Reverse Shoulder Arthroplasty in the Management of Glenohumeral Arthritis and Irreparable Cuff Insufficiency
Ludwig Seebauer
No financial support was given to perform this research. The author receives royalties from and is consultant to DePuy International, Leeds, UK.
INTRODUCTION
The combination of an arthritic shoulder with irreparable massive cuff deficiency is one of the most difficult and challenging issues in shoulder practice, due to the combination of severe articular surface and periarticular soft tissue damage. The first case was described by Adams and Smith in the 1850s.28 This pathologic entity is the common endstage result of several disease processes such as rotator cuff tear arthropathy (CTA), which is the most common reason,
but also could be caused by entities like autoimmune inflammatory joint diseases (e.g., rheumatoid arthritis) with massive rotator cuff defect or the crystal induced inflammatory arthritis (e.g., Milwaukee shoulder syndrome). Characterized by a substantial unrepairable defect of a minimum of two rotator cuff tendons, these disease processes lead to an unstable glenohumeral joint with superior migration of the humeral head and secondary severe damage to both the intraarticular and extra-articular elements. The result is a painful, dysfunctional shoulder that necessitates, in many cases, a surgical solution. The lack of adequate stability and the insufficient bone stock make the task of replacing the damaged joint with a stable construct difficult. Neer62,63 was the first who introduced in the modern literature the term “cuff tear arthropathy” and called it as one of the most challenging issues in shoulder arthroplasty, due to the infrequent restoration of overhead shoulder function with conventional shoulder arthroplasty.20,46 As a result, Neer introduced the term “limited goal rehabilitation” to characterize the typical surgical outcome. The primary goal of conventional hemiarthroplasty was an improvement in pain. A significant gain in function after hemiarthroplasty was mostly dependent upon having a biomechanically compensated or balanced anterior (intact subscapularis) and some infraspinatus and teres minor function along with an intact coracoacromial arc, resulting in a superior migrated humeral head with a stable fulcrum of rotation of the humeral head.
but also could be caused by entities like autoimmune inflammatory joint diseases (e.g., rheumatoid arthritis) with massive rotator cuff defect or the crystal induced inflammatory arthritis (e.g., Milwaukee shoulder syndrome). Characterized by a substantial unrepairable defect of a minimum of two rotator cuff tendons, these disease processes lead to an unstable glenohumeral joint with superior migration of the humeral head and secondary severe damage to both the intraarticular and extra-articular elements. The result is a painful, dysfunctional shoulder that necessitates, in many cases, a surgical solution. The lack of adequate stability and the insufficient bone stock make the task of replacing the damaged joint with a stable construct difficult. Neer62,63 was the first who introduced in the modern literature the term “cuff tear arthropathy” and called it as one of the most challenging issues in shoulder arthroplasty, due to the infrequent restoration of overhead shoulder function with conventional shoulder arthroplasty.20,46 As a result, Neer introduced the term “limited goal rehabilitation” to characterize the typical surgical outcome. The primary goal of conventional hemiarthroplasty was an improvement in pain. A significant gain in function after hemiarthroplasty was mostly dependent upon having a biomechanically compensated or balanced anterior (intact subscapularis) and some infraspinatus and teres minor function along with an intact coracoacromial arc, resulting in a superior migrated humeral head with a stable fulcrum of rotation of the humeral head.
Most patients with rotator cuff deficient arthropathy are significantly older than 70 years, with poor quality tissues and multiple medical co-morbidities, making improvements in functional outcome through postoperative rehabilitation more challenging and limited. Patients with an elevated humeral head but with an unstable fulcrum for rotation have superior escape of the humeral head from the coracoacromial arch, resulting in what was termed “a pseudoparalytic shoulder.” These patients are characterized by unrepairable massive (two tendons and more) rotator cuff defects, with or without joint surface arthritis or deformity. In all patients with a diagnosis of rotator cuff deficient arthropathy, the cuff defect by definition is not reparable. An alternative option for a nonarthritic shoulder with a nonreparable rotator cuff defect without superior escape is reconstruction of the rotator cuff defect, which consists of complex muscle tendon transfer procedures (e.g., latissimus dorsi tendon transfer, teres major transfer, or pectoralis major tendon transfer). Muscle transfer reconstruction requires extensive surgery and prolonged rehabilitation with an uncertain functional outcome in the elderly patient. Moreover, progression of the pathology to an arthritic joint is not prevented by a tendon transfer.44,94
Paul Grammont introduced a reverse total shoulder prosthetic reconstruction with a medial center of rotation in the early 1980s (DeltaTM prosthesis, DePuy International, Leeds, UK) in Europe,5,38 and in the late 1980s Mark Frankle (EncoreTM prosthesis, Encore Medical Corporation, Austin, TX) introduced reverse shoulder arthroplasty in the United States with a lateral center of rotation.30 Over the last two decades, improvements in surgical techniques and prosthetic design of the reverse total shoulder concept dramatically improved the treatment results of the complex pathology of rotator CTA.
CLASSIFICATION OF CUFF TEAR ARTHROPATHY
Rotator CTA or rotator cuff deficient arthritic (RCDA) shoulder is not a unique pathologic entity, but consists of different underlying pathologies. It is a common end stage of several disease processes with a unique clinical feature: painful arthritic shoulder with a massive, irreparable rotator cuff defect. Often, this is combined—secondary or primary—with significant bone erosion on the glenoid and also sometimes at the proximal humerus. Neer62 termed this rotator CTA as an end result of a chronic massive cuff tear. But, CTA in the narrower sense represents only the most important pathoetiology of several pathologies that leads to the clinical and radiologic entity of CTA in a wider sense, better termed as rotator cuff deficient arthritic (RCDA) joint.
DIFFERENT PATHOETIOLOGIES OF CUFF TEAR ARTHROPATHY
It is important to recognize the various disease processes that lead to glenohumeral RCDA joint.
Rotator CTA in the narrower sense is an extreme end result of a massive rotator cuff tear. The term coined by Neer in 198362 refers to a primary massive rotator cuff tear that by virtue of mechanical superior instability and nutritional effects leads to a secondary glenohumeral joint destruction. It is believed that between 0% and 25% of massive rotator cuff tears will end up as CTA but it is difficult, if not impossible, to predict which of the massive tears will result in CTA. This entity represents the highest percentage of RCDAs treated nowadays by reverse shoulder arthroplasty.
Rotator CTA is the end stage of a long-standing cuff defect, which is characterized by massive rotator cuff tear with superior migration and progressive reduction of acromion- humeral distance with secondary erosive changes and deformation of the tuberosities (“femoralization”), erosion of the acromion, deformity of the humeral articular surface, and central and/or superior glenoid bone erosion. He also described two different pathogenetic models for end-stage rotator CTA: one mechanically based due to loss of the normal centering of the humeral head, the other biologic and biochemically oriented due to loss of the normal synovial fluid nutrition due to an inflammatory condition resulting in damage to the articular cartilage.
Rheumatoid arthritis (RA) is the next common cause of RCDA. Between 48% and 65% of RA patients have significant glenohumeral joint involvement. About 24% of those having glenohumeral arthritis will have a simultaneous rotator cuff tear.50 Superimposed on the aforementioned changes are severe osteopenia, erosions of the entire glenoid without osteophyte formation, and medialization of the glenohumeral joint.
The Milwaukee shoulder syndrome was originally described by McCarty in 1981.59 This is an uncommon entity affecting shoulders of elder people, predominantly women. It consists of a massive rotator cuff tear, joint instability, bony destruction, and large blood-stained joint effusion containing basic calcium phosphate crystals, detectable protease activity, and minimal inflammatory elements. Its relation to rotator cuff arthropathy is not clear, and it might represent one spectrum
of the above. The role of the basic calcium phosphate crystals in creating this syndrome is still controversial. It could be discussed whether the type III cases according to our classification system represent a relevant portion of this pathology.
of the above. The role of the basic calcium phosphate crystals in creating this syndrome is still controversial. It could be discussed whether the type III cases according to our classification system represent a relevant portion of this pathology.
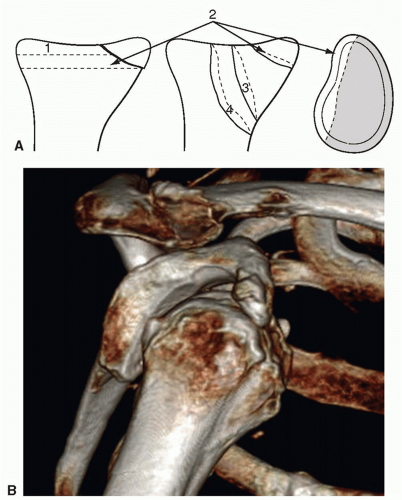
BIOMECHANICS OF MASSIVE ROTATOR CUFF TEARS
Balanced versus Unbalanced Shoulder- Pseudoparalysis
The rotator cuff tendons provide a major contribution to the dynamic stabilization of the glenohumeral joint by centering the humeral head within the concavity of the glenoid, resulting in a compression force in the joint.49,90 A massive tear, consisting of the supraspinatus and at least one of the other adjacent rotator cuff tendons (in most cases the infraspinatus), may render the rotator cuff’s anterior and posterior force couple ineffective in both the vertical and the transverse planes. The balance between the superior force generated by the deltoid muscle and the central-inferior direction of the rotator cuff force couple is lost. The centering of the humeral head will be biomechanically unbalanced and the functional for rotation of the humeral head within the glenoid is also lost. The result is a diminution of joint reaction force and a change in the overall direction of the joint force that leads to an unstable glenohumeral joint with superior displacement of the humeral head.66 It remains debated whether the presence of the long head of the biceps tendon provides any meaningful resistance to superior translation of the humeral head, but a severe damaged tendon is unlikely to add stability by active tensioning of the muscle-tendon unit.48 The fulcrum and moment arm of the deltoids decrease with superior migration of the humeral head.16,82 Posterior- superior massive tears have a more direct superior humeral head migration, whereas the anterior-superior rotator cuff defects will have more of an anterior-superior migration due to loss of subscapularis function. The anterior-superior cuff defects are more likely to present with escape of the humeral head from the coracoacromial arch and a pseudoparalytic shoulder function. Gagey33 described a biomechanically important tight fibrous frame consisting of collagen fiber bundles in the anterior part of the supraspinatus and in the superior part of the subscapularis, the biceps tendon, and the coracohumeral ligament, which acts as a passive restraint against anterior-superior translation. Therefore, rotator cuff defects of the same size located in the anterior-superior section of the cuff leads to a greater amount of superior translation than posterior-superior defects. The superior migration of the head leads to deformation of the humeral head (“femoralization”), rounding and thinning of the coracoacromial arch (“acetabularization”), and subsequently to the destruction of the anterior-superior glenoid26 (Fig. 19-1). The acromioclavicular joint is also frequently involved in the process, joining its cavity with that of the now combined synovial intra-articular and subacromial bursae spaces. Cases of secondary stress fractures of the thinned acromion or scapular spine have also been published.15,61 Progression of the erosive changes of the coracoacromial arch can result in detachment of the deltoid origin.86 When this occurs there is an even greater loss of shoulder function and the reconstructive options even with reverse shoulder arthroplasty are compromised. The continued anterosuperior displacement and instability of the humeral head will change the center of rotation cause resulting in insufficiency of the function of the deltoid muscle.16 Biomechanical investigations done by Grammont10,39 and De Wilde16,18 have shown that a caudal and medial displacement of the glenohumeral center of rotation causes a significant increase in the moment arm of rotation of the deltoid muscle. Conversely, it could be assumed that the superior and lateral displacement of the center of rotation deteriorates the biomechanics of the deltoid. Finally, with an unopposed superior pull of the deltoid without a stable center of rotation or fulcrum, elevation or abduction of the arm is compromised. The active flexion and abduction of the shoulder despite the greatest deltoid contraction attempts is significantly less than 90 degrees often with superior escape of the humeral head from the confines of the coracoacromial arch, defined as a pseudoparalytic shoulder (Fig. 19-1).
CLASSIFICATION SYSTEMS OF CUFF TEAR ARTHROPATHY
Hamada-Fukuda Classification41
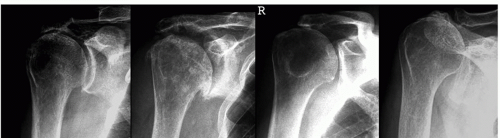
The Hamada-Fukuda classification is a morphologic and radiological description of the progression of massive rotator cuff tears, and the more advanced stage in this classification addresses primary rotator CTA.62 Using arthrographic definition of a massive cuff tear, they defined five types: Type 1 is characterized by a normal joint morphology and an acromiohumeral distance of more than 6 mm. In
type 2, the acromion-humeral distance was 5 mm or less. In type 3, additional acetabularization could be observed. Acetabularization is defined as a concave deformity of the acromion undersurface and distinguished into two subtypes. In type 4, narrowing of the glenohumeral joint is added, and in type 5, collapses of the humeral head are seen. Despite this very comprehensive description of the common progression of the morphologic features of massive rotator cuff tear that can progress to rotator CTA, the classification does not provide a means of correlation of the pathologic changes with a recommended treatment of prediction of outcome of treatment.
type 2, the acromion-humeral distance was 5 mm or less. In type 3, additional acetabularization could be observed. Acetabularization is defined as a concave deformity of the acromion undersurface and distinguished into two subtypes. In type 4, narrowing of the glenohumeral joint is added, and in type 5, collapses of the humeral head are seen. Despite this very comprehensive description of the common progression of the morphologic features of massive rotator cuff tear that can progress to rotator CTA, the classification does not provide a means of correlation of the pathologic changes with a recommended treatment of prediction of outcome of treatment.
Favard Classification26
Favard described three different types of CTA focusing on the pathologic changes of the glenoid. Type I is characterized by superior glenohumeral wear with upward migration and pathologic changes of the acromion, type II shows central narrowing with little alteration of the acromion shape, and finally type III represents the lysis of the head or acromion.
This classification defines the anatomic pathology without their effect on the type of treatment recommended or a prediction of the outcome of treatment. Type I is developing slowly out of old tears (cuff tear arthropathy acc. Neer)—some coming to destructive type of arthropathy. Type II is estimated as an osteoarthritic shoulder with secondary massive cuff tear. Type III is seen for “rheumatoid shoulders” with a concomitant cuff tear and bony destruction.
Levigne Classification55
Levigne and coworkers55 developed a classification for the radiologic appearance of rheumatoid arthritis shoulders with massive rotator cuff tears. They distinguished between six different types: Concentric type without glenoid erosion (C1) and with glenoid erosion (C2), ascendant type without erosion (A1) and with erosion (A2), and destructive type without erosion (D1) and with erosion (D2).
Burkhart Classification86
Burkhart classification is not a classification for CTA, but it was developed as a classification of cuff tears based on their biomechanical behavior. Under dynamic radiologic examination (fluoroscopy), Burkhart found three different biomechanically different types of rotator cuff tears. His investigations focus on the position of the fulcrum of the glenohumeral joint. The fulcrum of the glenohumeral joint could be stable, unstable, or captured.
The Seebauer classification was established to define the functional and biomechanical consequences of CTA based on the severity of the disease and has four types. The classification focuses on the position and stability of the center of rotation of the humeral head on a static (normal X-ray) and dynamic (fluoroscopy) radiologic imaging. The major intention was to develop a classification that offers therapeutic guidelines and is independent from the underlying cause of the rotator cuff deficiency or arthritic changes of the joint.
The occurrence, expression, and presentation of the morphologic features are multifactorial and are dependent on the severity of the underlying pathology and the pathomechanics of the joint. The pathomechanics of the rotator cuff tear is dependent on the size and location of the tear and the number of tendons involved. The types of pathology within the classification are also dependent upon the integrity of the coracoacromial arch and the bony geometry of the glenoid.
The classification defines the progression of the soft tissue and bone defects, which causes superior migration and instability of the humeral head, and therefore, defines the biomechanical, functional, and morphologic classifications, which focus on the position and stability of the center of rotation of the humeral head. As a result, the Seebauer classification can be used as a tool for surgical decision based on the head stability within the CA arch.
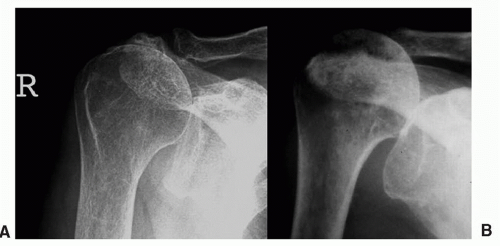
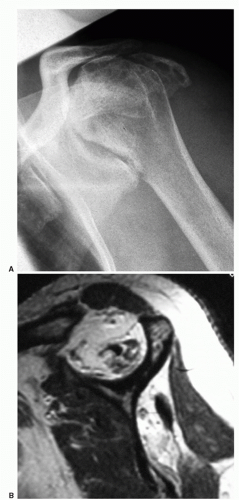
In types Ia and Ib, the center of rotation is not displaced, whereas in types IIa and IIb it is significantly displaced superiorly. Type IIb is characterized by a complete static or dynamic anterosuperior instability (Fig. 19-2) (Table 19-1). Sometimes, the distinction between type IIa and IIb is difficult on a simple static anteroposterior (AP) X-ray. To distinguish between both types, the physical examination of the shoulder with attempted active forward elevation against resistance shows an dynamic increase in the superior displacement of the humeral head from the position of the humeral head at rest in type IIb patients. This could also be proved by a radiologic investigation under fluoroscopy or with stress radiographs of the shoulder. The four types are markedly different with respect to preoperative function (after elimination of pain by local anesthetic injection test) and to the results after conventional shoulder hemiarthroplasty77 (Fig. 19-3A,B).
TABLE 19-1 Author’s Pathomechanical and Pathomorphologic Classification of Cuff Tear Arthropathy (CTA) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
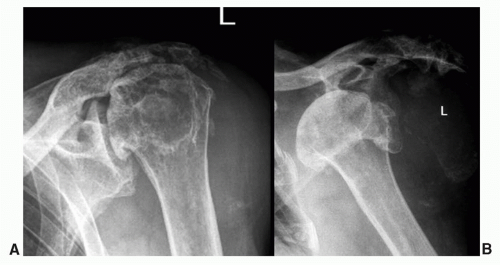
Additional Type of Cuff Tear Arthropathy: Type III A&B According to the MODIFIED SEEBAUER CLASSIFICATION
Within the last year, an increasing number of elderly, mostly female were observed with a very progressed and difficult to treat type of CTA (Fig. 19-4). The author calls this group the “geriatric shoulder.” The patient is older than 75 years and is characterized by superior glenoid erosion, attrition of the coracoacromial arch with erosion of the acromion (Type IIIa) and in some cases significant anterior glenoid erosion and chronic (fixed) anterior dislocation of the humeral head (Type IIIb).
Loew’s Classification56
A more recent classification of Loew et al.56 differentiated three types of rotator CTA based on the severity of the joint damage, joint stability, clinical symptoms, and radiologic changes.
Glenoid Defect Classification Systems
The presence and significance of glenoid defects in patients with a chronic rotator CTA are defined in several publications.2,31,74,75 Significant glenoid involvement is seen in up to 30% of patients.
Favard distinguished between four types of glenoid defects26 and in a later paper81 five different types of glenoid erosion: E0: no erosion, E1: central erosion, E2: isolated superior erosion, E3: global central and superior erosion, and E4: isolated inferior erosion.
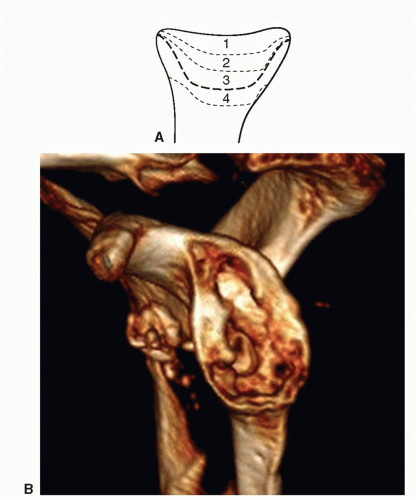
Owing to the fact that there are not only superior or inferior defects, but also anterior, superior, or a combination of the defect’s location in patients with CTA, we developed a classification,74 which distinguishes between centric and eccentric defects, where in eccentric defects not only the extension, but also the position of the defect is classified.
Seebauer Classification of Glenoid Defects
Centric (contained) defects (Fig. 19-5A,B)
C1 shallow
C2 deep, stable vault
C3 deep, unstable vault
C4 deep, vault destroyed.
Eccentric defects (Fig. 19-6A,B)
Anterior, posterior, inferior, superior
E1 small (shallow)
E2 medium (−30%)
E3 large (30% to 60%)
E4 massive (>60%).
For example, E1a means small anterior eccentric glenoid defect.
Frankle’s Glenoid Defect Classification31
A more recent classification by Frankle et al.31 distinguishes between four different types of glenoid erosion, which could be observed in patients with rotator CTA undergoing reverse shoulder arthroplasty. In a series of 216 patients with CTA (n=130), failed cuff surgery (n=82), and proximal humeral malunions
(n=4), he found 37.5% of pathologic glenoid morphology, mostly with posterior (17.6%) and superior (9.3%) eccentric erosion. All the patients had evidence of rotator cuff deficiency with glenohumeral subluxation, arthritis, or pseudoparalysis.
(n=4), he found 37.5% of pathologic glenoid morphology, mostly with posterior (17.6%) and superior (9.3%) eccentric erosion. All the patients had evidence of rotator cuff deficiency with glenohumeral subluxation, arthritis, or pseudoparalysis.
CLINICAL AND RADIOLOGICAL EVALUATION
Patients with rotator cuff deficiency have various degrees of pain, recurrent swelling, and functional loss. The etiology may be trauma or various diseases affecting the articular surfaces and soft tissues around the joint such as rheumatoid arthritis. To determine the optimal treatment, a careful clinical evaluation is necessary. Furthermore, it is important to take the patient’s age and functional demands into account.
Dines et al.21 developed an algorithm for the treatment of irreparable rotator cuff tears. This algorithm did not take a specific accounting of the elderly patient with a pseudoparalytic shoulder without radiologic signs of arthritis. The treatment algorithm must take into account if the residual rotator cuff is able to provide a biomechanically stable articulation. Often what appears to be a biomechanically unstable shoulder is a result of the functional limitations associated with shoulder pain. Therefore, it is important to evaluate active and passive range of motion of the shoulder both before and after the use of a local anesthetics into the joint. On the other side in cases where patients are able to actively elevate the arm above shoulder level or in cases with dynamic or static superior humeral head escape and pseudoparalysis injection of the joint is not likely to provide much additional information. In many patients it can be seen that between these two extremes, local injection of the joint to minimize the contribution of pain to the limits of function can be helpful in evaluating the true active range of motion. Patients with maintained fixed fulcrum kinematics (balanced shoulder) have good active range of motion, while patients with biomechanical deficiency (unbalanced shoulder) after a testing injection of local anaesthesia have poor active range of motion (pseudoparalysis) (Fig. 19-7).
The reverse ball-and-socket arthroplasty rely on the deltoid muscle for function. The prosthetic design provides a fixed fulcrum that enforces rotation of the humerus and thereby provides biomechanical function of the rotator cuff in the absence of the rotator cuff. Therefore, the function of the axillary nerve and deltoid muscle must be checked. The easiest way to evaluate the function is by asking the patient to elevate the arm while the examiner place fingers over the anterior third of the deltoid muscle. If contraction is felt, the function of the muscle is satisfactory. If it is difficult to clinically determine the function of the deltoid muscle, an EMG can be indicated. Furthermore, it is important to evaluate the strength of internal rotation and external rotation. The reverse total shoulder replacement does not provide rotational function to the shoulder and overhead abduction-external rotation especially benefits from the external rotation function of the remaining portions of the rotator cuff. The presence of lag signs (e.g., hornblower sign) in abducted or adducted position should be evaluated on physical examination. Significant external rotational lag signs in both arm positions indicate total absence of infraspinatus and teres minor. In these cases, we recommend either CT-arthrogram or an MRI in both axial and sagittal planes to define the presence of the lower part of the infraspinatus and teres minor portion
of the rotator cuff along with the severity of the muscle atrophy of these muscles. In cases with the loss of all external rotation function, a reverse total shoulder replacement in combination with a muscle-tendon transfer to improve external rotation function should be considered.
of the rotator cuff along with the severity of the muscle atrophy of these muscles. In cases with the loss of all external rotation function, a reverse total shoulder replacement in combination with a muscle-tendon transfer to improve external rotation function should be considered.
Radiological Evaluation
Plain radiographs in true AP, axillary, and scapula lateral (Y)-views should always be taken to analyze the degree of joint degeneration, osseous defects, glenoid erosion, amount and dynamic and static instability of the joint. In some cases with clinically demonstrated pseudoparalytic shoulder, the standard radiographs do not show significant superior migration of the head. This generally occurs with more acute than in chronic massive cuff tears. In the dynamic stress radiographs with fluoroscopy under resisted abduction of the arm, the superior instability and migration can be confirmed if radiographic documentation of the physical exam findings is desired.
CT-scans in all planes and three-dimensional (3D)- reconstruction can be useful in cases with glenoid bone loss, or with marked thinning of the acromion associated with fatigue fractures of the scapular spine. For estimation of glenoid defects, the 2D CT-scans, even if analyzed in all three planes (axial, coronal, and sagittal) are significantly less predictive about the extent of the glenoid defect31,73 than a 3D-reconstruction.
An MRI examination should be carried out always in younger patients (<70 years), to determine the exact size, repairability of the cuff defect, and whether a treatment alternative to reverse shoulder arthroplasty exists. Alternatives to reverse replacement include cuff repair, muscle tendons transfer for cuff reconstruction, cuff repair and hemiarthroplasty, muscle tendon transfer and hemiarthroplasty, or arthroscopic debridement with biceps tenotomy. This should be considered with a more acute tear with less than or equal to grade 2 muscle atrophy, compensated shoulder function without pseudoparalysis, or superior escape. MRI scan is useful to evaluate the cuff in these cases (Fig. 19-7A).
TREATMENT OPTIONS OF CUFF TEAR ARTHROPATHY
Nonsurgical
Strengthening of the deltoid muscle and remaining rotator cuff muscle can result in improved function. Injection of corticosteroids into the joint can be tried to relive pain in combination with oral analgesics. This can be sufficient in patients with mild or moderate pain and moderate loss of function.
Arthroscopic Surgery
Arthroscopic debridement and biceps tenotomy has been reported86 to improve pain and partial improvement in function in patients with CTA, if the long head of the biceps is still present under the acromion, the cuff defect is more posteriorsuperiorly, and there is still some balance between the rotator cuff force couples with good deltoid function. The outcome of limited-goal arthroscopic debridement is much less predictable, in patients with CTA without an intact biceps tendon and with more anterior-superior defects, as these patients more commonly progress to anterior-superior static subluxation and unbalanced shoulder kinematics. The arthroscopic procedure can be tried particularly in elderly patients with low demands and in patients not willing to undergo major surgery. It may relieve pain but not restore function in pseudoparalytic shoulders.
Arthrodesis—Resection Arthroplasty
In patients with severe deltoid muscle damage or axillary nerve palsy, arthrodesis or resection arthroplasty can be the only option to achieve pain relief. The predictability of pain relief by performing an arthrodesis in patients with CTA is not as good as desired. Nevertheless, in patients with pseudoparalysis, an arthrodesis can improve functional range of motion. However, increased load on the thoraco-scapular articulation and the acromioclavicular joint may create pain at these locations. In 1991, Arntz et al.3 reported 10 patients who underwent arthrodesis for irreparable cuff tears. The arthrodesis improved active forward elevation on an average of 15 degrees. They concluded that arthrodesis could be indicated in patients with massive irreparable cuff tears and significant deltoid deficiency or in young patients with demands of significant strength at low angles of flexion.
Resection arthroplasty is a poor solution, which yields an unstable, nonfunctional, often painful shoulder, and thus should not be carried out as a primary surgical treatment in these patients.
Anatomical Unconstrained Arthroplasty
Total Shoulder Arthroplasty
The superior migration of the humeral head in patients with CTA creates eccentric load on the glenoid component. This has been called the “the rocking-horse” effect of glenoid contact, resulting in increased rate of loosening.32 In 1991, Lohr and Cofield57 reported better pain relief in total shoulder arthroplasty compared to hemiarthroplasty in 22 patients with cuff deficiency but an increased incidence of radiographic and clinical loosening of the glenoid component. Similar findings were reported by Franklin et al. in a study where three of nine patients with cuff deficiency needed early revision after total shoulder arthroplasty.32 Owing to this increased risk of glenoid loosening, anatomical total shoulder replacement is not recommended in patients with significant cuff deficiency. This does not imply that all patients with any sized rotator cuff tear will have early glenoid loosening or a less favorable outcome with an anatomic total shoulder replacement. A single tendon, reparable tear of the supraspinatus tendon with a wellbalanced shoulder and a centered humeral head will not result in an unbalanced shoulder and the early and mid-term results of an anatomic total shoulder arthroplasty are equal to that in an osteoarthritic shoulder with an intact rotator cuff.
Hemiarthroplasty
For many years hemiarthroplasty has been the treatment of choice for the arthritic shoulder with cuff deficiency. Due to the clinical success of the Paul Grammont’s concept and the introduction of the reverse ball-and-socket arthroplasty, the indication for using a hemiarthroplasty has become much more limited. When considering all patients with cuff deficient arthropathy the results after hemiarthroplasty are less predictable than the results obtained from reverse shoulder replacement. Neer proposed the term “limited goal” rehabilitation for patients with rotator cuff tear arthroplasty undergoing hemiarthroplasty replacement.63 Persistent pain has been reported in 6% to 53% of the patients after hemiarthroplasty and an improved active elevation from 60 to 70 degrees preop to 90 to 120 degrees postop.23,29,63,67,71,92,95 An oversized humeral head has been suggested in order to create a better articulation with the acromion and the coracoacromial arch. However, Sanchez et al. could not find a correlation between head size and function. Furthermore, the use of an oversized humeral head may increase the joint reaction forces and may be responsible for a more rapid glenoid bone resorption.71 Also, a large head makes it more difficult to partially repair the rotator cuff.
Several techniques have been proposed and used for hemiarthroplasty. Pollock et al.67 and DiGiovanni et al.63 advocated the use of a subscapularis tendon transfer to a more superior position as a method for superior stabilization of the humeral head. The subscapularis tendon can then be re-inserted into the top of the greater tuberosity. The use of anatomic, or slightly smaller, humeral head sizes seems to facilitate this transfer. This option is limited to those patients who have a functional, un-shortened subscapularis tendon.
CTATM-Head Hemiarthroplasty
In an attempt to improve the results of hemiarthroplasty in patients with CTA, a specific head has been designed, i.e., CTA head (CTATM-head DePuy Johnson and Johnson, Warsaw, Indiana). It has a lateral extension over the greater tuberosity creating a greater arc for articulation against the glenoid fossa and the undersurface of the acromion and coracoacromial arch (see Fig. 19-8). The head size is anatomical, so there is no “overstuffing of the joint.” This size adapted head, which did not deteriorate the lever arm significantly, is articulating under the acetabularized coracoacromial arch as a fulcrum. The prosthesis design with its greater lateral coverage of the head prevents the painful impingement of the eroded and uncovered greater tuberosity against the acromion in abduction/flexion and external rotation. Early clinical results showed encouraging outcomes in patients, where the joint is biomechanically still balanced and stable and the center of rotation is not extremely anterior-superior migrated.4 In our institute we have a follow-up of 21 patients with a follow-up time of more than 24 months.72 These 21 patients had Seebauer type Ia, Ib, or IIa CTA. All patients had compensated shoulder function with a stable
humeral head under the coracoacromial arch without superior escape. The patients with type Ia and Ib CTA demonstrated over the complete follow-up period a constant clinical result with minimal superior migration of the center of rotation by the time. In patients with type IIa, we sometimes could observe slow decrease of the Constant score values and increasing superior migration with the development of a type IIb-instability. In two of the 21 patients, a revision to reverse shoulder arthroplasty was performed due to a secondary subscapularis tendon failure.
humeral head under the coracoacromial arch without superior escape. The patients with type Ia and Ib CTA demonstrated over the complete follow-up period a constant clinical result with minimal superior migration of the center of rotation by the time. In patients with type IIa, we sometimes could observe slow decrease of the Constant score values and increasing superior migration with the development of a type IIb-instability. In two of the 21 patients, a revision to reverse shoulder arthroplasty was performed due to a secondary subscapularis tendon failure.
Bipolar Arthroplasty
A bipolar arthroplasty has a humeral component with a stem with a small diameter head, upon which is a mobile outer shell that is sized to be approximately the size of the humeral head. The mobile head is snap fit to the smaller fixed head.93 The idea was to have a hemiarthroplasty acting like a “total shoulder replacement” by having motion between the fixed head and the outer shell. In the 1980s and 1990s, a few series reported reasonable to good results with this type of hemiarthroplasty. Today, the bipolar arthroplasty is not widely used, as the outcome is unpredictable and there has been concern of “overstuffing” of the joint.
Reverse Arthroplasty
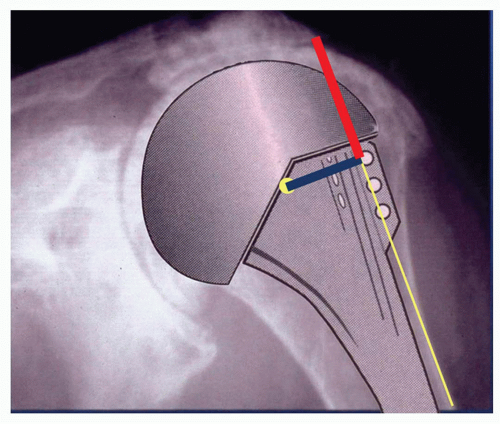
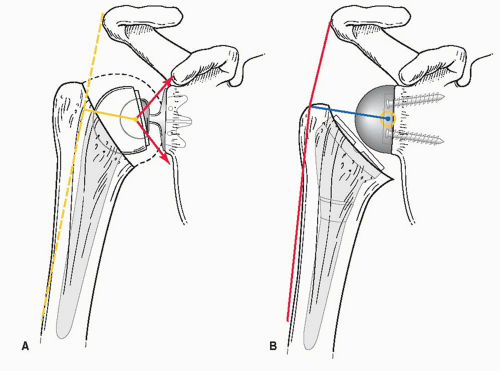
The concept of reverse total shoulder relies on the deltoid muscle for function and stability. The conversion of convexity and concavity provides stable fulcrum kinematics of the glenohumeral joint, despite the presence of a massive cuff defect. Most of the early designs failed on the glenoid side due to a small radius of curvature of the glenosphere with lateralized center of rotation (Fig. 19-9A). The present reverse design with a medial center of rotation primarily used in Europe in mid-1980s to the current time is based on the concepts of Paul Grammont from Dijon, France.10,38,39 The first publication of larger clinical series of his DeltaTM prosthesis was reporting about implantations from 1987 on in France.5,38 Grammont’s design has the convex head on the glenoid side with the center of rotation on the glenoid resection surface and the concave component on the humeral side. The simultaneous medialization and lowering of the center of rotation brings the deltoid muscle into a better biomechanical pattern (Fig. 19-9B). In 1993, Grammont and Baulot38 reported on the first 14 cases with the DeltaTM reverse ball-and-socket arthroplasty with good pain relief and improved function. A number of consecutive series of different authors confirmed that this prosthesis can give excellent pain relief and restoration of active range of motion in patients with painful pseudoparalytic shoulders.5,10-13,30,40,45,85,89,91,78,81 Due to the small number of long-term follow-up studies, it is primarily recommended in older patients with CTA. Many patients that would have received a hemiarthroplasty in the past are now treated with the reverse arthroplasty. However, patients with good active range of motion despite arthritis and a massive rotator cuff tear (biomechanical balanced shoulder) may still have a good outcome with a hemiarthroplasty.4,72
In the United States, the first commercially available reverse shoulder arthroplasty (Encore Medical, Austin, TX) was developed by Mark Frankle and clinically used since the late 1990s.30 In Frankle’s design the center of rotation is not as far medialized as in Grammont’s design. This has decreased the risk of bone erosion at the inferior glenoid (inferior glenoid notching), a frequently observed phenomena in Grammont’s type of reverse shoulder arthroplasty and also has some other benefits on the deltoid and residual cuff biomechanics by keeping the center of rotation more laterally. On the contrary, the positioning of the center of rotation laterally to the glenoid resection surface increased the risk of early glenoid component loosening, particularly with the early designs for glenoid fixation. The frequency of this problem observed in the first series could be decreased by modification of the fixation design without changing the original design idea.
Recently, a combination of Grammont-type prosthesis design with an interposition of an autologous bone graft between the native glenoid and the metaglene base plate was introduced to increase the scapular neck length termed by Pascal Boileau the BIO-RSA.9 This concept was put forth to have the benefits of Grammont concept of having the implant center of rotation at the bone interface and the Frankle design concept of lateralization of the glenosphere. The theoretical benefits of this design will be discussed later in this chapter.
History and Biomechanics of the Reverse Shoulder Arthroplasty
Several constrained total shoulders have been tried. Some of these have been reverse designs. The goals were to restore deltoid length and to create a fixed center of rotation. Initial results showed significant improvement in function, but due to high failure rate on the glenoid side and the design-related limited range of motion, these designs were abandoned.1,51,68 A common design feature of these early constrained arthroplasties was the lateralized center of rotation outside the glenoid bone (Figs. 19-9A and 19-12). This created a high stress on the fixation of the glenoid component, resulting in early aseptic loosening. Therefore, these types of reverse shoulder arthroplasty did not achieve a wide and long-term clinical application and were abandoned quite soon.
Paul Grammont, from Dijon, France, continued to work on the concept of reverse design arthroplasty with the idea that it could restore a stable fulcrum and replace the function of the rotator cuff. After the failure of his “Ovoid” arthroplasty concept (egg-shaped humeral head replacement) in the mid-1980s, he moved to a reverse design with a large hemisphere on the glenoid side to place the center of rotation at the glenoid bone-implant interface. His first reverse design was the “Trumpet prosthesis” (Fig. 19-12A), which was designed in 1985. The humeral component was an all-polyethylene component and the glenoid component was a ball made of metal or ceramic and two-thirds of a sphere with 42 mm diameter. Both components were cemented. The results in eight cases were variable; therefore, Grammont decided to have a cementless fixation of the glenoid component and to have half a sphere instead of two-third of a sphere on the glenoid side. The design of Grammont’s definitive reverse shoulder arthroplasty characterized by the conversion of convexity and concavity to achieve a stable fulcrum shoulder joint kinematics despite massive cuff defect and by the medialization and lowering of the center of rotation brings the deltoid muscle into a better biomechanical pattern (Figs. 19-9B and 19-12B). Grammont’s design in contrast to reverse arthroplasty designs developed in the 1970s was not a fully constrained prosthesis, with a high risk of early glenoid component loosening. The intrinsic stability by his prosthesis geometry was achieved by the “Coadaptation” principle,38 by transforming the superior directed deltoid pull into joint stability and active abduction and flexion by inversion of concavity and convexity at the glenohumeral joint (Fig. 19-10). This definitively allows active flexion and abduction significantly higher than 120 degrees, and therefore improves shoulder function dramatically. The glenoid component consisted of a metaglene plate that had a central peg and was fixed with four additional screws. A large hemisphere (36 or 42 mm) was then attached to this metal plate. The center of rotation of the joint was at the glenoid bone-implant interface for the entire course of range of motion. This design principle creates a centripetal force transmission of the shear forces through the entire arc of motion to the glenoid bone-implant interface, helps to
avoid early glenoid loosening, and enhances bony fixation of the cementless implanted glenoid base plate (metaglene) (Fig. 19-11). The humeral component was uncemented with a corresponding polyethylene cup with various depths. It was further redesigned into the Delta3TM arthroplasty (DePuy International Ltd, Leeds, UK) available in 1991 (Fig. 19-12). Later, a very similar design was introduced in the market by several other companies (AequalisTM reverse shoulder arthroplasty, Tornier Inc., France; SRATM reverse shoulder arthroplasty, Lima Inc., Italy; Zimmer® Anatomical Shoulder Invers-ReversTM, Zimmer Inc., Warsaw, Indiana; Zimmer® Trabecular MetalTM Reverse Shoulder System, Zimmer Inc., Warsaw, Indiana). The common principle of all this prosthesis followed the idea of Grammont with a hemispherical glenoid component, with a center of rotation at the glenoid bone-implant interface, with the metaglene fixed directly on the glenoid resection surface, and a humeral component with a concave epiphyseal design with a 155-degree orientation of the humeral PE-liner. This reverse ball-and-socket design by Grammont has two major advantages. It has a large glenoid hemisphere with no neck and a small humeral cup with a nonanatomical inclination angle of 155 degrees, which covers less than half of the glenosphere. This design with a large hemisphere with no neck on the glenoid side medializes the center of rotation and places the center of rotation at the surface of the glenoid bone (Figs. 19-9B and 19-11). All the forces acting on the prosthesis pass through the fixed center of rotation; thus, the neckless design with a hemispheric glenoid component transforms the torque created by former designs into compressive forces at the prosthesis-bone interface (Fig. 19-11). This solved the formerly inevitable problem of loosening of the convex glenoid component. This reduces the torque forces on the component and creates less risk of loosening. Furthermore, it provides a fixed center of rotation, preventing the superior migration of the humeral head and increases the length of the deltoid muscle (Fig. 19-9B). The large diameter also allows greater range of motion before impingement can occur. The nonanatomical inclination (155 degree) of the humeral component places the humeral component in an inferior position, making it easier to increase the length of the deltoid muscle, and places the deltoid muscle under tension. Because of the medialization of the glenosphere, an external rotation cannot be restored and impingement inferiorly between the humeral component and scapula, resulting in a “notch,” is a concern when the glenosphere is not placed inferior to the glenoid neck or there is a significant medial erosion of the glenoid fossa (Fig. 19-13A,B).10,79,81,83
avoid early glenoid loosening, and enhances bony fixation of the cementless implanted glenoid base plate (metaglene) (Fig. 19-11). The humeral component was uncemented with a corresponding polyethylene cup with various depths. It was further redesigned into the Delta3TM arthroplasty (DePuy International Ltd, Leeds, UK) available in 1991 (Fig. 19-12). Later, a very similar design was introduced in the market by several other companies (AequalisTM reverse shoulder arthroplasty, Tornier Inc., France; SRATM reverse shoulder arthroplasty, Lima Inc., Italy; Zimmer® Anatomical Shoulder Invers-ReversTM, Zimmer Inc., Warsaw, Indiana; Zimmer® Trabecular MetalTM Reverse Shoulder System, Zimmer Inc., Warsaw, Indiana). The common principle of all this prosthesis followed the idea of Grammont with a hemispherical glenoid component, with a center of rotation at the glenoid bone-implant interface, with the metaglene fixed directly on the glenoid resection surface, and a humeral component with a concave epiphyseal design with a 155-degree orientation of the humeral PE-liner. This reverse ball-and-socket design by Grammont has two major advantages. It has a large glenoid hemisphere with no neck and a small humeral cup with a nonanatomical inclination angle of 155 degrees, which covers less than half of the glenosphere. This design with a large hemisphere with no neck on the glenoid side medializes the center of rotation and places the center of rotation at the surface of the glenoid bone (Figs. 19-9B and 19-11). All the forces acting on the prosthesis pass through the fixed center of rotation; thus, the neckless design with a hemispheric glenoid component transforms the torque created by former designs into compressive forces at the prosthesis-bone interface (Fig. 19-11). This solved the formerly inevitable problem of loosening of the convex glenoid component. This reduces the torque forces on the component and creates less risk of loosening. Furthermore, it provides a fixed center of rotation, preventing the superior migration of the humeral head and increases the length of the deltoid muscle (Fig. 19-9B). The large diameter also allows greater range of motion before impingement can occur. The nonanatomical inclination (155 degree) of the humeral component places the humeral component in an inferior position, making it easier to increase the length of the deltoid muscle, and places the deltoid muscle under tension. Because of the medialization of the glenosphere, an external rotation cannot be restored and impingement inferiorly between the humeral component and scapula, resulting in a “notch,” is a concern when the glenosphere is not placed inferior to the glenoid neck or there is a significant medial erosion of the glenoid fossa (Fig. 19-13A,B).10,79,81,83
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree