Testing
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




