About 9% of shoulder girdle injuries involve damage to the acromioclavicular (AC) joint.16
The AC joint separation involves disruption of the AC ligaments, with varying degrees of injury to the coracoclavicular (CC) ligaments, deltoid, and trapezius muscle attachment.
The AC joint injuries are classified by the the severity of injury, radiographic findings including the position of the clavicle relative to the acromion and reducibility of the AC joint with shoulder shrugging (Table 1).
The AC joint is a diarthrodial joint that is innervated by the lateral pectoral nerve and the suprascapular nerve.
The articular surfaces of the AC joint are made up of hyaline cartilage and separated by an intra-articular meniscus type of structure, all surrounded by a joint capsule with a synovial lining.
The AC joint primarily rotates as well as translates in the anteroposterior (AP) as well the superoinferior plane. Normal scapular motion consists of substantial rotations around three axes and plays a major role in the motion at the AC joint. The scapula (acromion) can protract and retract, using the AC joint as a pivot point.
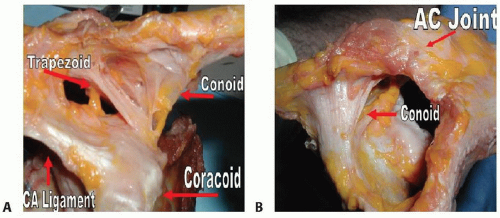
The static stabilizers of the AC joint includes the AC ligaments (superior, inferior, anterior, and posterior) and the CC ligaments (trapezoid and conoid). The dynamic stabilizers consist of the deltoid and trapezius muscles.
The AC joint capsule and the capsular ligaments (mainly the superior and posterior AC capsular ligaments) are the primary restraints to anterior-to-posterior translation of distal clavicle.7
The coracoclavicular ligaments (trapezoid and conoid) ligaments span the CC space and contribute to vertical stability. The trapezoid attaches on the undersurface of the clavicle at an anterolateral position. The conoid is a broad stout ligament located in a posterior and medial position (conoid tubercle). Both the trapezoid and conoid are posterior to the pectoralis minor attachment on the coracoid (FIG 1).
The AC and CC ligaments all contribute to the prevention of motion in all planes. The conoid ligament has the highest in situ forces with superior loads, regardless of the integrity of the AC ligaments. The AC ligaments are the main restraints to posterior and anterior translation. However, when the AC ligaments are transected, the conoid is the primary restraint to anterior loads and the trapezoid is the primary restraint to posterior loads.4
The mechanism of most AC joint injuries is a direct blow to the point of the shoulder (lateral acromion) with the arm adducted.
Indirect injury occurs by falling on an adducted outstretched hand or elbow, causing the humeral head to translocate superiorly and drive the humeral head into the acromion.
Most patients with type I or type II AC joint separations typically have full recovery with no long-term sequelae. However, some patients continue to be symptomatic. In one study, up to 27% of patients with types I and II injuries had persistent pain and required a surgical procedure. Some patients treated nonoperatively continued to have instability and pain with provocative tests (level IV evidence).11
Most patients with type III separations do well with conservative treatment. In a survey of Major League Baseball team physicians, 80% of athletes treated nonoperatively had complete pain relief and normal function (level IV evidence).9 Studies have failed to show a statistical difference in the return to activity (level IV evidence).12
Types IV, V, and VI AC joint separations do poorly without operative intervention (level V evidence).2 Persistent pain and functional deficit is attributed to a chronically dislocated AC joint with severe soft tissue disruption.
The mechanism of injury is an important history finding that clues one into a possible AC joint injury.
Pain in the AC joint region and obvious deformity of the AC joint are common physical presentations of AC joint separation.
In the absence of an obvious deformity, AC joint injury can be identified by a triad of point tenderness, positive pain at the AC joint with cross-arm adduction, and relief of symptoms by injection of a local anesthetic into the AC joint.
Special tests for AC joint pathology:
AC joint compression (shear) test: Isolated painful movement at the AC joint in conjunction with a history of direct trauma indicates AC joint pathology.
Cross-arm adduction test: Look for pain specifically at the AC joint. Pain at the posterior aspect of shoulder or lateral shoulder might indicate other pathology.
Paxinos test21: In a positive Paxinos test, tenderness or pain is present/worsened in the AC joint region when the examiner applies pressure to the acromion in an
anterosuperior direction and downward pressure to the midpart of the clavicular shaft.
Table 1 Classification of Acromioclavicular (AC) Joint Injuries
Type
Description
Illustration
Examination Findings
Radiographic Findings
I
Sprain of the AC joint with all ligaments intact
Mechanism of injury consistent with AC joint injury
No evidence of instability
Point tenderness at the AC joint and positive provocative tests
Radiographs are normal.
II
Rupture of AC ligaments
Sprain of coracoclavicular (CC) ligaments
Mild subluxation of the AC joint can be observed with stress examination.
Radiographs of the lateral end of the clavicle may be slightly elevated, but stress views fail to show a 100% separation of the clavicle and acromion.
III
Complete disruption of both the AC and CC ligaments without significant disruption of the deltoid or trapezial fascia
The clavicle is unstable in both the horizontal and vertical planes.
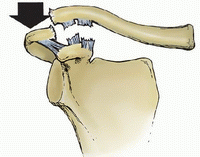
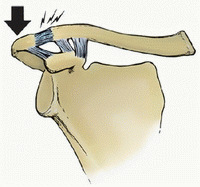
The upper extremity is usually held in an adducted position with the acromion depressed while the clavicle appears high-riding, but in reality, the acromion and the rest of the upper extremity is displaced inferior to the horizontal plane of the lateral clavicle.
Radiographs show up to 100% increase in the CC interspace.
IV
Complete disruption of both the AC and CC ligaments
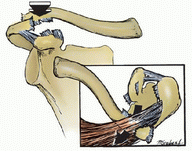
The distal clavicle is posteriorly displaced into the trapezius muscle and may tent the posterior skin.
Evaluation of the sternoclavicular (SC) joint is necessary to rule out anterior SC joint dislocation.
Posteriorly displaced clavicle can be seen on axillary view, which is always obtained in the standard radiographic evaluation of the AC joint.
V
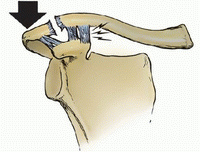
AC and CC ligaments are disrupted.
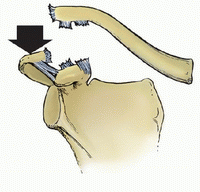
Severe droop secondary to anteroinferior translation of the scapula around the thorax due to the weight of the arm and the geometry of the chest wall. This is considered the third translation of the scapula with loss of the clavicular strut.
Reduction of the distal clavicle with shoulder shrug differentiates type III from type V (distal clavicle buttonhole through soft tissue sleeve).
Trapezial and deltoid fascia disrupted. Two to three times increase in the CC distance or a 100%-300% increase in the clavicle-to-acromion radiographic distance.
VI
Inferior dislocation of distal clavicle
Reduction may be blocked from interposition of the intact posterosuperior AC ligaments within the AC interval. Mechanism is thought to be severe hyperabduction and external rotation of the arm combined with retraction of the scapula
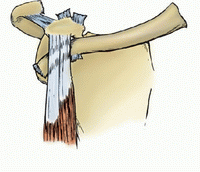
The distal clavicle is found in two orientations, either subacromial or subcoracoid, behind the intact conjoined tendon.
O’Brien test: Symptoms at the top of the joint must be confirmed by examiner palpating the AC joint. Anterior glenohumeral joint pain suggests labral or biceps pathology.
The AC joint is more superficial and surrounded by less soft tissue than the glenohumeral joint. The AC joint may be better visualized if a reduced penetration strength is used compared to standard radiographs of the glenohumeral joint.
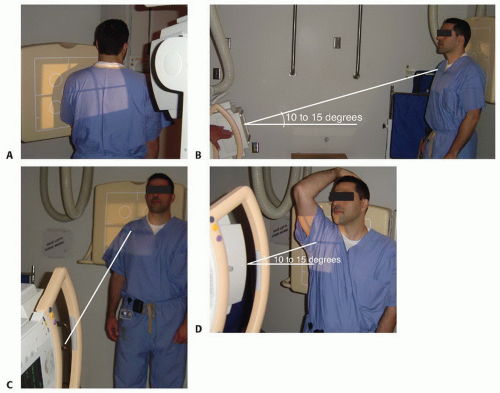
Standard radiographs at authors institution include AP view, supraspinatus outlet view (FIG 2A), and axillary and Zanca views.
A Zanca view is made by tilting the x-ray beam 10 to 15 degrees toward the cephalic direction (FIG 2B,C). An increase in the CC distance (usually 1.1 to 1.3 cm) of 25% to 50% over the normal side indicates complete CC ligament disruption. A normal CC interspace (average 1.1 to 1.3 cm), in conjunction with a complete dislocation of the AC joint, may indicate a coracoid fracture. This is better seen on a Stryker notch view (FIG 2D).
The AC joint width is normally 1 to 3 mm and decreases with age. The width seen on radiographs is influenced by the individual variability of obliquity of the joint in relation to the x-ray beam.
Although seldom necessary and mainly a historical practice, stress views (5 to 10 pounds placed in the ipsilateral hand) with increased CC interspace on the AP view may help differentiate between type II and type III injuries.
An axillary view of the shoulder is important in differentiating a type III from a type IV AC joint injury. Coracoid base fractures can also be identified on this view.
Bone scan may help confirm subtle AC joint pathology and arthrosis but is rarely required in clinic.
Cervical spine pathology
Trapezial spasm
Scapular dyskinesia
Hyperlaxity
Distal clavicle or acromion fracture
Coracoid fracture
Glenohumeral pathology (impingement, rotator cuff, Hill-Sachs, Bankart, superior labral anterior posterior [SLAP] lesion, biceps)
Ulnar paresthesias
Thoracic outlet syndrome
The main goals of treatment are to achieve a pain-free shoulder with full range of motion and strength and no limitations in activities.
Most type I and type II AC joint separations are treated in a nonoperative fashion.
Treatment begins with a sling, ice, and a brief period of immobilization only for pain control. Rehabilitation is started as soon as tolerated.
The rehabilitation program consists of four phases3:
Pain control, immediate protective range of motion, and isometric exercises
Strengthening exercises using isotonic contractions
Unrestricted functional participation with the goal of increasing strength, power, endurance, and neuromuscular control
Return to activity with sports-specific functional drills
Type III injuries:
These patients are usually evaluated on a case-by-case basis, taking into account variables like hand dominance, occupation, heavy labor, position and sport requirements (quarterbacks, pitchers), scapulothoracic dysfunction, and risk for reinjury.
In a meta-analysis of 1172 patients, 88% of those treated with surgery and 87% of those treated without surgery had satisfactory outcomes (level IV evidence).12
In patients with type III injuries treated nonoperatively versus operatively, there was no difference in strength at 2 years of follow-up (level IV evidence).19
Schlegel et al17 found that only 20% of patients reported a suboptimal outcome with conservative care. Objective studies showed that patients had no limitation of shoulder motion in the injured extremity and no difference compared with the unaffected extremity in rotational shoulder muscle strength. A finding that may affect heavy laborers was a decrease of 17% in bench press strength at the 1-year follow-up (level IV evidence).
Currently, there is inconclusive evidence to support for surgical treatment of type III AC joint dislocations.2,18 If symptoms persist for greater than 3 months—including increased pain, impingement due to scapular dyskinesia, decreased strength, inability to get the arm into a cocking position in throwing, and painful instability, especially posterior instability with the clavicle abutting the anterior portion of the spine of the scapula— then operative intervention may be indicated. Clinical studies looking at the outcomes of patients treated for AC joint dislocation are plagued with multiple issues: most of the studies are retrospective in design; have a mixture of types III, IV, and V; have both acute and chronic dislocations in the same cohort; and are treated with multiple different techniques within the same cohort. Long-term follow-ups are not available. Furthermore, the study groups contain mixed patient population (laborers, throwers) and the outcome measures are not standardized.
Complete AC joint injuries (types IV, V, and VI) are usually treated operatively because of the significant morbidity associated with persistently dislocated joint and severe soft tissue disruption.
For type III AC joint separation, one approach is to treat these injuries conservatively for 12 weeks and consider surgical stabilization if persistent pain and instability exist. In an alternative approach, a type III AC joint separation can be primarily treated surgically especially in an athlete and high-demand patient to allow quicker return to work or play and limit the duration of painful disability.
Operative interventions can be broadly divided into the following:
AC joint stabilization using hook plates, pins, or K-wires
CC space stabilization using suture loop, screw, Endo-Button (Smith & Nephew, Andover, MA), suture anchor, and other similar devices
Ligament reconstruction: CC ligament and/or AC ligament reconstruction using autograft or allograft
Dynamic muscle transfer (proximally based conjoint tendon transfer)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree