Replacement Arthroplasty for Acute Fractures
Mark Frankle David
Fisher Mark Mighell
INTRODUCTION
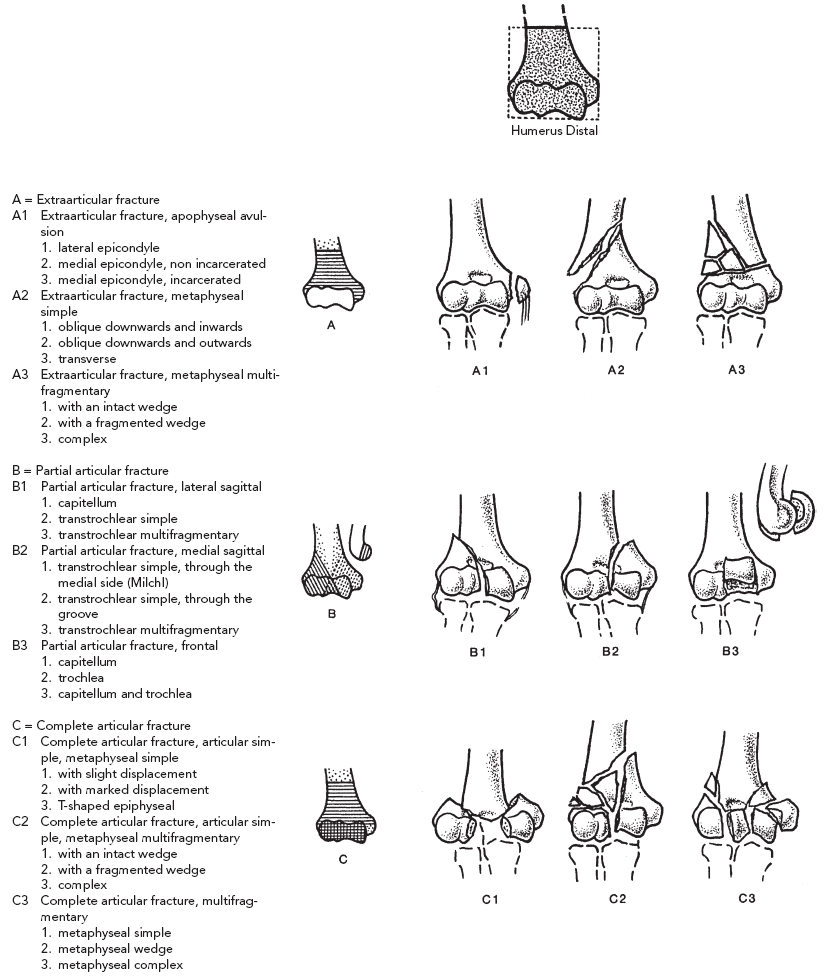
Displaced intraarticular fractures of the distal humerus are both rare and difficult to treat. They occur in fractures (1). The most commonly used classification is the one described by the Association for the Study for Internal Fixation (ASIF), which is a fracture classification system for distal humerus fractures (Table 26-1). The principle is to divide the fracture type into three areas based on the anatomic level of the fracture and involvement of the articular surface. These fracture types are as follows: Type A, where the fracture is extraarticular only; Type B, where the fracture extends into the articular surface but maintains continuity with the metaphysis of the distal humerus; and Type C, where the fracture completely disrupts the articular surface from the humeral shaft fragments. Each type can be further divided into groups and then again divided into subgroups depending on the morphologic complexities of the fracture. There are 27 possible descriptions for distal humerus fractures using this classification. This system has been used in an attempt to compare the extent of fracture complexity, the difficulties inherent in their treatment, and prognosis within study groups.
The AO principles of anatomic reduction, stable internal fixation, preservation of blood supply, and early active pain-free mobilization are paramount in elbow fracture reconstruction (2). Open reduction and internal fixation (ORIF) is the procedure of choice for most displaced fractures of the distal humerus; however, it is often difficult to achieve stable fixation in elderly patients with poor bone quality and extensive articular comminution. Fair to poor outcomes were reported in 25% of patients treated with ORIF for distal humerus fractures. Up to 70% required revision surgery, which was associated with high complication rates (3). Nonunion, malunion, posttraumatic arthritis, and joint stiffness can result in a painful elbow and poor patient satisfaction (3,4,5,6,7).
Total elbow arthroplasty has been described as an option for salvage of supracondylar humeral fracture nonunions or posttraumatic arthritis in elderly patients (4,5,6,7). Cobb
and Morrey were the first to report their results of total elbow arthroplasty (TEA) as the primary index operation for acute fractures of the distal humerus in elderly patients (8). Although effective treatment, the incidence of those people who may be candidates for arthroplasty was low. Only 21 patients with acute distal humerus fractures at the Mayo Clinic were treated with arthroplasty over 10 years. Subsequently, several clinical reports have also supported elbow arthroplasty as an alternative to primary fracture fixation in carefully selected patients (9,10,11).
and Morrey were the first to report their results of total elbow arthroplasty (TEA) as the primary index operation for acute fractures of the distal humerus in elderly patients (8). Although effective treatment, the incidence of those people who may be candidates for arthroplasty was low. Only 21 patients with acute distal humerus fractures at the Mayo Clinic were treated with arthroplasty over 10 years. Subsequently, several clinical reports have also supported elbow arthroplasty as an alternative to primary fracture fixation in carefully selected patients (9,10,11).
TABLE 26-1 CLASSIFICATION OF DISTAL HUMERUS FRACTURES | |
|---|---|
|
Fracture classification as discussed earlier is an important consideration in deciding treatment. Extensive intraarticular comminution is not the only determining factor. For example, in a series of 16 patients, with no history of an inflammatory arthropathy, who had a primary TEA for fracture, 13% had the AO classification A3, 13% were B3, and 74% were C3 (9). Extensive osteopenia and underlying inflammatory arthropathies are significant factors in considering TEA for acute fracture. In contrast, the decision to attempt fixation with the strategy of later converting to an arthroplasty if the fixation fails must be tempered. In a retrospective study of patients older than 65 years of age with complex elbow fractures, those who where treated with primary TEA had better outcome than those converted to TEA after the primary open reduction and internal fixation failed (12). The following chapter will review the literature concerning patient selection, evaluation and workup, outcomes, complications, surgical technique, and future direction of elbow arthroplasty for acute distal humerus fractures.
PATIENT SELECTION AND OUTCOMES
In 1997 Cobb and Morrey reported their results of TEA as primary treatment for distal humeral fractures in elderly patients (8). A retrospective review over 10 years included 129 acute distal humeral fractures (125 adults) that presented for care. Twenty patients (21 elbows) who had an age range from 48 to 92 years were treated with a primary TEA. The indications for arthroplasty were an extensively comminuted acute fracture and underlying articular destruction from rheumatoid arthritis in nine patients or ten elbows. The remaining 11 patients did not have rheumatoid arthritis but were far older than age 65 years. Five out of the 11 had an AO classification Type C3 distal humerus fracture.
Except for three patients who died, all were followed for a minimum of 2 years. Fifteen elbows had excellent results, and five had good results using the Mayo elbow performance score (Table 26-2). The mean arc of flexion-extension was 130-25 degrees. There were no fair or poor results.
In 1999 Frankle and colleagues reported their retrospective evaluation of all intraarticular distal humeral fractures in female patients older than age 65 years treated between 1990 and 1996 (12). Twenty-four patients with 24 fractures were treated either with primary TEA or internal fixation. All fractures were classified as AO/ASIF 13C fractures. All patients were followed for a minimum of 2 years. Using the Mayo performance score, the primary TEA group had a more predictable outcome compared to the internal fixation group (Fig. 26-1). There were 11 excellent and one good in the primary arthroplasty group, and only four excellent, four good, one fair, and three poor in the internal fixation group. None of the arthroplasties required revision, whereas the three poor results of internal fixation were revised.
TABLE 26-2 MAYO ELBOW PERFORMANCE SCORE | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Frankle and colleagues also reported outcomes in 40 patients with complex elbow fractures treated primarily with TEA versus those treated primarily with ORIF and then secondarily converted to TEA. Twenty-one patients with an age range from 52 to 88 years were initially treated with TEA; whereas 19 patients with an age range of 45 to 79 years were initially treated with ORIF and later converted to a salvage TEA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree