Reconstruction for Missed Monteggia Lesion
Apurva S. Shah
Peter M. Waters
DEFINITION
Monteggia fracture-dislocations are rare complex traumatic upper limb injuries defined by fracture of the ulna associated with proximal radioulnar joint dissociation and radio-capitellar joint dislocation. These injuries typically affect patients between 4 and 10 years of age.19
The diagnosis of an acute Monteggia fracture-dislocation is often missed by skilled radiologists, emergency room physicians, pediatricians, and orthopaedic surgeons.4, 21
Late presentation of a previously undetected traumatic dislocation of the radial head occurs.
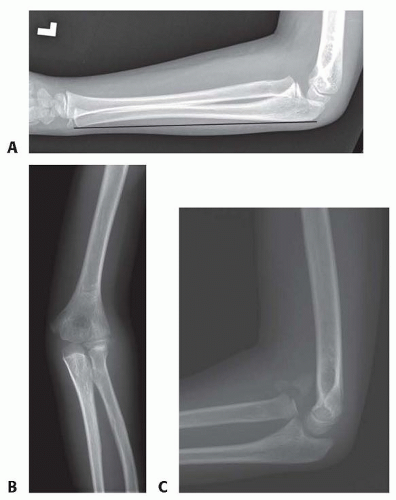
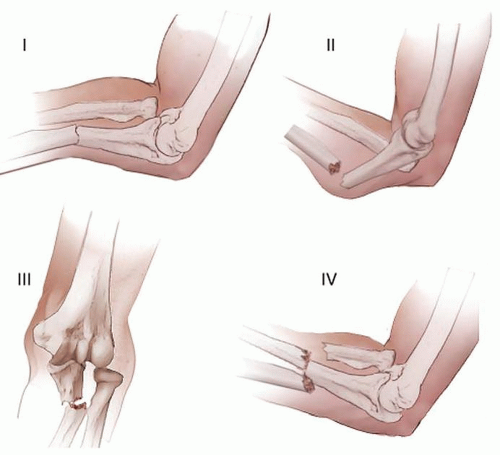
In children with a seemingly isolated dislocation of the radial head, scrutiny of forearm radiographs often demonstrates plastic deformation or fracture malunion of the ulna (FIG 1). The combination of these radiographic findings establishes the diagnosis of a chronic Monteggia fracture-dislocation or chronic Monteggia lesion, as opposed to a congenital dislocation of the radial head.4
Patients with chronic Monteggia lesions can present for evaluation at a variety of time points.21
In some children, radial head dislocation is first noted several weeks after initiating treatment for a misdiagnosed, isolated ulnar fracture.
In other patients, the diagnosis may not be established for months to years following injury due to the development of pain, loss of motion, and/or valgus malalignment.
Even a few weeks after injury, treatment of a Monteggia lesion is much more complicated than acute recognition and treatment.21
Nonetheless, due to pain, restriction of motion, and functional disability, most patients with chronic Monteggia lesions are offered surgical correction.
ANATOMY
Understanding the anatomy of the radiocapitellar joint and proximal radioulnar joint is crucial for understanding safe and appropriate treatment of chronic Monteggia lesions.
The bony architecture, joint contour, and periarticular ligaments all contribute to stability of radial head and congruity of the radiocapitellar and proximal radioulnar joints.
The radial head exhibits an asymmetric cylindrical shape with a concavity in the midportion to accommodate its articulation with the convex capitellum.
The radial head also articulates with the lesser sigmoid or radial notch of the proximal ulna. This complex pair of articulations permits forearm rotation in addition to elbow flexion and extension.
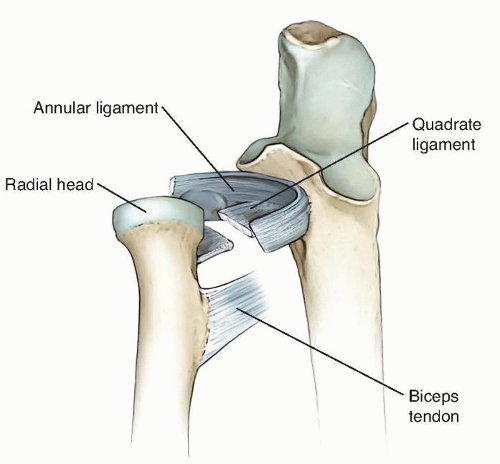
The annular ligament is the principal stabilizer of the radial head during forearm rotation. The annular ligament originates on the anterior margin of the lesser sigmoid notch of the proximal ulna and encircles the radial neck before inserting on or adjacent to the posterior margin of the lesser sigmoid notch (FIG 2).16
The annular ligament occupies 80% of the fibro-osseous ring.16
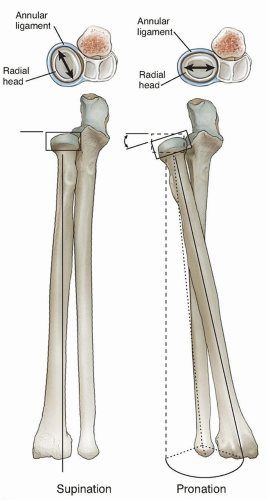
The annular ligament is one component of the Y-shaped lateral ligamentous complex and maintains the radial head in contact with the ulna at the proximal radioulnar joint (FIG 3).
Because the radial head is not perfectly cylindrical, the annular ligament has been found to tighten anteriorly in forearm supination and posteriorly in forearm pronation.16
The quadrate ligament lies just distal to the annular ligament and connects the proximal ulna and the radial neck (see FIG 2).
The anterior portion of the quadrate ligament is stronger and denser than the posterior portion, whereas the central portion is relatively thin.
The anterior portion stabilizes the proximal radioulnar joint in maximum supination and the weaker posterior portion stabilizes the joint in maximum pronation.24
The oblique cord is a small, inconsistent fibrous bundle that originates from the lateral side of the ulna just distal to the lesser sigmoid notch and inserts just distal to the bicipital tuberosity of the radius.27 The oblique cord progressively tightens in supination and also stabilizes the proximal radioulnar joint. This structure is not thought to be clinically relevant.27
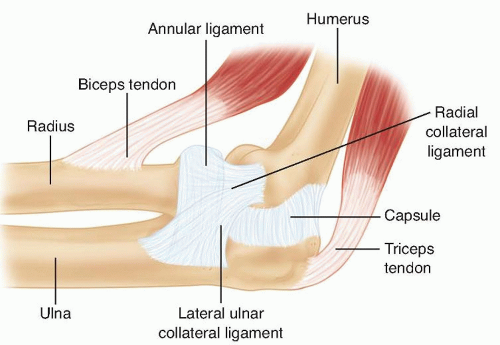
FIG 3 • The Y-shaped lateral ligamentous complex of the elbow consists of the radial collateral ligament, the lateral ulnar collateral ligament, and the annular ligament.
The radial head is most stable with the forearm in a position of supination.24 Although the bony architecture provides little inherent stability to the proximal radioulnar joint, the elliptical shape of the radial head contributes to ligament function. In forearm supination, the long axis of the radial head is perpendicular to the lesser sigmoid notch, causing the annular ligament and the anterior segment of the quadrate ligament to tighten (FIG 4).
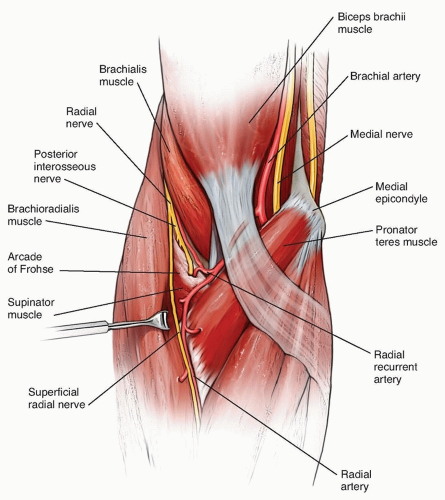
The posterior interosseous nerve passes under the arcade of Frohse and through the supinator (FIG 5). The proximity of
the posterior interosseous nerve to the radial head and neck makes the nerve susceptible to injury during reconstruction of a chronic Monteggia lesion. The posterior interosseous nerve is often adherent to a chronically dislocated radial head/neck and rarely can be entrapped in the radiocapitellar joint.21 Identification of the nerve during the reconstruction is critical for avoidance of iatrogenic injury.
PATHOGENESIS
There are multiple patterns of Monteggia fracture-dislocations in children.
Bado’s original classification of Monteggia lesions is well recognized and had undergone minimal modification other than the description of various Monteggia equivalent lesions (FIG 6).1 The scheme is based on the direction of the radial head dislocation and ulnar fracture angulation.
Bado type I lesions represent anterior dislocations of the radial head associated with an apex anterior ulnar diaphyseal fracture or plastic deformation. This pattern is the most common in children and represents approximately 70% to 75% of all injuries.19
Type I lesions can occur secondary to direct blow, hyperpronation, or hyperextension.
The most common mechanism is fall on an outstretched hand that forces the elbow into maximal extension with the forearm in relative pronation.26 Due to the laxity of
the annular and quadrate ligaments in pronation, the stability of the radial head is tenuous and the anterior bending force combined with reflexive contraction of the biceps brachii results in anterior dislocation of the radial head. Due to the continued bending moment, the ulna undergoes plastic deformation or tension failure of the anterior cortex.
Bado type II lesions are characterized by posterior or posterolateral dislocation of the radial ahead associated with a posterior ulnar diaphyseal or metaphyseal fracture. This is the most common pattern in adults but represents approximately 5% of Monteggia lesions in children.19
Bado type III lesions demonstrate lateral dislocation of the radial head and are associated with an apex lateral (varus) fracture of the proximal ulna. This is the second most common Monteggia lesion in children and represents nearly 30% of all pediatric injuries.19
Bado type IV lesions are characterized by anterior dislocation of the radial head and fractures of both the radius and ulna. Type IV lesions are rare in children.
The initial diagnosis of a Monteggia fracture-dislocation is often missed by qualified physicians.4, 21 Because the ulna heals rapidly in children, a chronic Monteggia lesion can develop over a period of 3 to 4 weeks. Due to the frequency of Bado type I lesions, most chronic Monteggia lesions in children are characterized by anterior dislocation of the radial head and apex anterior ulnar fracture malunion or plastic deformation.13, 21
Suboptimal treatment of the ulnar fracture in an acute Monteggia lesion can also result in unrecognized or late subluxation or dislocation of the radial head, resulting in a chronic Monteggia lesion.19
In general, only plastic and greenstick ulnar fractures should be treated with closed reduction and casting. All complete fractures should be treated surgically to avoid late instability.20
Transverse or short oblique ulnar fractures should be treated with intramedullary pin fixation and long oblique or comminuted fractures should be treated with open reduction and plate fixation.20
Always obtain dedicated elbow radiographs to evaluate congruency of the radiocapitellar reduction following reduction of the ulnar fracture.
Chronic Monteggia lesions can result in substantial loss of function and are far more complex than acute injuries in terms of surgical decision making and management.21
NATURAL HISTORY
Initial reports on chronic Monteggia fracture-dislocations suggested that the natural history of the untreated lesion was not problematic. In these reports, results from late surgical reconstruction were complicated by scarring, arthrosis, and loss of motion. For these reasons, the classic treatment was neglect and radial head excision at skeletal maturity if necessary.
More recent data suggests that most chronic Monteggia lesions are not tolerated well over time.6, 21 Patients can develop pain, arthrosis and loss of motion, functional impairment, progressive cubitus valgus, and late neuropathy even if initial symptoms are mild.2, 6, 21 Loss of elbow flexion and forearm pronation can occur.21 The best treatment for this problem remains preventative.
PATIENT HISTORY AND PHYSICAL FINDINGS
Most patients presenting with a chronic Monteggia lesion note a distinct history of trauma. The traumatic episode often involves significant force and is frequently characterized by a fall on to an outstretched hand with the elbow in extension and the forearm in pronation.
A history of trauma aids in distinguishing a traumatic radial head dislocation form a congenital radial head dislocation.
A history of acute elbow pain and temporary loss of motion in a child younger than 4 years of age secondary to minor trauma should prompt consideration of radial head subluxation or nursemaid’s elbow. Radiographs will reveal an aligned radial head and no ulnar fracture or deformity. Children with a nursemaid’s elbow usually have prompt resolution of discomfort and restoration of movement following closed reduction maneuvers.
The timing of the injury and nature of prior medical treatment should be clarified. Patients presenting within 2 weeks of injury may still be candidates for standard treatment strategies for acute Monteggia fracture-dislocations.
Physical examination may reveal cubitus valgus as well as loss of forearm rotation and elbow flexion. Nerve functional testing should be performed.
On inspection, anterior fullness in the cubital fossa may be detected. This corresponds to a palpable anterior dislocation of the radial head. The dislocated radiocapitellar joint should be palpated during forearm rotation to detect crepitation or other signs of elbow arthrosis.
The elbow carrying angle should be evaluated. The carrying angle in normal children increases with age and averages 9.3 degrees in males and 11.5 degrees in females.7 Patients with chronic Monteggia lesions frequently demonstrate cubitus valgus and can present with carrying angles that exceed 30 degrees.21 For some patients and families, this represents a significant aesthetic concern.
Elbow motion and forearm rotation should be precisely assessed. Normal elbow motion varies by child and averages 4 degrees of hyperextension to 145 degrees of flexion.7 Loss of elbow motion is common, particularly in chronic Bado type I Monteggia lesions where anterior dislocation of radial head results in abutment against the humerus.21 Elbow flexion is limited in the majority of patients with chronic Bado type I lesions and averages 110 degrees.13 Terminal elbow flexion may be associated with visible discomfort. Loss of forearm rotation, particularly pronation, is also common.21 Many children with chronic Monteggia lesions demonstrate compensatory radiocarpal and midcarpal rotation which can obscure assessment of true forearm rotation. In order to careful track true forearm rotation, the examiner must assess rotation of the radial styloid relative to the axis of the ulna.
A detailed neurologic examination should be performed to assess peripheral nerve function, including the ulnar nerve, median nerve, and posterior interosseous nerve (see Exam Table at the end of the book). Sensibility can be assessed subjectively with light touch or objectively with two-point discrimination in a cooperative child older than 5 years of age. Hand and wrist strength is tested.
In tardy ulnar nerve palsy, patients may demonstrate diminished sensibility at the volar pad of the small finger (autonomous zone). Patients may also present with intrinsic muscle atrophy, clawing of the small finger and ring finger, diminished digital abduction strength, a positive Froment sign, or a positive Wartenberg sign.3
Patients with a tardy posterior interosseous nerve palsy will demonstrate weakness with finger metacarpophalangeal joint extension and thumb retropulsion.11 Because the extensor carpi radialis longus is innervated by the radial nerve, patients may demonstrate preserved wrist extension with a tendency toward radial deviation. Sensation at the first dorsal web space is typically normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree