Reverse Shoulder Arthroplasty for Proximal Humerus Fractures
Michael M. Hussey
Brandon M. Steen
Mark A. Frankle
DEFINITION
Fractures involving the proximal region of the humerus that provide the supporting framework for the glenohumeral articulation are termed proximal humerus fractures.
These fractures typically occur along the physeal lines as described by Ernest Codman in 1934, most commonly involving the surgical neck and lesser and greater tuberosities.
Proximal humerus fractures remain the second most common fracture of the upper extremity and the third most common fracture in patients older than age 65 years.1
ANATOMY
The proximal humerus is composed of the humeral head, greater tuberosity, lesser tuberosity, and upper humeral shaft. In the normal shoulder, the head is covered with articular cartilage which allows for a smooth articulation with the glenoid. The greater and lesser tuberosities are separated by the intertubercular groove through which the long head of biceps tendon traverses.
The superior most point of the humeral head is on average 8 mm cephalad to the greater tuberosity11 and shown to average 30 degrees of retroversion in relation to the shaft.18
The upper edge of the pectoralis major tendon is on average 56 mm inferior to the top of the humeral head.15
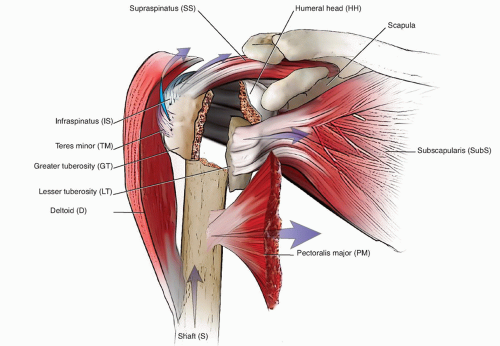
The rotator cuff complex (subscapularis, supraspinatus, infraspinatus, teres minor) inserts onto the proximal humerus at the lesser and greater tuberosities. This complex works in concert to not only bring about intricate movements of the arm in space but also to secondarily stabilize the glenohumeral joint.
This region consists primarily of metaphyseal bone surrounded by a vascular network of the circumflex humeral vessels.
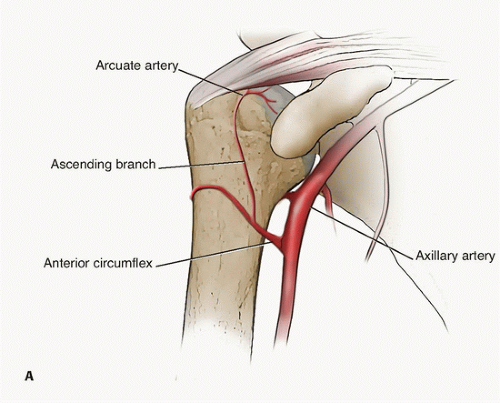
The humeral head receives the majority of its vascular supply from the arcuate artery, a terminal branch of the anterior circumflex humeral artery (FIG 1A). Disruption of this vessel by fracture or iatrogenic causes has the potential to cause avascular necrosis and a poor outcome.
The posterior aspect of the greater tuberosity and head are supplied by branches of the posterior circumflex humeral artery9(FIG 1B).
The axillary nerve courses around the lateral aspect of the proximal humerus at an average of 61 mm from the midportion of the acromion.4
PATHOGENESIS
These injuries are most commonly due to a ground level fall onto the upper extremity in the elderly population with osteopenia.
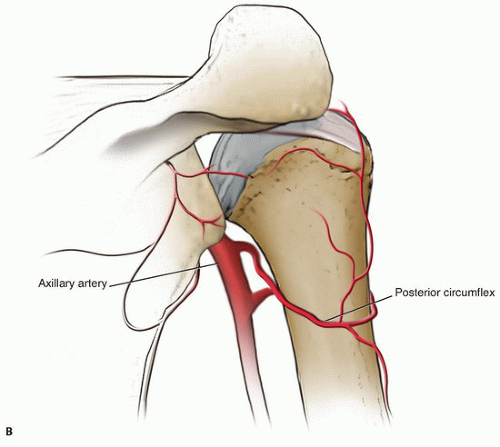
FIG 1 • (continued) B. Posterior view. The posterior circumflex humeral artery sends many branches to supply the posterior head and greater tuberosity.
The majority of fractures are minimally displaced. However, if sufficient energy and diminished bone density exist, displacement can occur, which often follows characteristic fracture patterns as described by Neer.16
The Neer classification is commonly used to describe these injuries and is based on displacement and/or angulation of the fracture “parts.”16 The use of this classification has led to a better understanding of the prognostic implications of treatment as well as improved therapeutic interventions.
Due to multiple tendon attachments onto the proximal humerus, these parts undergo characteristic patterns of displacement.
The greater tuberosity is frequently displaced posterosuperiorly by the strong external rotators of the cuff. The lesser tuberosity is pulled medially by the subscapularis, and the shaft is pulled superiorly and medially by the deltoid and pectoralis major, respectively (FIG 2). The head typically maintains a concentric alignment with the glenoid due to capsular attachments, except for cases of dislocation or valgus collapse.
A valgus impacted fracture involves lateral rotation and collapse of the head onto the shaft, with displacement of the tuberosities and impaction of the underlying cancellous bone.
NATURAL HISTORY
Significant displacement occurs in less than 15% of all proximal humerus fractures.16
Left untreated, displaced three- and four-part fractures are often associated with poor patient outcomes, leading to chronic pain, loss of motion, and impairment with activities of daily living.
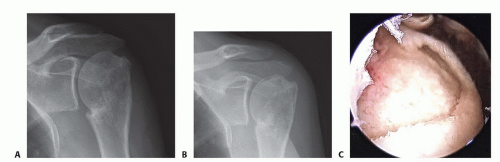
Significant fracture comminution and displacement can potentially lead to avascular necrosis of the humeral head (FIG 3A-C). Predictors of humeral head ischemia include posteromedial metaphyseal head extension less than 8 mm, loss of the medial hinge, four-fragment fractures, and angular displacement of the head greater than 45 degrees.10
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history should be taken from the patient to include age, mechanism of injury, arm dominance, occupation, prior history of falls, and smoking status.
Also critical to consider in the elderly population is functional status, living situation, and medical comorbidities.
A detailed physical examination should be performed to assess level of trauma sustained, presence of concomitant injuries, and degree of dysfunction of the injured extremity.
The neurovascular status of the extremity should be performed. Distal radial and ulnar pulses should be palpated and compared to the uninjured arm. Distal motor and sensory examinations in the axillary, musculocutaneous, median, radial, and ulnar nerve distribution should be evaluated. This is extremely important in polytrauma patients and those sustaining high-energy trauma.
The soft tissue envelope should be evaluated for ecchymoses, open wounds, abrasions, and presence of skin tenting.
Ability to perform active arm elevation and assessment of the rotator cuff is difficult secondary to pain and fracture displacement.
Of paramount importance is determination of axillary nerve injury, which can be achieved by testing sensation and deltoid motor function.
IMAGING AND OTHER DIAGNOSTIC STUDIES
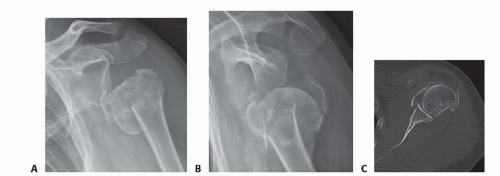
In fracture cases, patient discomfort often limits radiographic analysis. Typically, a true scapular anteroposterior(AP), scapular Y, and axillary lateral radiographs are obtained to evaluate details of the fracture and whether or not a dislocation is present. A Velpeau view may be helpful in situations where obtaining an axillary lateral is extremely painful (FIG 4A,B).
In certain instances, computed tomography (CT) scan can be obtained to better characterize fracture pattern and aid
in preoperative surgical planning. CT can be very helpful to evaluate head impaction as well as tuberosity fragmentation and displacement (FIG 4C).
DIFFERENTIAL DIAGNOSIS
Humeral shaft fracture
Rotator cuff tear
Scapular fracture
Glenohumeral dislocation
Brachial plexus injury
NONOPERATIVE MANAGEMENT
Conservative management is the mainstay of treatment for the majority of proximal humerus fractures, as most are minimally displaced. These injuries have a very low nonunion rate.
Most patients are able to resume normal activities once fracture healing is achieved. Some loss of motion is typically well tolerated due to the large arc of motion of the shoulder.
Patients are placed in a sling or shoulder immobilizer for comfort during the first 10 to 14 days. They are instructed to start elbow/wrist/hand range-of-motion (ROM) exercises immediately after injury to prevent stiffness.
Once pain subsides, patients are encouraged to perform daily gentle ROM exercises of the shoulder such as pendulums.
When fracture consolidation is evident on follow-up radiographs (typically between 4 and 6 weeks), increased passive and active ROM exercises are added to the therapy regimen.
By 3 or 4 months, strengthening is begun and resumption of normal daily activities usually achieved.
SURGICAL MANAGEMENT
Proximal humerus fractures that have significant comminution and displacement are commonly managed by surgical means. In the young population and in those with good bone quality, every effort should be taken to obtain an anatomic reduction and fixation of the fracture.
Frequently used methods include open reduction internal fixation (ORIF), closed reduction percutaneous pinning (CRPP), and intramedullary nail fixation.
Prosthetic replacement is considered in three- and four-part fractures, particularly in the elderly with osteoporotic bone and in those with significant head involvement.
Hemiarthroplasty has been used most commonly but has been met with mixed results. Postoperative ROM and functional outcomes as well as reduction in pain have proven unpredictable, as hemiarthroplasty relies heavily on correct tuberosity positioning and healing.2,12,17
More recently, reverse shoulder arthroplasty (RSA) has been used as primary treatment for these complex injuries. RSA can be an invaluable option in the elderly, osteoporotic patient with a comminuted fracture, where tuberosity reconstruction and healing is felt to be difficult and unpredictable. Inherent in the design of the prosthesis, a good outcome is less dependent on tuberosity quality and healing, allowing for more confidence in reconstruction with varied pathology. 6 The biomechanical advantage of RSA allows the deltoid to take a greater role in arm elevation and abduction.
Preoperative Planning
Assessment of deltoid function is paramount when deciding whether to perform RSA due to its reliance on deltoid motor function.
Plain radiographs of the uninvolved arm can be obtained to assist in preoperative planning and templating.
If ORIF is still being considered in the treatment plan, a CT scan can be useful to evaluate tuberosity and head displacement prior to surgery.
Positioning
The patient is placed in the beach-chair position with all bony prominences padded appropriately. The affected extremity is draped free to allow uninterrupted access.
Complete arm extension and adduction should be ensured prior to starting to facilitate glenoid exposure and access to the humeral canal. If a cutout is not present on the bed, then the patient should be moved as far lateral as possible to ensure impingement free ROM.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree