Shoulder Arthritis
Eric T. Ricchetti
Gautam P. Yagnik
CLINICAL PRESENTATION
Glenohumeral arthritis occurs in up to 20% of adults and is much less common than arthritis of the knee or hip. The most common etiology of glenohumeral arthritis is osteoarthritis, but other diseases, such as rheumatoid or inflammatory arthritis, osteonecrosis, rotator cuff tear arthropathy, and posttraumatic or postsurgical arthritis, can also be a cause.1,2,3
The different etiologies of glenohumeral arthritis may dictate potentially different treatment options. Pain in the affected shoulder is the most common presenting complaint in patients with glenohumeral arthritis. Shoulder stiffness is also a frequent problem, and patients may note a sensation of crepitus with shoulder movement. Symptoms usually begin gradually and are chronic and progressive. Discomfort is typically worsened with activity, and patients may awaken at night from pain, particularly if they sleep on the affected shoulder.1 Functional limitations may be evident, including an inability to perform overhead activities or reach behind the back or under the opposite axilla with the affected arm.3
In documenting the patient’s history, it is important to characterize the onset and duration of symptoms, as well as the degree of functional limitation and the patient’s activity level.4 All prior treatment modalities, including physical therapy regimens, nonsteroidal anti-inflammatory medications, injections, and operative procedures on the shoulder should be documented. Additionally, obtaining the patient’s overall past medical history can provide information about disease severity or predisposing factors for glenohumeral arthritis, such as a history of steroid use in rheumatoid arthritis patients or radiation exposure in patients with osteonecrosis of the humeral head.1,4
CLINICAL POINTS
The condition occurs much less frequently than arthritis in the knee or hip.
Pain is the most common presenting complaint.
Onset is gradual and becomes chronic.
History may provide important clues.
PHYSICAL FINDINGS
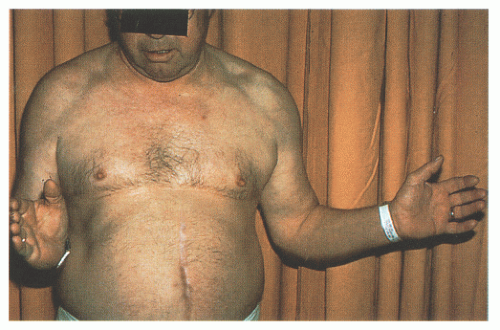
The physical examination should help in confirming or refuting the initial diagnosis that is made on the basis of the patient history. A careful examination of the cervical spine should first be performed to rule out any abnormalities, including radiculopathy and degenerative joint disease that may cause referred pain, stiffness, or weakness in the shoulder. The affected shoulder is then inspected for any prominence, atrophy, or asymmetry compared to the contralateral side, as well as prior surgical scars. Mild shoulder atrophy may be present from disuse. More significant atrophy may be noted along the supraspinatus or infraspinatus fossa if a large rotator cuff tear is also present. Shoulder palpation is performed to define areas of tenderness. Although this is often nonspecific, glenohumeral joint line tenderness is typical with arthritis, either anteriorly or posteriorly. Anterior and lateral tenderness may be more frequently seen in inflammatory arthritis.1 Muscle strength as well as range of motion are also assessed. Range of motion of the shoulder is performed actively and passively and compared to the asymptomatic side. Both active and passive motion are typically restricted in glenohumeral arthritis, usually in multiple planes. Decreased external rotation is commonly seen in osteoarthritis from chronic stiffness and anterior capsular contracture (Fig. 41-1).4
Specific patterns of restricted motion may also be related to prior trauma or surgery, such as a loss of external rotation in patients with previous surgical stabilization for anterior shoulder instability. Pain and crepitus in the glenohumeral joint may be elicited with active or passive motion.3 Muscle strength testing should assess the rotator cuff, deltoid, and other shoulder girdle muscles.4 Evidence of rotator cuff muscle weakness may be pain related or could be evidence of significant rotator cuff pathology, particularly if lag signs are present.
STUDIES (LABS, X-RAYS)
Lab Studies
Laboratory studies are generally not helpful in the diagnosis of glenohumeral arthritis unless septic shoulder is a concern.
Radiographic Evaluation
Plain radiographs are the initial imaging study of choice. Radiographs should include a true anteroposterior (AP) view (Fig. 41-2) and an axillary lateral view (Fig. 41-3) to best see the classic features of arthritis.
Osteoarthritis will typically show joint space narrowing, osteophyte formation, sclerosis, and subchondral cysts, while rheumatoid arthritis will show joint space narrowing, osteopenia, bony erosions, subchondral cysts, and occasionally osteophyte formation.2,3 Loose bodies may also be seen, typically in the axillary pouch. The axillary lateral view is particularly important in assessing the degree of joint space narrowing and the amount and location of glenoid erosion.3
Radiographs may also be helpful in identifying other shoulder abnormalities, such as osteoarthritis of the acromioclavicular joint, calcific tendinitis, and os acromiale.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree