This article reviews the incidence, management, and complications of scoliosis in patients with cerebral palsy. Treatment of scoliosis in patients with cerebral palsy includes both nonoperative and operative management and often the decision to proceed with surgery is a multidisciplinary decision. Because of severe spasticity, many of these patients undergo intrathecal baclofen pump placement before, during, or after posterior spinal fusion. The complication rates can be high with intrathecal baclofen pump placement, but many patients can have significant benefit with this therapy.
Key points
- •
The incidence of scoliosis in patients with cerebral palsy is high, particularly in those with more involvement.
- •
Because of severe spasticity, many patients with cerebral palsy undergo intrathecal baclofen pump placement before, during, or after posterior spinal fusion.
- •
Despite high complications, it seems equally safe to place intrathecal baclofen pumps before, during, or after spinal fusion.
Introduction
Patients with cerebral palsy (CP) commonly develop scoliosis. The treatment of scoliosis in these patients can be different from treatment of the idiopathic scoliosis population. Management of the spinal deformity in CP can be challenging and often presents the surgeons and caregivers with many difficult decisions and obstacles. The approach to the care of these children should be multidisciplinary in order to optimize outcomes and decrease the frequent complications.
Introduction
Patients with cerebral palsy (CP) commonly develop scoliosis. The treatment of scoliosis in these patients can be different from treatment of the idiopathic scoliosis population. Management of the spinal deformity in CP can be challenging and often presents the surgeons and caregivers with many difficult decisions and obstacles. The approach to the care of these children should be multidisciplinary in order to optimize outcomes and decrease the frequent complications.
Cerebral palsy and scoliosis
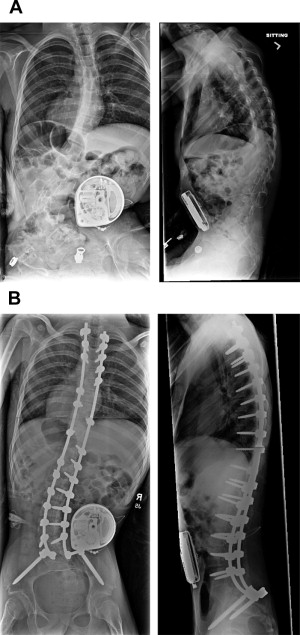
The neuromuscular scoliosis that occurs in CP is typically a C-shaped curve that is often kyphoscoliotic and is associated with pelvic obliquity ( Fig. 1 ). Children with CP have an increased risk of developing scoliosis compared with other patient populations. Muscle weakness, truncal imbalance, and asymmetric tone in paraspinal muscles have long been implicated for the onset of scoliosis in CP, but there is little literature to support this theory.
The prevalence of scoliosis in a total population of children with CP is nearly 30%. Curves tend to begin at an earlier age than in idiopathic scoliosis. They are more likely to progress even after the patient reaches skeletal maturity. There is also an increased incidence of increased Gross Motor Function Classification System (GMFCS) level. Children with GMFCS level IV and V CP have a 50% risk of moderate or severe scoliosis by the age of 18 years.
Studies have found correlation between the size of the deformity and the decline in functional activities. Majd and colleagues found an increased curve progression in patients with a decline in function compared with patients who were functionally stable. They also found that patients developing decubitus ulcers with prolonged sitting were more likely to have larger curves.
Scoliosis treatment in cerebral palsy
Nonsurgical Treatment
Nonoperative treatment of scoliosis in patients with CP consists of:
- •
Observation
- •
Seating modifications
- •
Bracing
Observation can be chosen for curves of any size or magnitude. Reasons for continued observation are numerous. The curve size may be of insufficient magnitude to require surgical treatment. In addition, family decisions may be made to avoid operative management or other nonoperative modalities because of various comorbidities or after weighing the risks and benefits.
Molded wheelchair inserts can be used to attempt to improve overall sitting balance. Three-point force configuration support systems have been shown to achieve the best static correction of the scoliosis. However, there is no evidence that this alters the natural history. Modifications of the wheelchair should be individually tailored to the patient.
Bracing goals for CP are often different from the goals in idiopathic scoliosis. There is little evidence that bracing slows curve progression, but there are many studies that show no significant effect of bracing. The goals of bracing are to maintain comfortable, upright sitting, allow functional use of the upper extremities, and allow maximum ability to interact with the environment. Soft braces seem to be tolerated better than rigid orthoses in patients with spastic CP. Soft braces maintain skin integrity and potentially minimize respiratory compromise.
Surgical Treatment
Goals, indications, and benefits of surgery, as well as the risk and potential complications, must be carefully weighed with the patient’s family. There is no absolute indication of surgery ( Box 1 ).
| Goals of Surgery | Relative Surgical Indications for Spinal Fusion |
|---|---|
| Improve coronal and sagittal balance Improve sitting balance Halt progression of scoliosis Level pelvis Improve positional discomfort | Progression of Cobb angle >50° Deterioration in functional sitting Age >10 years, with adequate hip range of motion to allow seating, stable nutritional, and medical status |
For patients undergoing surgery, a thorough preoperative assessment is required. Assessment needs to include pulmonary function, nutritional status, gastrointestinal evaluation, and neurologic function.
Pulmonary function testing is not easily performed in this patient population, but evaluation with a chest radiograph is often necessary. Patients with poor nutrition (serum albumin <35 g/L and total blood lymphocyte count <1.5 g/L) are known to have increased postoperative infection rate, longer length of intubation, and longer hospital stays. Nutrition may need to be optimized with nutritional supplementation or even a G-tube placement. From a gastrointestinal standpoint, assessment for gastroesophageal reflux and aspiration risk is needed because these patients are at risk for aspiration pneumonia.
In addition, seizure disorders should be controlled, and the medications used to control the condition should be noted. Some medications, such as phenytoin, phenobarbital, and valproic acid, can cause reduced bone mineral densities. Valproic acid has also been implicated for increased intraoperative blood loss and the need for blood transfusions.
The technical aspects of surgery for spinal fusion are beyond the scope of this article. There have been major advancements from a surgical standpoint from Luque rods, Luque rods with Galveston technique, unit rod fixation, Cotrel-Dubousset and Isola instrumentation, and more recently pedicle instrumentation. Pedicle instrumentation has been shown to have improved curve correction rates, lowest loss of correction, and greatest apical vertebral translation.
The complication rate in the perioperative period for these patients is nearly 30%. Patients with CP undergoing surgery for spinal deformity are at high risk for complications secondary to medical comorbidities. Reames and colleagues and Hod-Feins and colleagues found surgical complications rates to be much higher among this patient population compared with the rates in idiopathic scoliosis. Perioperative complications including delayed extubation and length of hospital stay are significantly higher in neuromuscular scoliosis compared with idiopathic scoliosis. This difference is likely directly related to longer surgeries, higher blood loss, and other medical comorbidities such as seizure disorders.
Major complications in the postoperative period have also been described. Death is reported in 0% to 7% of patients. Sponseller and colleagues reported a deep infection rate of 6% and superficial rate of 4%. Deep infections in patients with CP are often polymicrobial with gram-negative organisms. Pseudoarthrosis rates have decreased over time from the use of Harrington rods (as high as 40%) to Luque instrumentation (0%–13%) to more recent fixation with pedicle instrumentation (1%) ( Box 2 ).
| Perioperative Complications | Postoperative Complications |
|---|---|
| Death Neurologic complications Respiratory distress, atelectasis, pneumonia Delayed extubation Gastric distension, ileus, obstruction Seizures Blood loss Hemodynamic instability | Death Superficial/deep infections Pseudoarthrosis Implant failure |
Outcomes of spinal fusion are difficult to assess in this patient population because there is still no adequate outcome tool to adequately assess improvement in function. Cassidy and colleagues showed no clinically significant differences in pain, pulmonary medication need, decubitus ulcers, function, or time for daily care in patients who underwent spinal fusion compared with those who had not. In contrast, Larsson and colleagues evaluated patients 1 year after surgery and found improvement in curve size and sitting balance. Multiple studies have shown high satisfaction in parents and caregivers after surgery. Based on a caregiver questionnaire, Watanabe and colleagues found improvements in sitting balance (93%), cosmesis (94%), and quality of life (71%).
Scoliosis, spinal fusion, and intrathecal baclofen pumps
Indications/Benefits of Intrathecal Baclofen Pumps
Intrathecal baclofen (ITB) is approved for treatment of spasticity related to several disorders including CP. It inhibits both monosynaptic and polysynaptic reflexes at the spinal cord level thus decreasing excitatory neurotransmitter release from primary afferent terminals to decrease spasticity. Penn and Kroin first reported its use for severe spasticity with immediate reduction of muscle tone to near-normal levels. The efficacy of ITB in children with CP is well documented. Multiple studies have shown improvement in patients with CP. Gooch and colleagues showed improved satisfaction of care providers, ease of care, and decreased pain. Other studies have also found improved ease of care and others have shown improved gait in ambulatory patients with CP. In addition, Gerszten and colleagues showed a decreased need for subsequent orthopedic surgery for lower extremity spasticity. The indications for implantation of ITB pumps are primarily for intractable spasticity ( Box 3 ).
| Indications for ITB Pump Therapy | Benefits of ITB Pump Therapy |
|---|---|
| Intractable spasticity Uncontrollable spasticity with drug therapy Intolerable side effects to oral baclofen | Improved spasticity Improved range of motion Improved ease of care Improved pain Increased caregiver satisfaction Improved hygiene, transfers Improved gait |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




