Rehabilitation after Elbow Arthroplasty
Samuel A. Antuña
The goal of elbow replacement is to restore the function of the elbow joint as a link that positions the hand in space and as a stabilizer for power and fine motor function. The elbow must be mobile, stable, and pain-free to allow individual independence in activities of daily living. Rehabilitation after an elbow arthroplasty should include restoration of these essential requirements.
Any rehabilitation program must be individualized according to the characteristics of the implant that has been used. Stability of unlinked implants depends on the integrity of osseous and capsuloligamentous structures. It is essential to allow these structures to heal during the early postoperative period and at the same time avoid stiffness secondary to prolonged immobilization. Linked implants do not require the ligaments to be stable, allowing a more aggressive and prompt rehabilitation program.
The approach used for the implantation of the prostheses dictates the limitations in range of motion and the necessity of immobilization. Therefore, the therapist should have a thorough knowledge of the details of the surgical procedure, and he or she also should be familiar with the basic approaches in elbow arthroplasty and their implications with regard to triceps integrity. Additionally, the surgeon should communicate any special incidents during surgery that might influence the therapy program.
In this chapter we discuss the specific rehabilitation programs for the most commonly used elbow prostheses and emphasize the implications of different surgical techniques on the postoperative regimen. We provide detailed rehabilitation protocols for the clinician to use in patients with an elbow replacement.
ANATOMY AND FUNCTION
The anatomy of the elbow region has been discussed in detail in Chapter 19. However, some aspects that influence the rehabilitation plan should be emphasized.
The elbow has three independent joints that act together to allow motion in two planes: flexion-extension
and pronation-supination. It does not function as a simple hinge, allowing a valgus-varus movement during flexion of 3 to 4 degrees (1). Most activities require an arc of motion between 30 degrees of extension and 130 degrees of flexion. An arc of 100 degrees of forearm rotation, with 50 degrees of supination and pronation, is also required for these sedentary tasks (2). This arc of motion represents the minimum goal that we need to pursue during the rehabilitation program after elbow replacement.
and pronation-supination. It does not function as a simple hinge, allowing a valgus-varus movement during flexion of 3 to 4 degrees (1). Most activities require an arc of motion between 30 degrees of extension and 130 degrees of flexion. An arc of 100 degrees of forearm rotation, with 50 degrees of supination and pronation, is also required for these sedentary tasks (2). This arc of motion represents the minimum goal that we need to pursue during the rehabilitation program after elbow replacement.
The progression of passive and active-assisted strengthening is mainly dictated by the status of the triceps tendon because it is the only muscle that may be disrupted during surgery that has a significant impact on elbow range of motion. It is worth remembering that the triceps attaches to the tip of the olecranon through the Sharpey fibers but has a continuity with the anconeus and the posterior periosteum of the ulna that, if preserved, facilitates the postoperative function of the muscle. It is important to remember that the majority of muscles originating from the medial and lateral epicondyles traverse both the elbow and the wrist joints and that any alterations in these muscles may compromise elbow and wrist function. Moreover, any rehabilitation program must include wrist therapy to recover the complete function of these muscles.
The stability of the elbow is maintained by primary and secondary constraints (1,3). The primary constraints are the congruence of the ulnohumeral joint and the capsuloligamentous structures. The medial and lateral ligamentous complexes prevent valgus and posterolateral displacement, respectively, and their integrity is essential to avoid instability. The radial head is a secondary stabilizer, which has a most important role preventing medial instability when the medial collateral ligament is disrupted. The anterior band of the medial collateral ligament and the lateral ulnar collateral ligament are tight during the whole arc of motion and are important structures in preventing articular displacement. The lateral ligamentous complex is taut in supination and relaxes in pronation. Therefore, when the lateral ligaments have been disrupted during implantation of an unconstrained prostheses, the best position for immobilization to allow adequate healing of this structure is pronation. Additionally, the anterior capsule of the elbow joint, usually a very thin structure, may be thickened. In this group of patients one needs to be prepared to maintain the motion achieved during surgery with measures directed to avoid rescarring of the capsule (4).
EVALUATION
Clinical Assessment
Before seeing the patient, the therapist should obtain information concerning the general physical status of the patient and the level of activity prior to surgery to tailor the rehabilitation program to the individual capabilities and expectations. The function of the ipsilateral shoulder and wrist joints before the operation should be assessed, especially in the patient with rheumatoid arthritis in whom these joints may be involved. The status of the contralateral upper limb and the use of walking aids for lowerextremity pathology should also be investigated.
A thorough, detailed knowledge of the surgical technique, the type of implant used, complications encountered, and precautions prescribed by the treating surgeon are key to developing an effective rehabilitation program that will minimize impairment and maximize the patient’s functional ability. The therapist and the surgeon should maintain communication regarding the patient’s prognosis, treatment approach and guidelines, and progress.
Stability
The type of implant, linked or unlinked, is probably the single most important variable that influences the immediate postoperative regimen. The stability of unconstrained implants depends primarily on the integrity of the ligaments but may also be jeopardized by technical errors during prosthetic implantation or defects in the extensor mechanism. The therapist should know if an adequate reconstruction of the ligaments was achieved during surgery. The intraoperative range of motion after prosthetic implantation and the ligaments repaired should be recorded, and any tendency of the elbow to subluxate during passive range of motion, particularly in extension, should be noted and transmitted to the therapist. If the lateral collateral ligament has been released and repaired, it is necessary to unload it to allow adequate healing and avoid any disruption or elongation that may compromise stability. Therefore, the elbow of patients with unconstrained implants in whom the ligament has been released during surgery should be temporarily immobilized limiting full extension and supination (5,6).
The stability of semi-constrained implants is dependent on the loose hinge articulation between the ulnar and humeral components. The ligaments are routinely released during surgery, and no attempt at reconstruction is required (7). Postoperatively, the stability is not a concern and limiting motion to maintain stability is not necessary.
Management of the Triceps
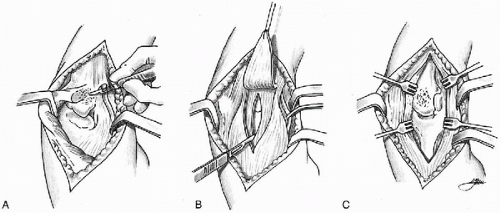
The surgical management of the triceps is an important factor that must be considered during the early rehabilitation program (Fig. 31-1). The surgical approaches that detach the triceps from its insertion, either by reflecting it to one side or by a split in the midline, require meticulous reattachment of the tendon through bone holes and protection of the repair postoperatively (8,9). Active extension of the elbow against gravity places stress on the repair and should be avoided during the first 3 to 4 weeks after surgery. When an approach that detaches the triceps is used,
only passive extension or gravity-assisted extension should be allowed. Some authors prefer an approach in which the triceps tendon is reflected from the muscle fibers as an inverted V and then the muscle fibers are released longitudinally (10). When this approach is used, the tendon is reattached to the muscle proximally allowing an V-Y plasty if flexion is limited intraoperatively. Healing of the musculotendinous junction is most important to achieve satisfactory muscle function, and the repair must be protected postoperatively to avoid disruption of the repair because this occasionally has been the cause of early posterior instability in unlinked implants (11,12). A period of 2 to 3 weeks of immobilization or controlled motion is required if this technique is used. Lastly, some arthroplasties may be implanted through an approach that preserves the triceps muscle and its attachment to the olecranon. This is the case in some posttraumatic situations or advanced rheumatoid elbows in which there is deficient distal humerus bone stock or the distal humerus is to be resected at the time of surgery. This approach works through the lateral and medial margins of the muscle (13, 14, 15). When this triceps-sparing approach is feasible, the postoperative regimen is greatly facilitated and active range of motion, including extension, can be initiated immediately after surgery.
only passive extension or gravity-assisted extension should be allowed. Some authors prefer an approach in which the triceps tendon is reflected from the muscle fibers as an inverted V and then the muscle fibers are released longitudinally (10). When this approach is used, the tendon is reattached to the muscle proximally allowing an V-Y plasty if flexion is limited intraoperatively. Healing of the musculotendinous junction is most important to achieve satisfactory muscle function, and the repair must be protected postoperatively to avoid disruption of the repair because this occasionally has been the cause of early posterior instability in unlinked implants (11,12). A period of 2 to 3 weeks of immobilization or controlled motion is required if this technique is used. Lastly, some arthroplasties may be implanted through an approach that preserves the triceps muscle and its attachment to the olecranon. This is the case in some posttraumatic situations or advanced rheumatoid elbows in which there is deficient distal humerus bone stock or the distal humerus is to be resected at the time of surgery. This approach works through the lateral and medial margins of the muscle (13, 14, 15). When this triceps-sparing approach is feasible, the postoperative regimen is greatly facilitated and active range of motion, including extension, can be initiated immediately after surgery.
REHABILITATION CONSIDERATIONS
Goals of Rehabilitation
The goals of rehabilitation after an elbow arthroplasty are to restore motion and strength, prevent complications of contracture and instability, and coordinate treatment of the involved tissues through the progressive stages of healing. Optimal rehabilitation requires careful timing and progression of therapy during the physiologic phases of tissue repair, balancing appropriate tissue stress to increase motion without provoking pain and inflammation (16). This requires the therapist to have a solid knowledge of the physiology of tissue healing and response to stress.
Patient Education
An informed patient is less likely to become anxious and will be more cooperative and involved in rehabilitation. Ideally, before the operation the therapist should give the patient an overview of the course of treatment and explain the importance of his or her efforts in reaching maximum potential. Preoperatively, the patient should be informed of the type of implant that is going to be used and its implications in the postoperative program. Additionally, the family setting of the patient and the facilities available to assist with home therapy should be investigated. Any concomitant pathology that may influence the therapy should be addressed with the patient before the operation. Detailed information of the limitations with the use of the arm during the early postoperative period should be given to the patient, and the therapy program should include a written outlined home program in addition to the therapy provided in the hospital. The patient should be aware of the meaning of passive, active-assisted, and active motion, and a basic knowledge about the use of splints is also desirable. All the time spent in the preoperative visit will result in higher benefit to the patient.
Pain and Edema Control
The rehabilitation starts at the time of surgery. If the inflammatory phase of healing can be minimized, more complete and rapid rehabilitation will be attained. Pain
can be a major limiting factor because it affects the patient’s effort and emotional well-being. The patient should be reassured that the pain is an expected part of the inflammatory response during the early phase of healing and should be encouraged to distinguish between tolerable discomfort and the type of pain that warns of impeding damage secondary to a complication of surgery.
can be a major limiting factor because it affects the patient’s effort and emotional well-being. The patient should be reassured that the pain is an expected part of the inflammatory response during the early phase of healing and should be encouraged to distinguish between tolerable discomfort and the type of pain that warns of impeding damage secondary to a complication of surgery.
The scheme represented by the mnemonic PRICEMM (protection, rest, ice, compression, elevation, medication, and modalities) is highly appropriate in the early postoperative period (17). Immobilization is recommended after an elbow replacement, but the type, optimal position, and duration of immobilization varies according to the implant design and the surgical approach. The aims of immobilization are to protect the healing structures, prevent injury, and maintain stability. Ice or cool packs are effective for reducing pain and edema and controlling hemorrhage and exudates in the inflammatory phase. The benefit of compression cryotherapy has been demonstrated in a prospective study in a group of patients using the Cryocuff (aircast), with significant reduction of postoperative pain, swelling, and blistering (17). Elevation may be the only edema control measure when a splint is in place. The patient should keep the elbow above the heart level whenever possible. When the patient is sleeping, the elbow is supported on pillows, and any discomfort secondary to shoulder pathology should be regularly checked.
The inflammatory process can also be controlled by pharmacologic methods. Nonsteroidal antiinflammatory medications may be used alone or in combination with narcotic drugs. Narcotic medications are rarely required for an extended period after elbow replacement, and whenever they are used, a strict control of the dose is recommended to avoid undesired side effects. When a continuous axillary brachial plexus catheter is placed postoperatively, the block should not be delivered until the patient is capable of cooperating with a neurologic examination to confirm the integrity of all three major nerves of the arm. In some instances, high-voltage galvanic stimulation has also proved helpful in controlling the inflammatory process by initiating involuntary muscle contractions that relieve edema (18). However, high-current intensity should be avoided when active or forceful muscle contraction is contraindicated, as when the triceps muscle has been disrupted or detached.
Exercise versus Pathology
Functional joint range of motion and flexibility must be restored within the healing parameters of the structures involved. Early protective motion has been shown to provide benefits such as improved collagen organization and decreased pain perception (19). However, when rehabilitating an elbow replacement, the therapist should use different protocols according to the type of implant and the surgical approach. The ideal scenario for the therapist is when the extensor mechanism has been preserved and postoperative instability is not a concern. In this setting, which only occurs when a semi-constrained implant has been used with a triceps-sparing approach, active range of motion in every plane can be started immediately. On the other extreme is the patient with a resurfacing implant in whom the lateral collateral ligament has been repaired and the approach has also disrupted the triceps tendon. Under these circumstances, both triceps insufficiency and postoperative instability are a concern, and the therapist must proceed cautiously with range of motion. In between these extremes is a spectrum of risk that makes fluent communication between the surgeon and the therapist essential.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree