Essentials of Diagnosis
- Auricular chondritis (spares the earlobe).
- Inflammation in other cartilaginous areas (eg, the nose, joints, trachea, ribcage, and airways) and in tissues rich in proteoglycans, such as the eyes and heart valves.
- Frequently associated with an underlying disorder such as systemic vasculitis, connective tissue disease, or myelodysplastic syndrome.
General Considerations
Relapsing polychondritis (RP) is an immune-mediated condition associated with inflammation in cartilaginous structures and other connective tissues throughout the body, including the ears, nose, joints, respiratory tract, and others. The incidence of RP is estimated to be approximately 3.5 cases/million people. Thirty percent of RP cases occur in association with another disease, usually some form of systemic vasculitis (particularly granulomatosis with polyangiitis [formerly Wegener granulomatosis]), connective tissue disorder (eg, rheumatoid arthritis or systemic lupus erythematosus), or a myelodysplastic syndrome. RP is often assumed to be “autoimmune” in nature, but the evidence for a true autoimmune pathogenesis is relatively weak. Some patients have been reported to have antibodies to type 2 collagen, but these assays are not widely available and their poor sensitivities and specificities make them inappropriate for general clinical use. In general, a cartilage biopsy is not required to make the diagnosis. Rather, the identification of cartilaginous inflammation in typical areas (auricular cartilage, nasal bridge, costochondral joints) and the exclusion of other possible causes suffice.
RP is associated with a broad range of clinical courses. One end of the disease spectrum includes intermittent bouts of auricular cartilage inflammation that respond quickly to treatment. The other end is characterized by widespread, aggressive cartilaginous inflammation that leads to serious end-organ complications. The greatest clinical challenge is identifying the presence of cartilaginous inflammation and instituting effective therapy before irreparable damage occurs in the involved organs.
Clinical Findings
| Feature Data | Data |
|---|---|
| Mean age at diagnosis | 47 years |
| Auricular chondritis | 90% |
| Reduced hearing | 37% |
| Nasal chondritis | 60% |
| Saddle-nose deformities | 25% |
| Laryngotracheal involvement | 52% |
| Ocular inflammation | 54% |
| Arthritis | 69% |
| Skin involvement | 25% |
| Aortic or mitral regurgitation | 8% |
| Vasculitis | 12% |
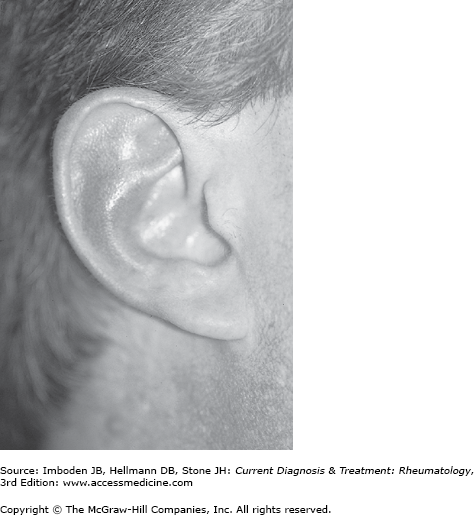
Unilateral or bilateral auricular chondritis is often the first disease symptom (Figure 28-1). The onset of auricular inflammation is usually quite abrupt and not subtle. The inflammation may be confused with cellulitis of the ear or even sunburn in more minor cases. A major clue to the diagnosis of RP is confinement of the inflammation to the auricular part of the ear, with sparing of the earlobe. The cartilaginous portions of the ears are erythematous and tender to touch. Swelling of the external ear canal may cause conductive hearing loss. RP may also be associated with sensorineural hearing loss, the mechanism of which remains obscure (vasculitis is often implicated, without proof).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree