The reverse shoulder arthroplasty is considered to be one of the most significant technological advancements in shoulder reconstructive surgery over the past 30 years. It is able to successfully decrease pain and improve function for patients with rotator cuff–deficient shoulders. The glenoid is transformed into a sphere that articulates with a humeral socket. The current reverse prosthesis shifts the center of rotation more medial and distal, improving the deltoid’s mechanical advantage. This design has resulted in successful improvement in both active shoulder elevation and in quality of life.
Key points
- •
The reverse shoulder replacement changes the position of the normal shoulder joint by placing a sphere on the glenoid that articulates with a humeral socket.
- •
The reverse prosthesis provides a medial and distal fixed axis of rotation that improves deltoid function.
- •
Inferior glenosphere placement with inferior tilt, lateralizing the center of rotation, and a more varus humeral component may improve impingement, free range of motion, and minimize scapula notching.
- •
Appropriate deltoid tensioning decreases the risk for postoperative instability, nerve palsy, or acromial stress fractures.
- •
Focusing the postoperative rehabilitation on strengthening the anterior deltoid and pectoralis major can increase arm flexion, whereas strengthening the posterior deltoid in abduction increases external rotation.
Introduction
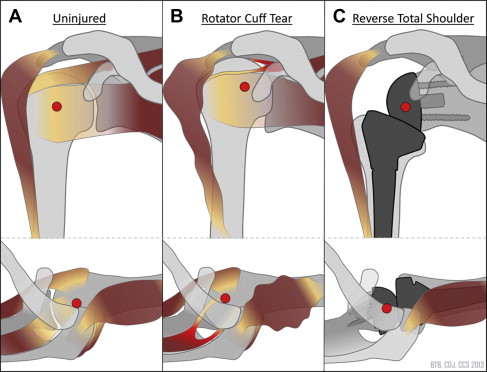
The reverse shoulder arthroplasty (RSA) has revolutionized reconstructive shoulder surgery. Secondary to promising clinical results, the reverse shoulder prosthesis has generated a great deal of enthusiasm in a relatively short period of time. Initially recommended for patients with rotator cuff arthropathy, surgeons have expanded its application to massive cuff tears without arthritis, fracture care, rheumatoid arthritis, and failed prior surgery replacements with a high level of success. An RSA flips the normal shoulder ball and socket anatomy. The design of the reverse prosthesis places the ball in the socket position and conversely positions the socket in the ball position. This stabilization design results in a semiconstrained prosthesis that stabilizes the glenohumeral center of rotation analogous to a functioning rotator cuff ( Fig. 1 A–C). This effectively prevents superior migration of the humerus on the glenoid and thereby maintains the deltoid muscle’s resting length (see Fig. 1 C). The deltoid muscle, now restored to its anatomic resting length, can compensate for the rotator cuff deficiency. The RSA commonly provides rotator cuff patients with significant improvement in forward elevation and decrease in pain. Several clinical studies have reported considerable enhancement in activity and quality of life following a successful RSA. In fact, patients following an RSA resume an activity level similar to patients’ activity level after a traditional hemiarthroplasty or total shoulder replacement. The commonly reported activities starting from low and progressing to high demand included cooking, baking, driving, gardening, leaf raking, lawn mowing, snow shoveling, wheelbarrow use, and shoveling dirt. Although extensive long-term data are not available, short to intermediate outcome studies suggest that the survivorship of the reverse shoulder implant is comparable with hemiarthroplasty and total shoulder replacements.
Introduction
The reverse shoulder arthroplasty (RSA) has revolutionized reconstructive shoulder surgery. Secondary to promising clinical results, the reverse shoulder prosthesis has generated a great deal of enthusiasm in a relatively short period of time. Initially recommended for patients with rotator cuff arthropathy, surgeons have expanded its application to massive cuff tears without arthritis, fracture care, rheumatoid arthritis, and failed prior surgery replacements with a high level of success. An RSA flips the normal shoulder ball and socket anatomy. The design of the reverse prosthesis places the ball in the socket position and conversely positions the socket in the ball position. This stabilization design results in a semiconstrained prosthesis that stabilizes the glenohumeral center of rotation analogous to a functioning rotator cuff ( Fig. 1 A–C). This effectively prevents superior migration of the humerus on the glenoid and thereby maintains the deltoid muscle’s resting length (see Fig. 1 C). The deltoid muscle, now restored to its anatomic resting length, can compensate for the rotator cuff deficiency. The RSA commonly provides rotator cuff patients with significant improvement in forward elevation and decrease in pain. Several clinical studies have reported considerable enhancement in activity and quality of life following a successful RSA. In fact, patients following an RSA resume an activity level similar to patients’ activity level after a traditional hemiarthroplasty or total shoulder replacement. The commonly reported activities starting from low and progressing to high demand included cooking, baking, driving, gardening, leaf raking, lawn mowing, snow shoveling, wheelbarrow use, and shoveling dirt. Although extensive long-term data are not available, short to intermediate outcome studies suggest that the survivorship of the reverse shoulder implant is comparable with hemiarthroplasty and total shoulder replacements.
Can an RSA replace the rotator cuff?
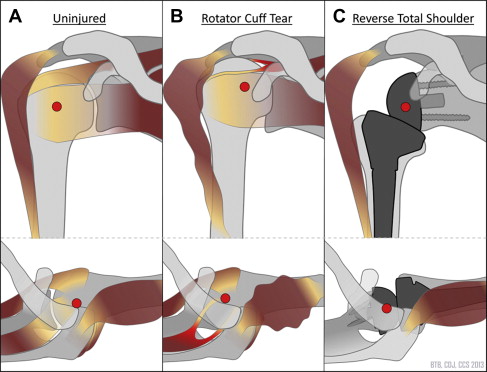
The minimally constrained nature of the native shoulder joint allows a nearly limitless possible array of arm positions. The rotator cuff muscles play a key role in accomplishing this balance between mobility and stability. For most day-to-day activities, patients typically need the ability to elevate their arm approximately 120° in front of their body as well as 120° out to the side ( Fig. 2 ). Internal and external rotation of the shoulder are also required for many activities of daily living (ADLs). Most ADLs require approximately 60° of shoulder external rotation, particularly when the elbow is away from the body, like washing ones hair, and 100° degrees of internal rotation when the arm is by one’s side, such as putting on a belt, fastening a bra, or reaching to one’s back pocket.
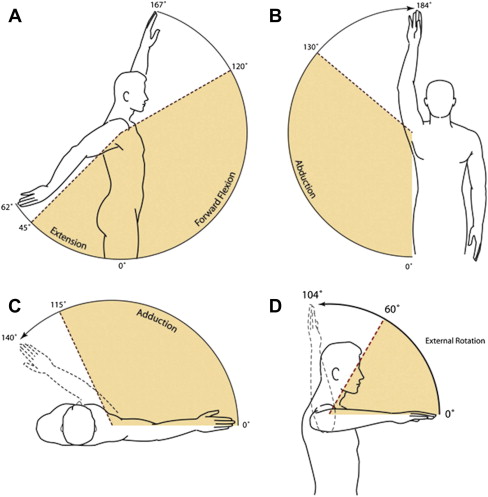
When the rotator cuff is no longer functional, patients can lose this ability to actively elevate their shoulders to 90°; this loss of motion has been coined pseudoparesis ( Fig. 3 A ). Following a reverse shoulder replacement, most patients regain the ability to elevate their shoulder again with minimal discomfort (see Fig. 3 B, C). Postoperatively, studies have shown that patients can anticipate approximately 120° to 150° of active shoulder forward flexion and abduction with restoration of many ADLs. In contrast to shoulder elevation, improvement of shoulder external and internal rotation can be limited following an RSA. Studies have shown minimal improvement in shoulder external rotation (as little as 2° to up to 31° postoperatively). Thus, the RSA cannot completely replace the native functional rotator cuff.
How does it work?
In the normal shoulder, the rotator cuff muscles provide a dynamic balanced force couple that keeps the humeral head centered on the glenoid socket throughout all ranges of motion (see Fig. 1 A). The glenohumeral joint is balanced in the axial plane by the subscapularis, anteriorly, and the infraspinatus and teres minor, posteriorly. The supraspinatus completes the balanced compressive force in the coronal place and counteracts the deltoid vector of pull to keep the humeral head center. These axial and coronal force couples maintain a stable center of rotation, allowing the deltoid to efficiently provide a rotary force to elevate the arm with power and direction. The rotator cuff also plays a pivotal role in initiating shoulder abduction as well as controlling the needed internal and external rotation to position the hand in space. When the rotator cuff function is compromised, such as with a massive tear, this normal balanced compressive force is lost. In this scenario, the deltoid losses its mechanical advantage and ability to provide a rotation torque to the arm (see Fig. 1 B). Consequentially when patients attempt to elevate their arm, the deltoid pulls the humerus proximally, rather than rotating it, and leads to the classic shoulder shrug ( Fig. 4 ). Overtime, this eccentric load across the shoulder joint results in superior glenohumeral instability, pathologic articulation of the humeral head with the acromion, and arthritis ( Fig. 5 ).


The RSA directly addresses the altered kinematics of the rotator cuff deficient shoulder. The reverse ball and socket is a semi-constrained implant that provides a new fixed center of rotation. Most modern reverse shoulder replacements medialize and distally place the center of rotation to a certain degree. This modification improves both the deltoid’s moment arm (the mechanical advantage) and tension while decreasing the amount of force required for abduction (see Fig. 1 C). Research has shown that the RSA decreased the force required for abduction by approximately 30%. Additionally, the change in the deltoid’s vector of pull allows it to recruit more anterior and posterior fibers for flexion and abduction. These changes significantly improve the deltoid’s ability to raise the arm. This biomechanical effect is also particularly important during the initiation phase of arm elevation. In the native shoulder, the rotator cuff supraspinatus tendon plays a key role in initiating shoulder elevation. Following the RSA, the deltoid is now better suited to initiate shoulder abduction even without a functional supraspinatus.
Design features that impact outcome
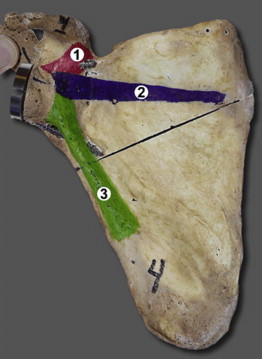
The reverse shoulder replacement consists of 3 main components: the baseplate, the glenosphere, and the humeral socket ( Fig. 6 A–F ). The baseplate is a metal-backed plate that directly contacts the glenoid. Varying design options of the baseplate include a flat or convex radius of curvature. The convex baseplate improves bony contact, whereas a more flat baseplate, depending on the design, may actually preserve more bone stock during reaming and implantation. The convex baseplate design may also transmit a more compressive force (as opposed to a shear force) at the baseplate-bone interface. Modern baseplates are secured to the glenoid with cementless fixation but are coated on the backside to allow bony ingrowth. The baseplate is typically stabilized to the glenoid via a press-fit central post, keel, or central screw. Depending on the implant design chosen, up to 6 peripheral nonlocking or locking screws can be used for added compressive fixation strength, which has been shown to minimize the baseplate-glenoid micromotion and encourages bony ingrowth. This modern baseplate design has minimized the risk for premature baseplate failure. Some implants allow the peripheral baseplate screws to be freely redirected to locations within the scapula of increased bone stock. If variable angle screws are used, the screws should be directed to 1 of 3 columns: the base of the coracoid, the scapula spine, and/or down the lateral scapula pillar ( Fig. 7 ). The Tornier Aequalis (Tornier, Inc Bloomington, MN), the Depuy Delta XTEND (Depuy, Inc Warsaw, IN) and the Trabecular Metal Reverse (Zimmer, Warsaw, IN) systems all provide baseplates with a central post (see Fig. 6 A–F). All 3 systems allow multiple peripheral screws to augment fixation. The Reverse Shoulder Prosthesis (DJO, LLC, Vista, CA) has a baseplate with a central 6.5 mm cancellous screw. The technique allows bicortical fixation of the central screw when directed to exit along the medial anterior cortex of the scapula. In this system, 4 additional peripheral locking screws promote secure fixation of the baseplate. The Exactech Equinoxe Reverse Shoulder’s baseplate (Exactech, Inc Gainesville, FL) provides a unique central post cage that secures in the glenoid vault and encourages bony ingrowth, whereas the Comprehensive (Biomet, Inc, Warsaw, IN) has a central boss that accepts a 6.5 modular central screw. There is no clear clinical data that compares the durability of the different baseplate designs. It is the authors’ opinion that they are all very similar, and the patients’ scapular anatomy and the surgeon’s comfort level should decide whether one design should be used over another.
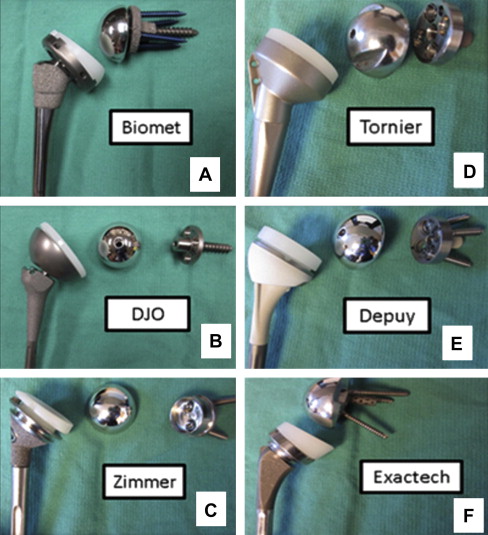
The glenosphere (see Fig. 6 A–F) secures into the baseplate and becomes the new articulating ball. Glenosphere options vary in shape and design. Depending on the design chosen, they can place the new center of rotation directly on the glenoid surface or further lateral, closer to the native shoulder. The Tornier Aequalis, Exactech Equinoxe, and Depuy Delta XTEND place the center of rotation at the surface of the glenoid. The DJO Reverse, Biomet Comprehensive, and Zimmer Trabecular Metal reverse implants allow the surgeon the option of shifting the center of rotation further lateral away from the glenoid with a built-in offset. The further away the center of rotation is placed from the glenoid surface, the higher the shear force at the glenoid/baseplate interface. Studies have shown that with modern fixation techniques, the increase in micromotion is minimal even when the center of rotation is placed up to 10 mm away from the glenoid surface. Although the Exactech Equinoxe places the center of rotation at the glenoid surface, it lateralizes the humerus instead via a larger glenosphere and offset humeral socket, which, in theory, improves the deltoid’s moment arm while allowing more room for impingement-free range of motion. Eccentric glenospheres are also available that allow controlled distal placement of the center axis without compromising the location of bone fixation.
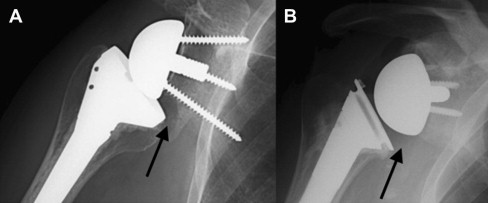
The humeral socket (see Fig. 6 A–F) is the opposing articulating surface for the glenosphere. Varying thickness and offset options for the humeral socket can be used as needed to elongate the deltoid, lateralize the humerus, and achieve the desired soft tissue tension. The humeral socket engages into a humeral stem that can be cemented or press fit into the humeral canal. Secondary to the medialized center of rotation, semiconstrained design, and limited space available for motion, the humeral socket is at risk of impinging with the scapula as it articulates with the glenosphere. If the humeral socket is allowed to repetitively abut the scapula neck with the use of the artificial shoulder, bony erosion can take place (ie, scapula notching) ( Fig. 8 A ). The humeral socket-shaft angle can vary between approximately 130° to more than 150° depending on the implant chosen. The more valgus (∼150°–155°) humeral socket increases the deltoid tension by lengthening the acromion-humeral distance, which has been shown to improve active forward flexion and implant stability. The more varus (∼130°–140°) humeral socket more closely matches the native anatomic head neck angle. This varus angle seems to better minimize scapula notching (see Fig. 8 B). The Tornier and Depuy reverse implants have a more valgus humeral socket-shaft angle, whereas the DJO, Zimmer, Biomet, and Exactech reverse implants have a more varus humeral socket-shaft angle.
Surgical techniques that impact outcome
The current designs of the RSA are unable to completely compensate for all function lost in the rotator cuff–deficient shoulder. Following an RSA, improvement in external rotation of the shoulder varies considerably from patient to patient and depends on how much of the infraspinatus and teres minor (ie, external rotators) remain intact. The medialization of the center of rotation, although improves elevation, limits the ability of the anterior and posterior deltoid fibers to contribute to internal and external rotation. Researchers recently found that the RSA results in a considerable decrease in the ability of the deltoid and the remaining intact rotator cuff to contribute to shoulder external rotation. Some current surgical techniques and implant designs attempt to offset this effect by minimizing the amount of medialization that occurs. A lateralized center can be performed by either building out the glenoid with a bone graft or using a prosthesis with a built-in lateral center of rotation. In theory, this allows the anterior and posterior deltoid fibers as well as the remaining intact rotator cuff to preserve their internal and external rotary line of pull. Clinical results seem to support this concept by showing improved patient shoulder external rotation following the placement of a reverse prosthesis with surgical techniques that push the center of rotation further lateral. However, lateralizing the center of rotation may not necessarily increase the activity level or variety of activities patients perform after an RSA. Clear conclusive evidence on the benefit of lateralization is still somewhat elusive.
Preservation of the remaining rotator cuff, tendon transfers, and changing humeral version are other techniques to increase rotational motion and strength. The surgeon should attempt to preserve as much of the remaining posterior cuff as possible during reconstruction. Researchers recently found that following a reverse total shoulder arthroplasty, the posterior deltoid may actually lose its external rotation function. As a result, only the remaining teres minor and infraspinatus can provide any external rotation tasks during abduction postoperatively. In the authors’ hands as well as others, concomitant latissimus transfers can significantly improve postoperative external rotation in patients with complete structural and functional loss of their infraspinatus and teres minor confirmed by magnetic resonance imaging. Although patients can experience encouraging improvement in external rotation, achieving the level of rotation necessary for most ADLs continues to be difficult to achieve with this approach alone.
Significant scapula notching has been associated with decreased clinical outcomes and premature baseplate failure and should be avoided if possible (see Fig. 8 A). To optimize results, the surgeon must focus on placing the glenoid baseplate and glenosphere in a position to maximize the impingement-free arc of motion. Several basic science studies have shown that placing the baseplate inferiorly on the glenoid with 15° to 30° of inferior tilt minimizes inferior scapular impingement. Seeing that the scapula is a 3-dimensional structure, the effect of glenosphere positioning on anterior and posterior scapula impingement that occurs during internal and external rotation has also recently garnered attention. Li and colleagues found that only inferior placement, inferior tilt, and lateralization best allowed impingement-free motion during internal and external rotation. Interestingly, a recent clinical study found that inferiorly tilting the glenosphere might not considerably impact the risk of inferior notching. Fifty-two consecutive patients were randomized to undergo an RSA with or without an inferior tilt to the glenosphere. The severity of notching was graded at a minimum of 1 year postoperatively based on anteroposterior radiographs. The investigators did not find a difference in the incidence of inferior notching between the two cohorts. However, the effect of inferior glenosphere tilt on mechanical impingement and notching in other planes of motion (anterior or posterior) was not evaluated, thus preventing a true comparison. It also remains unclear how longer-term follow-up would impact their findings. Although inferior tilt of the glenosphere may not avoid complete scapula impingement, it does have other added benefits. Slight inferior tilt seems to improve the compressive force at the baseplate/bone interface, assists in tensioning the deltoid, and, most importantly, prevent incidental superior tilt.
Much debate remains on whether a neutral version or a more retroversion is appropriate for the humeral socket. The native humeral version usually centers around 30° of retroversion. Limited clinical data suggest improved outcomes with a more neutral version. Basic science investigations have found that version may not necessarily increase the internal and external impingement-free arc of motion but shifts an established range in the sagittal plane. Increased retroversion seems to allow better external shoulder rotation at the expense of internal rotation. Some investigators have proposed that for some patients this improvement in external rotation activities (eg, using the phone, washing hair, and so forth) is worthwhile, and the effect on most internal rotation activities would be negligible. Humeral sockets positioned with a more neutral version have been shown to allow increased shoulder internal rotation but loss of external rotation, particularly with the shoulder adducted. However, neutral version does not significantly impact shoulder external rotation in the more important abducted position. A more neutral version may allow improvement of internal rotation activities that require positioning the hand in front or behind the body (ie, personal hygiene) without sacrificing external rotation activities that occur with the arm abducted (eg, using a phone, washing hair, and so forth).
Indications
Rotator Cuff Disease With and Without Arthritis
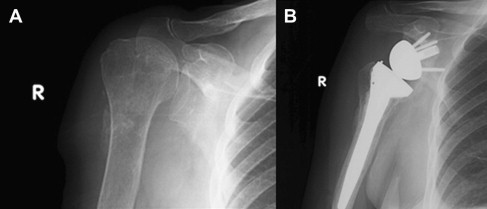
Cuff tear arthropathy (CTA) and massive cuff tears with pseudoparalysis remain the most common and best indications for a reverse shoulder replacement. CTA entails a constellation of findings, including rotator cuff dysfunction, proximal and anterior escape of the humeral head, end-stage arthritis, and pseudoparalysis ( Fig. 9 A ). Older patients may also present with massive irreparable rotator cuff tears and loss of active arm elevation (pseudoparalysis) without end-stage arthritis. The RSA can provide considerable improvement in function and quality of life in these patients (see Fig. 9 B). However, the treating surgeon must remain attentive of critical technical concepts to maximize results.
In the setting of CTA, significant superior glenoid wear can occur, and this bone loss places the surgeon at an increased risk for inadvertent superior tilt positioning of the glenosphere. Superior tilt has been shown to result in decreased arc of motion, increased medial scapular impingement, instability, and higher failure rates. Detailed preoperative planning and assessment of the native glenoid wear pattern should heighten the surgeon’s awareness. Preoperatively, radiographs and a 3-dimensional computed tomography scan will often reveal superior glenoid wear. Current glenoid drill guides may be unable to accommodate for significant glenoid superior wear and other techniques anatomic landmarks should be used to assist in appropriate positioning. Intraoperatively, if patients are positioned in a complete upright position, the alignment drill bit should at least be placed parallel to the floor. A simple technique that the surgeon may use intraoperatively is appreciating the inferior smiley face that results following appropriate eccentric reaming. To avoid medialization of the baseplate by excessive reaming, bone graft from the humeral head can be inserted superiorly between the glenoid and baseplate. The authors have found the aforementioned technique very useful.
Numerous outcome studies following the result of the modern reverse shoulder replacement for patients with CTA report reproducible improvement in pain, active elevation, overhead function, and objective outcome scores. In a large series, Wall and colleagues reported greater than 90% satisfaction rate with an average postoperative active forward flexion of approximately 135°. After a minimum of a 5-year follow-up, Cuff and colleagues found a significant improvement in American Shoulder and Elbow Society (ASES) scores (from 31 to 77). The patients’ ability to elevate their arms also significantly improved from 70° preoperatively to 150° at the final follow-up. Similar success has also been shown for elderly patients with massive irreparable rotator cuff tears without arthritis. Caution should remain on implementing the reverse shoulder prosthesis, if pseudoparalysis is not present, because patients could risk losing the active elevation and rotation they had preoperatively.
Rheumatoid Arthritis
The traditional unconstrained shoulder replacement in patients with rheumatoid arthritis leads to gradual superior migration of the humeral head secondary to a physiologically insufficient rotary cuff. Betts and colleagues reported a 100% occurrence of proximal of the artificial humeral head regardless of the index status of the rotator cuff. This progressive instability tends to correlate with a deterioration of function. This observation has fueled some to offer patients an RSA as a treatment alternative.
Several studies have reported consistent improvement in objective measured outcomes and high patient satisfaction when using the RSA for rheumatoid arthritis. With an average follow-up of nearly 4 years, Young and colleagues reported improvement in active shoulder flexion from an average of 77° preoperatively to approximately 140° postoperatively, with a 94% patient satisfaction rate. Others have also reported similar success. Ekelund and Nyberg found statistical improvement in both range of motion and pain in 23 patients with rheumatoid arthritis who underwent an RSA. Patients, on average, experienced improvement in active shoulder flexion of approximately 80° and a reduction in pain from an 8 to 1 on based the visual analog scale. They reported a low risk for infection (∼4%) despite their immune compromised cause. Holcomb and colleagues also found that postoperative shoulder elevation improved reliably from 52° to 126°, with an 86% success rate when they followed their patients for a minimum of 2 years.
Primary Glenohumeral Arthritis with Static Posterior Subluxation
Recently, investigators have highlighted the concerning results of using the traditional total shoulder replacement in the presence of primary shoulder arthritis with severe posterior glenoid erosion and static posterior glenohumeral subluxation. Higher rates of postoperative posterior instability and premature glenoid failure were found in patients with considerable glenoid intermediate retroversion (>30°) or biconcave (type B2 glenoid) “neo” glenoid retroversion (>27°). These findings have caused some to propose using the reverse total shoulder replacement (TSR) as a more reliable surgical option for this subset of patients.
Failed Shoulder Arthroplasty
The reverse shoulder prosthesis is now considered to be a viable alternative for patients with a failed prior shoulder replacement ( Fig. 10 A, B ). However, the lack of adequate humeral and glenoid bone stock as well as the absence of a functional rotator cuff, frequently encountered in the revision setting, adds a layer of added complexity. Improvements in both pain and function can be anticipated, but several important surgical concepts and techniques are often needed.









