Abstract
Osteoarthritis (OA) is one of the most common joint disorders worldwide. Its prevalence is increasing because of the growing aging of the population in developed and developing countries as well as an increase in risk factors leading to OA, particularly obesity and a sedentary lifestyle. Risk factors of OA can be divided into person-level factors (age, gender, obesity, genetics and diet) and joint-level factors (injury, malalignment and abnormal loading of the joints) that interact in a complex manner. OA is the 11th cause of disability in the world. It is responsible for activity limitations, particularly walking, and affects participation and quality of life. Patients with OA are at greater risk of all-cause mortality, particularly for cardiovascular diseases, than the general population. This excess mortality is closely associated with disability level. Consequently, strategies to reduce burden through primary and secondary prevention programs are increasingly important.
1
Introduction
Osteoarthritis (OA) is one of the most common joint disorders worldwide ; it typically affects knees, hips, hands, spine, and feet . The prevalence and incidence rates reported in epidemiological studies vary widely, because the estimates depend on the definition of cases (pathological, radiographic or clinical OA), the population sampled (primary versus tertiary care, developed versus developing countries), and the joint(s) involved .
Radiographic OA is mainly assessed by the Kellgren and Lawrence score, which grades the severity of the disease from 0 to 4 by the appearance of osteophytes, joint space loss, sclerosis and cysts. These criteria were adopted by the World Health Organisation (WHO) to define radiographic OA in epidemiologic studies .
Clinical OA is defined by the history and the examination. Several standards have been proposed for the diagnosis of clinical OA; the most recognized may be the criteria of the American College of Rheumatology .
There is a strong dissociation between radiographic findings and clinical symptoms: for example, only 40% of patients with moderate radiographic knee OA and 60% of those with severe knee OA have symptoms . The diagnosis of symptomatic radiographic OA has been developed to take into consideration both structural change and joint symptoms.
Consequently, when interpreting results of epidemiological studies, the setting of the study, the definition of cases and the method of data collection must be kept in mind. Here we summarize the risk factors and burden of OA.
2
Prevalence and incidence of OA
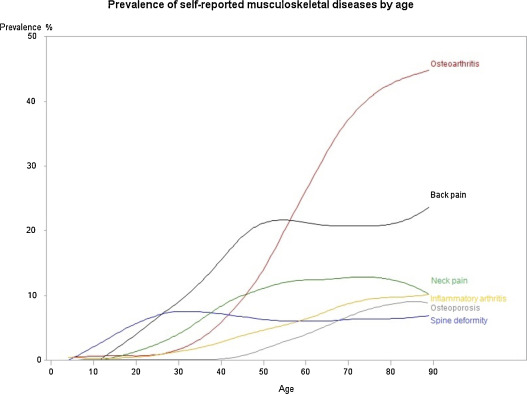
In the literature, the prevalence of OA ranges from 12.3% (self-reported in the “Disability-Health” 2008 population-based survey in France) to 21.6% (physician-diagnosed OA in the United States estimated by the 2003–2005 US National Health Interview Survey). The disease is more common in women than men . It increases with age, occurring after the age 40 to 50 years ( Fig. 1 Fig. 1 ), and is greater in developed than developing countries , although in certain countries such as Iran, the prevalence was high in rural areas (knee OA: 19.3% according to the COPCORD study) .
The incidence of OA is high as well. A recent Spanish study investigating > 3 million subjects reported incidence rates of clinically defined OA of 6.5, 2.1, and 2.4/1000 person-years for knee, hip, and hand, respectively , which is higher than the rates found in older studies .
2.1
Hip and knee OA
According to the 2010 WHO Global Burden of Disease Study, the global prevalence of radiographically confirmed symptomatic knee OA in 2010 was estimated at 3.8% (95% uncertainty interval [95% UI] 3.6–4.1%) . Hip OA is less common. The global age-standardized prevalence of symptomatic radiographically confirmed hip OA in 2010 was 0.85% (95% UI 0.74% to 1.02%). There was no evidence of a change in age-standardized prevalence between 1990 and 2010, for hip or knee OA . This finding is surprising and contrasts with other international and national reports that concluded an increasing incidence of knee or hip OA . In fact, the growing age of the population in developed and developing countries as well as increased risk factors for OA, particularly obesity and a sedentary lifestyle, suggested that the number of people living with hip or knee OA will increase substantially over the coming decades . The results of the 2010 WHO study could be explained by the modeling process itself or by an insufficient period of data collection (20 years could be insufficient to detect a difference) .
2.2
Hand OA
The prevalence of radiographic hand OA ranges from 27% to 80% . Two large national surveys were conducted (the Zoertermeer Survey in The Netherlands and the Framingham survey in the United States). In the Zoertermeer Survey, 10% to 20% of patients < 40 years old showed a radiographic change in hands or feet and 75% of women 60 to 70 years old had radiographic hand OA in the distal interphalangeal joints . Data from the Framingham cohort demonstrated a prevalence of 13.2% in men and 26.2% in women ≥ 70 years old with at least one hand joint with symptomatic OA .
Symptomatic hand OA is far less common. Its prevalence was found to be 8% in the US National Health and Nutrition Examination Survey (NHANES III) and 7% in the Framingham cohort .
2
Prevalence and incidence of OA
In the literature, the prevalence of OA ranges from 12.3% (self-reported in the “Disability-Health” 2008 population-based survey in France) to 21.6% (physician-diagnosed OA in the United States estimated by the 2003–2005 US National Health Interview Survey). The disease is more common in women than men . It increases with age, occurring after the age 40 to 50 years ( Fig. 1 Fig. 1 ), and is greater in developed than developing countries , although in certain countries such as Iran, the prevalence was high in rural areas (knee OA: 19.3% according to the COPCORD study) .
The incidence of OA is high as well. A recent Spanish study investigating > 3 million subjects reported incidence rates of clinically defined OA of 6.5, 2.1, and 2.4/1000 person-years for knee, hip, and hand, respectively , which is higher than the rates found in older studies .
2.1
Hip and knee OA
According to the 2010 WHO Global Burden of Disease Study, the global prevalence of radiographically confirmed symptomatic knee OA in 2010 was estimated at 3.8% (95% uncertainty interval [95% UI] 3.6–4.1%) . Hip OA is less common. The global age-standardized prevalence of symptomatic radiographically confirmed hip OA in 2010 was 0.85% (95% UI 0.74% to 1.02%). There was no evidence of a change in age-standardized prevalence between 1990 and 2010, for hip or knee OA . This finding is surprising and contrasts with other international and national reports that concluded an increasing incidence of knee or hip OA . In fact, the growing age of the population in developed and developing countries as well as increased risk factors for OA, particularly obesity and a sedentary lifestyle, suggested that the number of people living with hip or knee OA will increase substantially over the coming decades . The results of the 2010 WHO study could be explained by the modeling process itself or by an insufficient period of data collection (20 years could be insufficient to detect a difference) .
2.2
Hand OA
The prevalence of radiographic hand OA ranges from 27% to 80% . Two large national surveys were conducted (the Zoertermeer Survey in The Netherlands and the Framingham survey in the United States). In the Zoertermeer Survey, 10% to 20% of patients < 40 years old showed a radiographic change in hands or feet and 75% of women 60 to 70 years old had radiographic hand OA in the distal interphalangeal joints . Data from the Framingham cohort demonstrated a prevalence of 13.2% in men and 26.2% in women ≥ 70 years old with at least one hand joint with symptomatic OA .
Symptomatic hand OA is far less common. Its prevalence was found to be 8% in the US National Health and Nutrition Examination Survey (NHANES III) and 7% in the Framingham cohort .
3
Risk factors of OA
The risk factors of OA can be divided into person-level factors, including age, gender, obesity and genetics and diet, and joint-level factors, including injury and abnormal loading of the joints . Knee malalignment is the strongest predictor of progression of knee OA.
3.1
Person-level risk factors
3.1.1
Age
Age may be the main risk factor of OA . The suspected mechanism leading to joint damage is poorly understood but is probably multifactorial (including oxidative damage, thinning of cartilage, muscle weakening, and a reduction in proprioception) .
Sarcopenia itself may be an independent risk factor of knee OA but could also participate in its progression . In fact, quadriceps weakness has been observed in patients with symptomatic knee OA; it could be due to atrophy with disuse, but data suggest an arthrogenous inhibition of muscle contraction. This weakness also results in a lack of stability and should be specifically managed during rehabilitation programs.
3.1.2
Gender
The prevalence of hip, knee and hand OA is higher in women than men, and the incidence increases around menopause . Several authors have suspected a role of hormonal factors in the development of OA. However, results are conflicting , and the difference between men and women could be explained by other factors (reduced volume of cartilage, bone loss or lack of muscle strength) .
3.1.3
Obesity
Obesity, defined as body mass index (BMI) > 30 kg/m 2 , is strongly associated with knee OA (pooled odds ratio [OR] in a recent meta-analysis including 22 studies: 2.66 [95% CI 2.15–3.28]), whereas the relationship between overweight (BMI > 25 kg/m 2 ) and knee OA is lower but still significant (pooled OR 1.98 [95% CI 1.57–2.20]) . Several authors showed a dose–response relationship between obesity and risk of knee OA: for every 5-unit increase in BMI, the associated increased risk of knee OA was 35%, with the magnitude of the association significantly stronger for women than men .
Silverwood et al. estimated that in patients with new-onset knee pain, 24.6% of cases were related to overweight or obesity . Several studies showed that weight loss improved pain and function and decreased low-grade inflammation . The Framingham Study estimated that weight reduction by 5 kg decreased the risk of developing knee OA by 50% .
Obesity is also associated with hand OA (OR 2.59 [95% CI 1.08–6.19]) , so the impact of obesity may not be just biomechanical but also has some metabolic and inflammatory systemic effects. This hypothesis is reinforced by recent literature showing an association between OA and metabolic syndrome .
The relationship between body weight and hip OA is inconsistent and weaker than with knee or hand OA .
3.1.4
Genetics
Genetic factors account for 60% of hand and hip OA and 40% of knee OA. Many genes could play a role in the disease onset and so could provide targets for future pharmacological treatments (e.g., genes encoded for vitamin D receptor, insulin-like growth factor 1, type 2 collagen, growth differentiation factor 5) .
3.1.5
Diet
Several dietary factors suspected to increase the development of OA include a low level of vitamins D, C and K . However, further studies are needed to better define the association between OA and these dietary factors.
3.2
Joint-level risk factors
Injury: the knee is one of the most frequently injured joints. The rupture of the anterior cruciate ligament (ACL) leads to early-onset knee OA in 13% of cases after 10 to 15 years. When such rupture is associated with damaged cartilage, subchondral bone, collateral ligaments and/or menisci (observed in approximately 65–75% of ACL-injured knees), the prevalence of knee OA is higher, between 21% and 40% .
ACL surgical reconstruction improves joint stability, but it may not prevent knee OA in the long term, nor protect the knee from re-injury or restore normal knee kinematics as compared with conservative treatment . Patients who undergo ACL reconstruction have poorer outcomes if the injury is associated with a meniscal tear, even if they undergo a meniscal repair or a meniscal resection at the same time . Meniscal repair is the treatment of choice for young athletes with an acute meniscal tear , but its efficacy for OA onset is unknown. Total meniscectomy has been found detrimental to the knee joint in that radiographic OA was estimated to be 14 times more common in people 20 years after undergoing total menisectomy as compared with controls . Arthroscopic partial meniscectomy was not efficacious as compared with sham surgery for people with degenerative meniscal tears without OA and could participate in the development of OA.
3.3
Abnormal loading of joints
Data suggested that repetitive joint use was associated with the development of OA. Knee OA was more frequently observed in people with occupations that required squatting and kneeling, whereas hip OA was associated with prolonged lifting and standing , and hand OA was more frequent in people with occupations requiring increased manual dexterity .
The relationship between physical activity and OA is complex and is developed in another part of this special issue. Briefly, highly repetitive, intense and high-impact physical activity seems to confer increased risk of developing radiographic hip and knee OA as compared with controls, but whether this association is due to only sports participation or results from injury is unclear .
4
Malalignment
Abnormal alignment is strongly associated with increased structural degradation in the compartment under the greatest compressive stress . Cerejo et al. showed that medial progression of knee OA was four-fold greater in patients with varus alignment and lateral progression five-fold greater in those with valgus alignment . The association between malalignment and OA onset is less apparent .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






