Shoulder Arthrodesis
Robin R. Richards
INDICATIONS/CONTRAINDICATIONS
Shoulder arthrodesis can effectively restore function to patients with specific shoulder disorders. Patient selection is important in determining whether the procedure will be beneficial. Where a choice is possible, shoulder arthroplasty is preferable to shoulder arthrodesis, because arthrodesis results in the sacrifice of all glenohumeral rotation through the glenohumeral joint. Shoulders can be fused if an arthroplasty fails, although fusion in this situation is a technical challenge.
Paralysis of Both Deltoid and Rotator Cuff Muscles
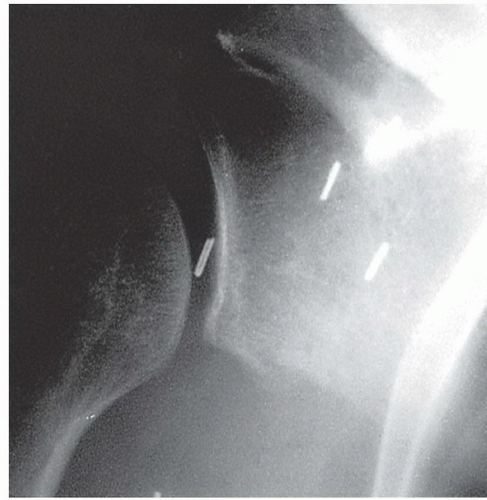
Experts agree that the presence of a flail shoulder is an indication for shoulder arthrodesis. Patients with anterior poliomyelitis, those with irreparable proximal root and upper trunk brachial plexus lesions, and some with isolated axillary nerve paralysis are candidates for shoulder arthrodesis. These patients often prefer to keep the arm in a sling to relieve discomfort and avoid injuring it (1). In a patient with the prerequisite good function in the periscapular musculature, particularly the trapezius, levator scapula, and serratus anterior, glenohumeral arthrodesis successfully stabilizes the extremity and allows effective hand function. A flail shoulder can also result in painful subluxation or instability that can be improved by arthrodesis (Fig. 42-1).
Doi et al. (2) reported on restoration of prehension with the double free muscle technique following complete avulsion of the brachial plexus and noted that secondary reconstructive procedures, such as arthrodesis of the carpometacarpal joint of the thumb, shoulder arthrodesis, and tenolysis of the transferred muscle and the distal tendons, were sometimes required to improve the functional outcome. El-Gammal et al. (3) used free-functioning gracilis transplantation combined with shoulder arthrodesis to restore function in pediatric patients with elbow and shoulder paralysis caused by poliomyelitis. Chammas et al. (4) found upper extremity function to improve after glenohumeral arthrodesis in two groups of patients with and without hand function. The author found that function following arthrodesis was improved in patients who had good hand function (5). Behdi et al. (6) recommended combining shoulder arthrodesis with aboveelbow amputation for the flail limb following complete posttraumatic brachial plexus injury. Wong et al. (7) reviewed their experience in six patients using shoulder arthrodesis as a secondary reconstructive procedure for patients with flail upper limbs following brachial plexus injury. Beaton et al. (8, 9) and Solomons and Cvitanich (10) discuss the one-stage shoulder arthrodesis and pectoralis major transfer for patients with upper brachial plexus injuries.
Axillary Nerve Paralysis
There is wide variability in the disability caused by axillary nerve paralysis. While muscle transfers may be available in carefully selected patients, and other patients may function quite well without any deltoid function, if there is significant limitation of shoulder function due to paralysis of the axillary nerve, arthrodesis should be considered.
Reconstruction After Tumor Resection
En bloc resection of periarticular malignant tumors often requires sacrifice of the rotator cuff, the deltoid, or both. In such cases, the outcome following reconstruction may be suboptimal. Kiss et al. (11)
reviewed 91 shoulder resections and found that the best results were achieved when the function of the rotator cuff was preserved. In some instances, arthroplasty with bone or soft-tissue allograft may be considered. However, arthrodesis is often a good solution for tumor reconstruction. Fuchs et al. reviewed functional outcomes after arthrodesis of the shoulder following tumor resection. There were no local recurrences and no patients developed metastatic disease. Arthrodesis provided good function independent of whether or not the procedure was performed as a primary or secondary procedure. Eight of the twenty-one patients (38%) had a complication (12). Macdonald et al. (13) discussed the use of CT scanning, solid modeling, and a free vascularized fibular graft for arthrodesis of the shoulder after excision of the upper humerus.
reviewed 91 shoulder resections and found that the best results were achieved when the function of the rotator cuff was preserved. In some instances, arthroplasty with bone or soft-tissue allograft may be considered. However, arthrodesis is often a good solution for tumor reconstruction. Fuchs et al. reviewed functional outcomes after arthrodesis of the shoulder following tumor resection. There were no local recurrences and no patients developed metastatic disease. Arthrodesis provided good function independent of whether or not the procedure was performed as a primary or secondary procedure. Eight of the twenty-one patients (38%) had a complication (12). Macdonald et al. (13) discussed the use of CT scanning, solid modeling, and a free vascularized fibular graft for arthrodesis of the shoulder after excision of the upper humerus.
Infection of the Glenohumeral Joint with Painful Incongruity
Although total shoulder replacement may be considered if the history of infection is remote, active or recent infection is better handled with a shoulder arthrodesis. Wick et al. (14) reported the long-term results after infection in 15 patients. Complications occurred in five patients. The complication rate was lower in patients less than 50 years of age and in those patients who had fewer than four previous operations (14).
Failed Total Shoulder Replacement
Although resection arthroplasty or revision may be considered if the patient is young, if there is history of infection, or if the bone stock is adequate, arthrodesis should be considered as a salvage procedure. Safran and Iannotti (15) discuss the need for various bone grafting techniques, including the use of the vascularized fibular bone graft to reconstruct bone deficiency. In another publication, Scalise and Iannotti (16) reviewed seven patients who had arthrodesis following failed prosthetic shoulder arthroplasty. Four of the seven patients had undergone additional bone grafting procedures in order to obtain union. The results of the study suggested that arthrodesis could achieve satisfactory clinical outcomes and that the patient should be aware of the frequent need for additional surgical procedures to obtain fusion. Barker et al. (17) reported complete bony union after arthrodesis of the native glenoid and acromion to an allograft proximal humerus. Tsukushi et al. (18) reported on the use of a clavicular rotation graft for revised shoulder arthrodesis after tumor resection of the proximal humerus.
Failure of Previous Repairs for Shoulder Instability, Particularly Multidirectional Instability
Occasionally, after multiple repairs, a patient will present with uncontrollable shoulder instability, particularly global laxity and multidirectional instability (19). If attempts at soft-tissue stabilization were satisfactory, but there is still symptomatic uncontrollable instability, shoulder arthrodesis can be considered as a means to stabilize the shoulder. Diaz et al. (20) report arthrodesis to be a viable treatment option for this group of patients. The author will consider arthrodesis for such patients if secondary osteoarthritic changes have begun to develop
in the glenohumeral joint. These patients, however, may continue to experience problems and may not function at as high a level as other patients undergoing arthrodesis.
in the glenohumeral joint. These patients, however, may continue to experience problems and may not function at as high a level as other patients undergoing arthrodesis.
Failed Rotator Cuff Surgery, Especially if Accompanied by Deltoid Inadequacy or Excessive Acromial Excision
The combination of a massive rotator cuff deficiency, deltoid insufficiency, and an acromial excision is virtually insolvable with repeated rotator cuff surgery and is often associated with the development of secondary osteoarthritic change in the glenohumeral joint (21, 22). Glenohumeral arthrodesis may provide these patients with a comfortable arm and glenohumeral stability, particularly if the patient is sufficiently symptomatic to exchange the loss of glenohumeral motion for the relief of pain.
Contraindications
Shoulder arthrodesis should be reserved for those situations that are not amenable to reconstruction by any other means. Many patients are amenable to arthroplastic reconstruction that preserves glenohumeral motion and has greater potential to restore function (23, 24, 25). The primary contraindications to shoulder arthrodesis include a progressive neurologic disorder with paralysis of the trapezius, levator scapula, and serratus and a contralateral shoulder arthrodesis. In addition, because shoulder arthrodesis requires a major effort by the patient to rehabilitate the shoulder, this procedure is contraindicated in a patient who cannot cooperate with such a program. I have not performed shoulder arthrodesis on elderly patients for this reason.
Alternative Techniques
The author’s practice is limited to the treatment of adults. In pediatric patients, where it is desirable to preserve growth, alternative surgical techniques to that described in this chapter may be considered (26). For instance, Mohammed (27) reported on the use of a Rush pin introduced from the spine of the scapula through the glenoid into the medullary canal of the humerus to perform shoulder arthrodesis. Mohammed supplemented this fixation with tension band wiring from the acromion to the neck of the humerus and a muscle pedicle graft attached to the acromion. Furthermore, a shoulder spica was applied for 4 to 6 weeks. Mohammed used this method on four patients with upper brachial plexus injuries and found that it did not affect bone growth in young patients, was effective in patients with osteoporosis, and gave a high rate of union. Kocialkowski and Wallace (28) reported on the use of an external fixator to obtain shoulder arthrodesis. Syal and MacDonald (29) reported on the use of arthroscopy to perform shoulder arthrodesis in two cases.
PREOPERATIVE PLANNING
The typical patient requiring shoulder arthrodesis complains of flail shoulder, symptomatic instability, and inability to use the elbow or hand because the shoulder cannot be stabilized. Unless there is a severe brachial plexus injury involving paralysis more distally, the functioning of the elbow and hand is often remarkably good. Examination of the shoulder may reveal atrophy of the deltoid or of the infraspinous or supraspinous fossae. The humeral head may be subluxated inferiorly at rest. Often, there is excessive mobility of the humeral head in the glenoid. In the absence of glenohumeral arthritis, the range of passive motion is often normal, especially in those patients undergoing arthrodesis for paralysis. Muscle testing reveals weakness of internal and external rotators of the shoulder, and weakness or paralysis of the deltoid muscle. In those patients who present for tumor reconstruction, failure of prior rotator cuff or instability surgery, failed arthroplasty, or distant glenohumeral joint infection, the physical examination is usually specific for those conditions. Standard radiographs ordered are anteroposterior, lateral, and axillary views of the glenohumeral joint, giving the surgeon information about the presence or absence of arthritis, any developmental abnormalities of the shoulder, and the adequacy of bone stock if internal fixation is to be used in the surgical arthrodesis. Occasionally, if the neurologic condition of the shoulder girdle muscles is in doubt, an electromyogram of the deltoid, rotator cuff, or scapular muscles may be indicated.
Before shoulder arthrodesis, preparations by the patient, the operating room staff, and the hospital’s rehabilitation personnel are necessary. Patients require some understanding of the operative technique and some insight into how glenohumeral arthrodesis can improve function and increase motion in the presence of a flail shoulder. The concept of the procedure is difficult for many patients. The most practical way to help them understand is to have them speak to a patient who has undergone the procedure. I attempt to provide the patient with the name of a former patient of the same sex, a similar age, and a similar diagnosis.
Shoulder arthrodesis requires a full set of the usual shoulder surgery instruments. In addition, pelvic reconstruction plates are used together with fully threaded cancellous screws (30). Plate-bending devices are required to contour the plate to the specific local anatomy of the individual patient. Curved osteotomes are used for decorticating the surfaces of the glenoid and humeral head and the undersurface of the acromion. Decortication of both the acromial humeral and the glenohumeral surfaces to increase the surface area available for arthrodesis is helpful in achieving solid arthrodesis. The operating room table must be adjustable so that the patient may be placed in a semisitting position intraoperatively. Although there are numerous methods for stabilization of a shoulder arthrodesis, the most popular method today is probably the AO technique with either a single plate or double plate (31).
Postoperative management requires the use of a thermoplastic orthosis appliance suspended from the opposite shoulder, although Riggins (32) has reported, from a small series of patients, that external immobilization is not needed after shoulder arthrodesis with plate fixation. In our institution, these appliances are custommade for each patient and this can be a time-consuming task. Accordingly, the rehabilitation personnel must be aware of the anticipated postoperative requirements of the patient in advance. It is sometimes expeditious to construct the thermoplastic orthosis appliance on the afternoon before or on the morning of surgery so that only minor adjustments are needed in the immediate postoperative period. This can be helpful in reducing patient discomfort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree