Large angular deformities can be a challenge when performing primary total knee replacement. Some investigators have advocated the use of increased component constraint in these settings. The goal of this study was to determine the location and extent of damage to a consecutive series of retrieved constrained tibial inserts used in primary arthroplasty. There was significant post and articular damage in retrieved implants. Reliance on the polyethylene post for implant stability was associated with post and articular surface damage and may be a potential source of failure. Attempts to achieve implant stability using soft tissue techniques seem justified.
- •
Alternative techniques should be considered for deformity correction and joint stability.
- •
Soft tissue techniques are the gold standard for knee balancing.
Introduction
The principle for success in primary total knee arthroplasty is ensuring a well-aligned and balanced construct. The soft tissue aspect of knee replacement is crucial for stability and for optimizing kinematic function. However, knees with large angular deformities are often difficult to correct using established soft tissue techniques and may result in instability and ultimately implant failure. In these situations the use of additional constraint using a conforming polyethylene post might enhance stability.
The use of constrained condylar implants in primary total knee arthroplasty has been previously described. These implant systems have used a conforming polyethylene post that articulates with a femoral component with a matching intercondylar box. The intent of this post-box constraint is to resist not only posterior tibial translation relative to the femur (ie, posterior stabilization) but also to provide resistance to varus/valgus bending moments.
The femoral component in such constrained knee implants was traditionally used with a supplemental femoral rod. There is increasing experience with so-called nonmodular devices that do not use augmented femoral rods. Anderson and colleagues reported excellent results using this system in a series of 61 patients with preoperative valgus alignment; only 1 failure occurred caused by patellar instability. However, little information exists regarding the integrity of the polyethylene post and the articular surface ex vivo. This study evaluated the location and extent of damage of a consecutive series of retrieved nonmodular constrained condylar implants to determine what clinical or radiographic factors may be associated with observed damage modes.
Methods
The implant retrieval archive at our institution is an institutional review board approved and Health Insurance Portability and Accountability Act–compliant registry. All explanted implants are identified by type and manufacturer and subsequently cataloged into the registry. We identified 56 consecutive nonmodular constrained condylar implants (Exactech, Gainsville, FL) that were explanted between August 1998 and August 2005. The nonmodular design uses a highly conforming central polyethylene post that fits into a square femoral box configuration with less than 1 mm of tolerance between the outer surface of the post and the inner surface of the box. The femoral component is stemless by design to avoid the need for additional diaphyseal fixation.
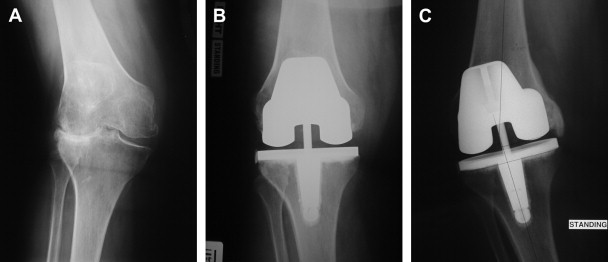
The implants were retrieved from 35 women and 21 men with a mean age of 66 years at the time of explanation. All patients had their index arthroplasty at our institution. The preindex total knee alignment was valgus in 41 knees and varus in 15 knees. The primary indication for the constrained implant was noted as the inability to achieve soft tissue balance and knee stability at the time of surgery ( Fig. 1 ). These 56 implants were revised at a mean of 21.2 months following the index procedure. The reason for revision was infection in 19 cases (34%), instability in 12 (21%), aseptic loosening of either the femoral or tibial component in 10 (18%), stiffness in 6 (11%), recurrent effusions in 5 (9%), and unknown in 4 (7%).
Each retrieved tibial insert was subsequently analyzed. The polyethylene posts were divided into 5 regions: superior, anterior, medial, lateral, and posterior. Each region was then divided into 4 quadrants ( Fig. 2 ). The articular surface was divided into 8 zones (4 medial and 4 lateral) and then subdivided further into 4 quadrants ( Fig. 3 ). Each region of interest was graded using the method described by Hood and colleagues. Using 10× magnification, each quadrant was subjectively graded on a 0 to 3 scale for each of 7 damage modes (deformation, embedded cement, pitting, scratching, burnishing, abrasion, and delamination) by a pair of observers (DP and JC) blinded to any of the clinical data. A damage score of 0 reflects no damage for that mode in that quadrant, whereas a damage score of 3 represents more than 50% of a quadrant having evidence of that particular damage mode. Using this grading system, a total damage score can be calculated based on number of damage modes, extent of damage score, number of quadrants, and the number of orientations investigated ( Table 1 ).
Patient demographics were recorded, including age at index surgery, gender, body mass index, prerevision alignment, reason for revision, and length of implantation. Comparisons were made of wear areas for each mode between the 2 surfaces using paired Student t -tests. Analysis of variance was used to examine differences in wear scores among regions. Regression analysis was used to examine the effects of clinical factors and radiographic alignment on wear scores. The type I error rate was set at 0.05.
Methods
The implant retrieval archive at our institution is an institutional review board approved and Health Insurance Portability and Accountability Act–compliant registry. All explanted implants are identified by type and manufacturer and subsequently cataloged into the registry. We identified 56 consecutive nonmodular constrained condylar implants (Exactech, Gainsville, FL) that were explanted between August 1998 and August 2005. The nonmodular design uses a highly conforming central polyethylene post that fits into a square femoral box configuration with less than 1 mm of tolerance between the outer surface of the post and the inner surface of the box. The femoral component is stemless by design to avoid the need for additional diaphyseal fixation.
The implants were retrieved from 35 women and 21 men with a mean age of 66 years at the time of explanation. All patients had their index arthroplasty at our institution. The preindex total knee alignment was valgus in 41 knees and varus in 15 knees. The primary indication for the constrained implant was noted as the inability to achieve soft tissue balance and knee stability at the time of surgery ( Fig. 1 ). These 56 implants were revised at a mean of 21.2 months following the index procedure. The reason for revision was infection in 19 cases (34%), instability in 12 (21%), aseptic loosening of either the femoral or tibial component in 10 (18%), stiffness in 6 (11%), recurrent effusions in 5 (9%), and unknown in 4 (7%).





