Oropharyngeal dysphagia is common in patients with Wallenberg syndrome. Although the functional outcome is good for most patients, the risk of inhalation pneumonia is high. Nevertheless, some patients exhibit permanent and chronic oropharyngeal dysphagia with pharyngeal residue and bronchial aspiration. In such cases, the central pattern generator for swallowing may be affected . We report 2 cases for which we proposed a novel strategy based on repetitive transcranial magnetic stimulation (TMS), electrical stimulation and surgery.
Currently, therapeutic possibilities for oropharyngeal dysphagia include speech-language therapy and gastrostomy. New perspectives include cortical modulation involving peripheral electrical stimulation and cortical magnetic stimulation . Several studies have assessed the efficacy of stimulation techniques on brainstem stroke. In one, repetitive TMS (rTMS) was successfully applied to the motor area of both hemispheres in patients with acute lateral medullary infarction . However, patients also often present paralyzed hemi-pharynx with pharyngo-esophageal dyssynergia, for which surgery could be useful. Therefore, we hypothesized that rTMS with electrical stimulation followed by surgery in patients with aphagia after brainstem stroke could help in recovery of the swallowing central pattern generator because the surgery should help in recovery of the upper esophageal sphincter opening.
The 2 patients who volunteered to take part in the treatment (both males, 57 and 44 years old) had aphagia due to a brainstem stroke that occurred 3 years previously. Patients had no other functional incapacity and both were active at home. Nutrition was only possible by gastrostomy because of severe aspirations.
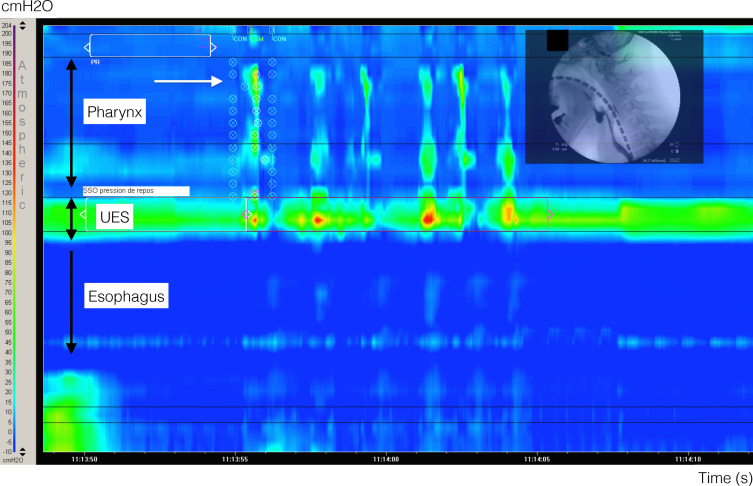
Swallowing was evaluated by standardized videofluoroscopic barium swallow testing (Flexiview 8800, General Electric, United Medical Technologies Corp., Fort Myers, FL, USA) associated with high-resolution manometry (MMS, Tubingen, The Netherlands) to characterize aspiration , pharyngeal residue, pharyngeal peristalsis and upper esophageal opening . rTMS was previously described by 2 of the authors . Briefly, mylohyoid electromyography responses were detected by using 2 pairs of surface electrodes, and cortical stimulations involved a Magstim super-rapid stimulator (Magstim, Whitland, Dyfed, UK) equipped with an air-refreshed, double, 70-mm, figure-of-eight coil (peak magnetic field = 2 T). rTMS was performed on the best point that permitted stimulation of the mylohyoid cortical area of each hemisphere. Each hemisphere was stimulated for 10 min (1 Hz at 20% above the threshold value). Stimulation was repeated each day for 5 consecutive days and 5 times at 3-month intervals. During rTMS, surface submental electrical stimulations (TENS Neurostimulator, Schwa-medico GmbH, D 35630 Ehringshausen, Germany) were performed . Surgery was performed after the appearance of the initiation of the swallowing reflex, which was not initially present, after the application of rTMS and TENS.
Pharyngeal resection of the non-contractile pharynx involved the lateral cervical approach with the patient under general anesthesia. The cricopharyngeal muscle was dissected and opened from the upper portion of the thyroid ala to the lower part of the pyriform sinus. A large portion of the inferior constrictor muscles and lateral pharynx mucosa was removed, as was 1 or 2 cm of the lateral thyroid ala. For the pharyngeal constrictor myotomy, a posterior midline muscular incision was made around the upper esophageal sphincter (4 cm high), preserving the mucosal integrity. Finally, a system of laryngeal suspension was created by using non-resorbable material . Swallowing was evaluated by videofluoroscopy and manometry after each rTMS session and at 1, 3 and 6 months after surgery. All treatments proposed are typically used for post-stroke dysphagia.
On initial evaluation, the patients were unable to swallow because of lack of initiation of the swallowing reflex. The consequences were 100% stasis in the paralyzed hemi-pharynx with massive and passive bronchial penetration. Manometry revealed no pharyngeal peristalsis and the upper esophageal sphincter pressure increased during swallowing ( Fig. 1 ). Evaluation of swallowing function demonstrated progressive improvement in pharyngeal peristalsis with rTMS and TENS, with the appearance of a swallowing reflex and pharyngeal peristaltism. Nevertheless, the patient showed continued stasis in the paralyzed hemi-pharynx with aspirations, and the upper esophageal sphincter did not open completely during swallowing. Therefore, we proposed functional surgery to prevent the onset of pharyngeal stasis and to improve swallowing.