This retrospective, consecutive case series of a single surgeon performed between 2001 and 2010 assesses the outcome following revision of metal-on-metal hip resurfacing arthroplasties (N = 113). Mean time to revision was 31 months (0–101) after primary hip resurfacing. Malpositioning of the components with associated wear-induced soft tissue fluid collections was the most frequent factor leading to failure of a hip resurfacing arthroplasty. The mid-term outcome of the revisions was satisfactory; complications occurred in 11 patients (9.7%). Six of these patients underwent a re-revision.
In the last 15 years, metal-on-metal hip resurfacing arthroplasty (MoMHRA) has been used in increasing numbers to treat hip pathologies especially in young and active patients, with an estimated 500,000 third-generation MoMHRA performed to date. Arthroplasty registries have reported inferior survivorship of certain hip resurfacing designs, recently leading to the withdrawal of the Articular Surface Replacement (ASR) design (DePuy, Warsaw, IN) from the market. Besides these reports, increasing numbers of revisions for unexplained pain and soft tissue reactions have been published, potentially alerting the attitudes of the orthopedic community, health authorities, and the public toward MoMHRA. Although global consensus exists regarding the importance of implant design and indications for MoMHRA, the methods to follow-up MoMHRA patients differ. More specifically, the measurement of metal ions in the peripheral blood has been recognized as a valuable and necessary tool to recognize increased wear of the articulating surfaces at an early stage, and can be used as a screening method.
Ease of revision with minimal bone loss has been put forward as a theoretical advantage of hip resurfacing. Isolated failure of the femoral resurfacing component was safely and successfully converted to total hip arthroplasty (THA) in one series. Another series highlighted the difference in outcome with different indications for revision. Cases revised for fracture, avascular necrosis (AVN), or component loosening, that is, mechanical failures without soft tissue damage, had better outcome and lower complication rates compared with cases with pseudotumor and extensive soft tissue destruction.
A review of 397 revisions of MoMHRA from the Australian Joint Replacement Register (AJR), comparing survival as a mode of outcome for different types of MoMHRA revisions, confirmed that the best outcome was achieved with either femoral-only revision or revision of both components. However, even femoral-only revisions had twice the risk of revision of a primary THA. Acetabular-only revisions were reported to have a high risk of re-revision in the AJR, with a 5-year cumulative revision rate of 20%.
The aim of this retrospective, consecutive case series of a single surgeon was to assess the outcome following revision of MoMHRA. In addition, the authors assessed whether the lessons learned from the initial previously reported experience improved outcome, and whether screening with the use of metal ions had an effect on post-revision outcome.
Patients and methods
Between November 2000 and September 2010, the senior surgeon (K.A.DeS.) performed 113 consecutive revisions of failed metal-on-metal hip resurfacing arthroplasties in 110 patients. There were 3 bilateral revisions and 2 re-revisions of hip resurfacings where initially only the acetabular component had been revised. Of the primary 113 hip resurfacing procedures, 70 had been performed elsewhere and 43 by the senior surgeon (K.A.DeS.). The initial operations were performed between June 1996 and December 2009.
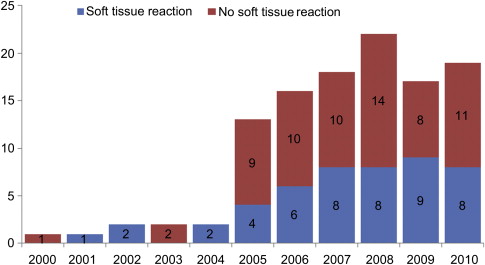
The number of revisions of hip resurfacings is increasing as more HRA are being implanted worldwide. In the authors’ center, the number of revisions has risen from an average of 2 cases per year during the period of 2000 to 2004 to an average of 17 per year in the period 2005 to 2009 ( Fig. 1 ).
Patient Demographics
There were 44 male patients (40%) undergoing 45 revisions (1 re-revision) and 66 female patients (60%) undergoing 70 revisions (3 bilateral revisions and 1 re-revision) ( Table 1 ). The mean age of the patients at the primary hip resurfacing operation was 49.9 years (range 14–71 years) and their mean age at the revision was 52.5 years (range 18–71 years). Forty-three of the primary MoMHRA were performed at the authors’ center (38%). A total of 3313 MoMHRAs have been performed since 1998, resulting in a known revision rate of 1.5% (patients revised at this center and reported from elsewhere). The remaining 70 failed MoMHRAs (62%) were from elsewhere, with patients having had their primary surgeries in 50 different centers in 6 different countries.
| Number of revisions: N = 113 | Bilateral revisions: n = 3 Re-revisions: n = 2 | — | |
| Patients: N = 110 Males: n = 44 (40%) Females: n = 66 (60%) | 44 revisions (1 re-revision) 69 revisions (3 bilateral, 1 re-revision) | — | |
| Mean age at primary surgery Mean age at revision surgery | 49.9 y (14–71) 52.5 y (18–71) | — | |
| Primary diagnosis: N = 111 Re-revision: 2 cup revisions | Osteoarthritis: n = 95 (85.8%) Congenital hip dysplasia: n = 7 (6.2%) Avascular necrosis: n = 8 (7.1%) Rheumatoid arthritis: n = 1 (0.9%) 1 cup loosening, 1 head loosening | — | |
| Types of hip resurfacing: N =113 | Overall number | KADS: N = 43 | % of total number by KADS 43/3313 resurf = 1.3% |
| BHR | n = 61 (55.8%) | n = 31 | 31/1967 BHR = 1.6% |
| McMinn | n = 2 (1.8%) | — | — |
| Conserve® Plus | n = 19 (16.8%) | n = 8 | 8/1055 = 0.8% |
| Conserve® Plus A-Class® | n = 1 (0.9%) | n = 1 | 1/122 = 0.8% |
| ASR | n = 10 (8.8%) | n = 2 | 2/66 = 3.0% |
| DUROM | n = 10 (8.8%) | — | — |
| ADEPT | n = 4 (3.5%) | — | — |
| CORMET 2000 | n = 3 (2.6%) | — | — |
| RECAP | n = 3 (2.6%) | n = 1 | 1/18 = 5.6% |
| — | 2 re-revisions of BHR resurfacings | ||
The original diagnosis was osteoarthritis in 97 cases (85.8%), congenital hip dysplasia in 7 females (6.2%), avascular necrosis in 8 cases (7.1%) including 4 males and 4 females, and rheumatoid arthritis in 1 male patient (0.9%).
Revised Hip Resurfacing Types
The consecutive series of 113 revised hip resurfacing arthroplasties consisted of 63 Birmingham Hip Resurfacings (BHR) (Smith & Nephew, Memphis, TN, USA), 2 McMinn (Corin, Cirencester, UK), 19 Conserve® Plus (Wright Medical Technology, Arlington, TN, USA), 1 Conserve® Plus A-Class® (Wright Medical Technology), 10 ASR (DePuy, Warsaw, IN, USA), 10 DUROM (Zimmer, Winterthur, Switzerland), 4 ADEPT (Finsbury Orthopaedics, Leatherhead, UK), 3 CORMET 2000 (Corin), and 3 RECAP (Biomet, Warsaw, IN, USA) hip resurfacing arthroplasties (see Table 1 ). Two BHR had to be re-revised. Primary hip resurfacing procedures by the senior surgeon (K.A.DeS.) included 31 BHR, 8 Conserve® Plus, 1 Conserve® Plus A-Class®, 2 ASR, and 1 RECAP (see Table 1 ). The mean interval between the primary hip resurfacing operation and the first revision was 30.9 months (range 0–101 months). The 2 cases of re-revision were conducted at 22 and 27 months after the first revision.
Diagnostic Tools
The diagnostic assessment of patients with a painful or failed hip resurfacing included plain anteroposterior and false-profile standing radiographs, clinical examination and scoring (Harris Hip Score [HHS] ), and serum metal ion measurements (Chromium [Cr] and Cobalt [Co]) done routinely since 2005/2006. Metal ion measurements were performed at the Laboratory for Toxicology of the University of Ghent, Belgium. Levels higher than 5.1 μg/L for Cr and 4.4 μg/L for Co were considered to be elevated and possibly associated with clinical problems due to increased wear of the components (De Smet KA, Campbell PA, van Orsouw M, et al. Interpretation of metal ion levels after metal-on-metal resurfacing. Poster presentation at the America Academy for Orthopaedic Surgeons. New Orleans [LA], March 2010, unpublished data). The radiographs were analyzed for acetabular and femoral component positioning with inclination and anteversion angles, femoral neck fracture or progressive neck narrowing, component migration or subsidence, and radiolucent lines, osteolytic lesions, or signs of bone remodeling. To assess the position of the acetabular components accurately and objectively, an EBRA analysis (Einzel Bild Roentgen Analyze, University of Innsbruck, Innsbruck, Austria) was performed by an independent reader (G.G.), who measured both the cup inclination and version angles. Optimal placement of the acetabular component was defined an inclination of 45° and an anteversion of 20°. A “safe zone” was defined as a zone of ± 10° about the optimum orientation. Components placed outside the safe zone were considered to be malpositioned.
When an infection or a soft tissue reaction was suspected, additional investigations were performed, including total body bone scans and granulocyte scans to investigate a possible infection, and ultrasonography and/or magnetic resonance imaging to look for cysts or soft tissue masses. Retrieved periprosthetic tissues were sent to an independent laboratory for retrieval analysis, histologic examination, and ALVAL (Aseptic Lymphocytic Vasculitis Associated Lesions) scoring.
Surgical Procedures
During the revision operation, a posterolateral approach was used for 110 interventions and an anterolateral for 3 ( Table 2 ). Whenever possible, it was attempted to preserve well-fixed, well-positioned acetabular and femoral components. When the acetabular component had to be revised, it was carefully removed with chisels to minimize loss of bone stock. Encapsulated fluid collections and metal-stained, damaged periprosthetic tissues were excised completely in the early revisions. With increasing experience, however, dissection was done with the utmost care to preserve as much muscle and soft tissue as possible to sustain the stability of the hip. Among the 113 hip resurfacing revisions, 10 (8.8%) were cup-only, 22 (19.5%) were femoral component-only revision, and the remaining 81 (71.7%) had both components revised. A ceramic-on-ceramic hybrid total hip replacement was used in 11 cases (9.7% of total revisions) with an uncemented acetabular component. Seventy-one uncemented total hip replacements were performed, 5 had Big Femoral Head metal-on-metal (MoM) bearings, and the remainder were ceramic-on-ceramic (CoC). The head diameters of the revision hips ranged from 28 to 58 mm with a mean diameter of 39.8 mm (median 36 mm).
| Type of Revision Procedure | Number |
|---|---|
| Cup-only | n = 10 (8.8%) |
| Femoral stem with Big Femoral Head metal-on-metal | n = 22 (19.5%) |
Total hip revision
| n = 81 (including 2 re-revisions) (71.7%) n = 11 (9.7%) |
| n = 70 (61.7%) n = 5 n = 65 |
| Head diameters of revision components | Mean 39.8 mm (28–58) |
| 28–36 mm ceramic head | n = 58 (51.3%) |
| 38–58 mm ceramic or metal head | n = 55 (48.7%) |
Following the initial experience there was a difference in surgical practice. There were significantly fewer cup-only revisions (7 vs 3) ( P <.001), a greater number of uncemented, titanium, THA stems were implanted ( P <.001), and bigger THA femoral heads were used ( P = .01).
Postoperative Care
Postoperative rehabilitation and thromboprophylaxis were performed following a routine hip arthroplasty protocol. Patients with a revision to a total hip replacement in whom both the acetabular and femoral component had been revised with decrease of the femoral head size, and patients in whom the hip capsule and soft tissue had been removed due to extensive metallosis and tissue necrosis, were asked to wear an antidislocation hip abduction brace for 6 weeks. This measure was taken following 5 cases of dislocation after hip resurfacing revisions in the early series, of which the results have been reported. All revised patients are reviewed clinically and radiographically at 6 weeks and subsequently at 1, 2, and 5 years postoperatively.
Outcome Measures
Patient-reported clinical outcome was assessed with the harris hip score (HHS). HHS was obtained prior to revision and at clinical reviews. The change in HHS (ΔHHS) between preoperative and latest follow-up was defined as: ΔHHS = HHS follow-up − HHS pre-revision .
The mean follow up after revision was 43 months (range 3–121 months).
Data were collected prospectively for all cases. Complications and re-revisions were recorded.
Analyses
Outcome was compared for gender, revision type, and operative findings, more specifically the presence or absence of soft tissue fluid collections.
Analysis was also performed for different subgroups: the first 42 cases, previously reported, comprised the Initial Group, the initial experience of revisions of failed hip resurfacings. Cases from 43 onwards formed the Later Group.
Patients with metal ion levels used as a diagnostic tool formed the Ions-measured Group (n = 74) and the outcome of these patients were compared with the outcome of patients without ion levels (Ions-not-measured Group, n = 36).
Nonparametric statistical tests were used to analyze HHS, femoral head size, time to revision, and so forth. The Chi-squared test was used for complication and re-revision rates. Significance was considered when P values of less than .05 were obtained; all statistical analyses were performed using SPSS (version 18, IBM SPSS, Chicago, IL, USA).
Results
Reasons for Revision
One hundred and six patients (109 hips) presented with some degree of pain or discomfort in the hip region, often associated with mechanical symptoms such as impingement or limited range of motion, and in a few cases also with a swelling around the groin ( Table 3 ). Four patients had no pain symptoms. The mean HHS before revision was 70.4 points (range 25–100). Elevated metal ion levels with or without radiographic signs of failure were an indication for revision in cases without clinical symptoms. Overall the metal ions levels were elevated in 40 patients (54.1%). The mean Cr levels were 22.39 μg/L (range 0.5–146.0 with a median of 7.40 μg/L) and the mean Co levels 22.42 μg/L (range 0.5–119.0 with a median of 4.40 μg/L). In the 40 patients with high metal ions, impingement was established intraoperatively in 11 cases (27.5%), metallosis in 36 cases (90%), and an adverse soft tissue reaction in 32 cases (80%).
| Preoperative Reason for Revision | Number and Percentage |
|---|---|
| More than 1 reason | n = 19 (16.5%) |
| Cup malpositioning | n = 57 (49.6%) |
| Cup loosening | n = 15 (13.0%) |
| Head malpositioning | n = 11 (9.6%) |
| Head loosening | n = 21 (18.3%) |
| Osteolysis | n = 57 (49.6%) |
| Fracture | n = 6 (5.2%) |
| Infection | n = 6 (5.2%) |
| Mismatch | n = 1 (0.9%) |
| High metal ions (measured since 2005–6) | n = 40 (34.8%) |
| Pain | n = 19 (16.5%) |
| Pain as only reason | n = 1 (0.9%) |
| Intra- and Postoperative Findings | Number and Percentage |
| Osteolysis | n = 33 (28.6%) |
| Neck narrowing | n = 20 (17.4%) |
| Impingement | n = 39 (33.9%) |
| Oversized components | n = 4 (3.5%) |
| Metallosis | n = 37 (30.8%) |
| Soft tissue fluid collection | n = 48 (42.5%) |
| Metal sensitivity | n = 6 (5.2%) |
The most common indication for revision was a symptomatic patient with a malpositioned cup (n = 68 cases, 60%). The most common radiological finding was osteolysis (n = 57, 50.4%), noted either as progressive neck narrowing, as radiolucent lines around the components, or as osteolytic lesions. Metal ions above the safe levels of 5.1 μg/L Cr or 4.4 μg/L Co (De Smet KA, Campbell PA, van Orsouw M, et al. Interpretation of metal ion levels after metal-on-metal resurfacing. Poster presentation at the America Academy for Orthopaedic Surgeons. New Orleans [LA], March 2010, unpublished data) were found in 40 patients (54.1% of all metal ion measurements). In 3 cases (2.6%) high metal ion levels were the primary reason for revision. Fifteen of the 48 soft tissue fluid collections (31.3%) were encountered with cups positioned in the safe zone. Six of those were found to be related to metal sensitivity (1 bilateral) and 3 to femoral component loosening; 6 others had high metal ions with or without signs of neck narrowing or impingement.
Surgical Observations
The most common intraoperative findings were a cystic soft tissue reaction (n = 48, 42.5%) and impingement (n = 37, 30.6%) (see Table 3 ). Cystic soft tissue fluid collections ( Fig. 2 ) around the hip were seen with all designs. The 3 female patients with bilateral revisions had bilateral soft tissue reactions. Soft tissue collections were associated with less soft tissue destruction in the Later Group.








