Radiologic Diagnosis
Garry Gold
Vijay Chandnani
Donald Resnick
The term osteoarthritis (OA), previously called degenerative joint disease, is applied to a variety of distinct processes affecting joints in extraspinal and spinal locations. There are basic differences in the anatomy of the various types of joints at these sites, and they change in unique fashions. Each type of articular degeneration is associated with characteristic clinical, pathologic, and radiologic features. This chapter discusses the radiologic manifestations of OA at extraspinal joints as well as in the various types of spinal articulations. Methods of quantitation of radiologic changes are also discussed.
Osteoarthritis of Extraspinal Locations
General Considerations
OA, the most frequent articular affliction, was not regarded as a distinct entity until the early twentieth century, when it was clearly differentiated from rheumatoid arthritis.1,2 OA is the best general phrase to describe degenerative alterations in any type of joint. These alterations may appear in fibrous, cartilaginous, or synovial articulations. The pathologic and radiographic appearances vary from one location to another, but at any site, the abnormalities appear to be related to degeneration of specific articular structures. The terms osteoarthrosis and OA are reserved for OA of synovial joints. Although inflammatory changes are not pronounced in most of these joints, OA is the term used in this chapter because this designation is widely accepted in the United States. Furthermore, in those joints in which significant synovial inflammatory abnormalities do accompany OA, such as in the interphalangeal articulations of middle-aged and elderly women, OA is the more accurate description of the disorder.
Primary and Secondary Osteoarthritis
OA has traditionally been classified into primary (idiopathic) and secondary types. Primary OA has been regarded as a process in which articular degeneration occurs in the absence of any obvious underlying abnormality, whereas secondary OA has been regarded as articular degeneration that is produced by alterations from a preexisting condition. This classification is misleading, because careful evaluation of many examples of “primary” OA will reveal some mechanical deviation in the involved articulation that has led to secondary degeneration of the joint. Examples include infantile and childhood disorders such as congenital dysplasia and a slipped capital femoral epiphysis; when mild, these are easily overlooked, yet later they can lead to OA in the hip. Thus, it appears likely that primary OA does not truly exist, and the use of such a designation seems only to underscore current diagnostic limitations.
Articular degeneration may result from either an abnormal concentration of force across an articulation with normal articular cartilage matrix or a normal concentration of force across an abnormal joint.3 Eventually, abnormalities of force and articular structure appear together (Table 8-1). This classification emphasizes that there are many potential causes of secondary OA and that these causes may lead to articular degeneration by increasing the amount of stress on cartilaginous and osseous structures or by directly affecting the cartilage or subchondral bone itself. These considerations have relevance to radiologic interpretation of degenerative changes in joints.
Radiographic-Pathologic Correlation
Degenerative changes are found not only in the stressed (pressure) areas of a joint but also in the nonstressed (nonpressure) segments.4 Therefore, either excessive or
diminished pressure appears to be deleterious to cartilage. Normally, cartilage derives its nutrition from intermittent intrusion and extrusion of synovial fluid during alternating periods of pressure and rest as well as from vessels in the subchondral bone, which allow material to pass into the basal layer of cartilage.5,6,7,8 Both sources of nutrition become defective in the presence of excessive or diminished stress, leading to degenerative changes.
diminished pressure appears to be deleterious to cartilage. Normally, cartilage derives its nutrition from intermittent intrusion and extrusion of synovial fluid during alternating periods of pressure and rest as well as from vessels in the subchondral bone, which allow material to pass into the basal layer of cartilage.5,6,7,8 Both sources of nutrition become defective in the presence of excessive or diminished stress, leading to degenerative changes.
TABLE 8-1 CLASSIFICATION OF OA | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In the stressed segment, pathologically evident thinning and denudation of the cartilaginous surface and vascular invasion, in addition to infarction and necrosis of the subchondral trabeculae, account for joint space loss, bone sclerosis, and cyst formation that are apparent on the radiographs (Table 8-2). In the nonstressed segment, pathologically evident hypervascularity of marrow and cartilage leads to radiographically detectable osteophytosis.4
Cartilage in degenerating joints at first appears discolored, thinned, and roughened; later, crevices, ulcerations, and larger areas of erosion become evident.9,10,11 This progressive cartilage loss accounts for one of the fundamental radiographic signs of OA, loss of joint space. This diminution is characteristically located mainly in the area that has been subjected to the greatest pressure, such as the superolateral aspect of an osteoarthritic hip and the medial femorotibial space of an osteoarthritic knee. This focal cartilaginous destruction and resulting loss of the interosseous space allow differentiation from processes such as rheumatoid arthritis that lead to diffuse chondral alterations. Certain sites of involvement are exceptions to this rule; in OA of the interphalangeal or metacarpophalangeal joints of the hands as well as of the sacroiliac joint, diffuse joint space involvement may be noted.
After cartilage loss, bone eburnation becomes evident in the closely applied osseous surfaces, apparently related to deposition of new bone on preexisting trabeculae and to trabecular compression and fracture with callus formation.12,13,14,15,16,17,18 In general, radiographic evidence of joint space loss is present before eburnation becomes apparent. After progressive loss of joint space, sclerosis becomes more apparent, extending vertically into deeper regions of the subchondral bone and horizontally into adjacent osseous segments. The radiodense area may initially appear uniform, but radiolucent areas of varying size eventually appear, reflecting subchondral cyst formation.
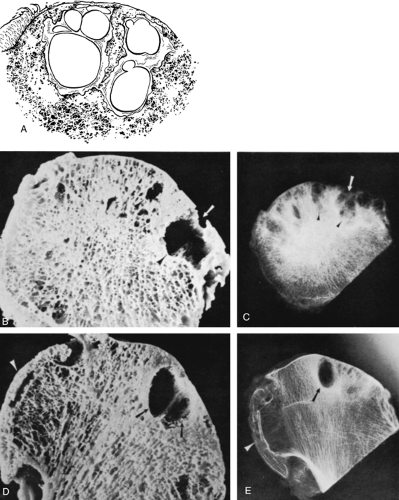
Cyst formation is an important finding in OA 19,20,21 (Fig. 8-1); these lesions have been variously termed synovial cysts,22 subchondral cysts,8 subarticular pseudocysts,23 necrotic pseudocysts,24 and geodes.25 Within the stressed segment of the subchondral bone in OA, cystic spaces appear between thickened trabeculae. These cysts are commonly multiple, of varying size (approximately 2 to 20 mm in diameter), and piriform. Communication with the articular space may or may not be identifiable.26 The cysts seen radiographically in OA characteristically have a sclerotic margin.
Osteophytes (Table 8-3) develop in areas of a degenerating joint that are subjected to low stress; they may be marginal (peripheral), although they may become apparent at other articular locations as well. Osteophytes typically arise as a revitalization or reparative response by remaining cartilage, but they may also develop from periosteal or synovial tissue.27 The features of conversion of cartilage to bone in OA resemble those accompanying normal endochondral (enchondral) ossification. Marginal osteophytes appear radiographically as lips of new bone around the edges of the joint and are of variable size. The excrescences frequently predominate in one side of the joint, develop initially in areas of relatively normal joint space, and are usually unassociated with significant adjacent sclerosis or cyst formation (Fig. 8-2). Osteophytes may also appear in the central portions of a joint in which remnants of articular cartilage still exist.27 The hypervascularity of the subchondral bone stimulates endochondral ossification, and the resulting excrescences are often demarcated at their bases by remnants of the original calcified cartilage. Central osteophytes frequently lead to a bumpy articular contour on the radiograph. In certain joints, bone may develop
from cartilaginous stimulation by the periosteum or synovial membrane. This phenomenon, termed buttressing,28,29 is most characteristic in the medial portion of the femoral neck. On radiographs, a radiodense line of variable thickness extends along part or all of the femoral neck.
from cartilaginous stimulation by the periosteum or synovial membrane. This phenomenon, termed buttressing,28,29 is most characteristic in the medial portion of the femoral neck. On radiographs, a radiodense line of variable thickness extends along part or all of the femoral neck.
TABLE 8-2 OA OF SYNOVIAL ARTICULATIONS (OSTEOARTHRITIS): RADIOGRAPHIC-PATHOLOGIC CORRELATION | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
TABLE 8-3 TYPES OF OSTEOPHYTES | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
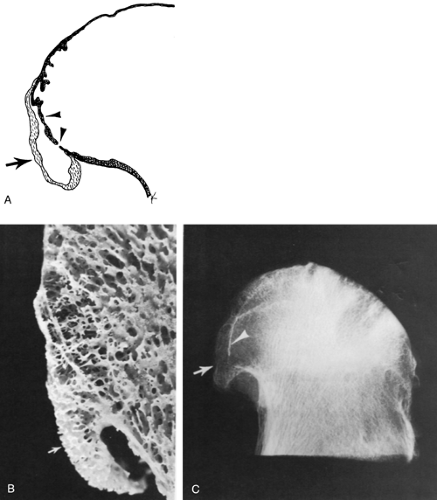
OA may be associated with degeneration of other articular structures, such as the fibrocartilage labrum, disks, and menisci.30,31,32 Degeneration of tendons, intraosseous ligaments, and membranes is also common, especially near the sites of attachment of these structures to bone (Fig. 8-3).
These may manifest radiographically as excrescences that are termed enthesophytes. Tendon and ligament calcification may also be noted.
These may manifest radiographically as excrescences that are termed enthesophytes. Tendon and ligament calcification may also be noted.
Osteoarthritis in Specific Locations
Hand and Wrist
OA of the proximal and distal interphalangeal joints of the hand (including the interphalangeal joint of the thumb) is extremely common, especially in middle-aged, postmenopausal women. Involvement of multiple digits of both hands is characteristic. Clinically, the altered digits may reveal malalignment, such as flexion deformity and radial or ulnar deviation at the interphalangeal joints. Bone outgrowths at the distal interphalangeal joints are termed Heberden nodes.33 Similar outgrowths at the proximal interphalangeal joints are termed Bouchard nodes.
Distal interphalangeal and proximal interphalangeal joints are frequently affected simultaneously and symmetrically; however, extensive alterations at distal interphalangeal joints may occur in the absence of proximal interphalangeal joint abnormalities, and less commonly, isolated abnormalities of proximal interphalangeal joints may be evident.
Radiographs reveal prominent osteophytes and joint space narrowing, providing close apposition of adjacent enlarged osseous surfaces. It is the closely applied, undulating articular surfaces that produce the diagnostic radiographic appearance of the disease, allowing it to be distinguished from erosive disorders, which produce separation of the involved bones. In OA, the wavy contour of the base of the distal phalanx resembles the wings of a bird (i.e., the “seagull” sign) (Fig. 8-4). The involved digits frequently reveal mild to moderate radial and ulnar subluxation at distal interphalangeal or proximal interphalangeal joints, producing a zigzag contour. At the margins of the affected joint, focal radiodense lesions (ossicles) are apparent overlying the joint capsule; they resemble intra-articular osseous bodies or fractured osteophytes.
Metacarpophalangeal joint involvement in OA is almost invariably associated with more prominent abnormalities at the proximal and distal interphalangeal joints. Uniform narrowing of one or more metacarpophalangeal interosseous spaces is most characteristic,34 and cystic lesions and osteophytes may also be apparent. Erosions are absent. One exception to these findings occurs in the first digit, in which isolated alterations at the first metacarpophalangeal joint can be a prominent manifestation of OA.
The radial distribution of OA of the wrist is well known. In the absence of significant accidental or occupational trauma, changes are usually confined to the trapeziometacarpal joint and trapezioscaphoid space of the midcarpal joint. At the
trapeziometacarpal joint, radiographic features of OA are characteristic. Radial subluxation of the metacarpal base, narrowing of the interosseous space, sclerosis, cystic changes in the subchondral bone, osteophytosis, and bone fragmentation become apparent (Fig. 8-5). OA of the trapezioscaphoid space is usually combined with degenerative changes at the trapeziometacarpal joint,35 although isolated abnormalities have also been reported.36,37,36 Typical radiographic features at this location are apparent in a unilateral or bilateral distribution; these include joint space narrowing and sclerosis of apposing surfaces of the trapezium, trapezoid, and scaphoid.
trapeziometacarpal joint, radiographic features of OA are characteristic. Radial subluxation of the metacarpal base, narrowing of the interosseous space, sclerosis, cystic changes in the subchondral bone, osteophytosis, and bone fragmentation become apparent (Fig. 8-5). OA of the trapezioscaphoid space is usually combined with degenerative changes at the trapeziometacarpal joint,35 although isolated abnormalities have also been reported.36,37,36 Typical radiographic features at this location are apparent in a unilateral or bilateral distribution; these include joint space narrowing and sclerosis of apposing surfaces of the trapezium, trapezoid, and scaphoid.
 Figure 8-5 Osteoarthritis of the trapeziometacarpal joint. Joint space loss, subchondral sclerosis and cysts, and osteophytes are present at the trapeziometacarpal joint (arrow). |
OA localized to other compartments of the wrist is distinctly unusual in the absence of a history of trauma. However, fracture, subluxation, dislocation, or osteonecrosis about the wrist can lead to altered joint motion and can result in secondary OA. Typical examples include OA of the radiocarpal and midcarpal compartments after scaphoid injuries,39,40 OA of the radiocarpal and inferior radioulnar compartment after osteonecrosis of the lunate (Kienböck disease), and OA of the inferior radioulnar compartment after subluxation of the distal part of the ulna. Arthrosis of the lunate-capitate space, leading to interosseous narrowing, sclerosis, and cyst formation, has been emphasized as an additional post-traumatic degenerative condition.41 This abnormality is usually combined with scapholunate separation, or dissociation, and narrowing of the radioscaphoid space.42 The resulting radiographic changes are termed the scapholunate advanced collapse pattern, or SLAC, wrist.42,43
Shoulder, Elbow, and Acromioclavicular Joints
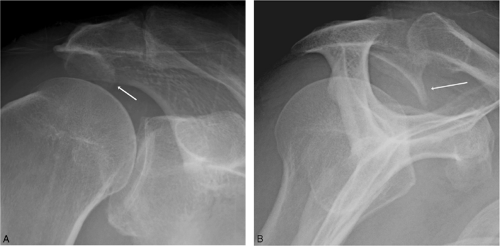
OA of the glenohumeral joint has been considered unusual in the absence of trauma. Nontraumatic degenerative changes at this location are usually secondary to other disorders, such as alkaptonuria, acromegaly, epiphyseal dysplasia, calcium pyrophosphate dihydrate (CPPD), crystal deposition disease, apatite deposition disease (Milwaukee shoulder)44, and hemophilia.45,46,47 The most frequent abnormality in OA at this site is osteophyte formation along the articular margin of the humeral head and the line of attachment of the labrum to the glenoid fossa. These osteophytes predominate along the anteroinferior portions of the joint. Another abnormality seen in OA of the glenohumeral joint is eburnation, manifested as subchondral sclerosis, along the superior and middle portion of the articular surface of the humeral head (Fig. 8-6). Other alterations seen at this location include osseous excrescences with occasional areas of cystic change in the anatomic neck of the humerus. Osteophytes are commonly evident in and around the bicipital groove as well.48
OA of the elbow is uncommon and usually follows accidental or occupational trauma, as seen in miners and drillers. Typical radiographic findings include joint space narrowing, sclerosis, cysts, and osteophytes. Olecranon enthesophytes at the ulnar attachment of the triceps tendon may accompany these alterations (Fig. 8-3).
Degenerative changes of the acromioclavicular joint are nearly universal in the elderly. Radiographic examination reveals joint space loss, sclerosis of apposing osseous surfaces, marginal osteophytes, hypertrophy and inferior subluxation of the acromial end of the clavicle, and osseous proliferation on either the superior or inferior surface of the acromion49,50 (Fig. 8-7).
Hip
OA of the hip is invariably associated with progressive and focal joint space narrowing. With the onset of this narrowing, the femoral head moves toward the acetabulum.
Three basic patterns of migration can be observed: superior migration, medial migration, and axial migration. With superior migration, the femoral head moves in an upward or superior direction with respect to the acetabulum. A medial migration pattern is evident when joint space loss is confined to the inner third of the joint. With axial migration, the femoral head migrates axially along the axis of the femoral neck, and there is diffuse loss of articular space. This classification system relies on changes seen on the frontal radiograph. Anterior or posterior migrations of the femoral head, as seen on lateral radiographs or with computed tomography or magnetic resonance imaging (MRI), may accompany these changes.
Three basic patterns of migration can be observed: superior migration, medial migration, and axial migration. With superior migration, the femoral head moves in an upward or superior direction with respect to the acetabulum. A medial migration pattern is evident when joint space loss is confined to the inner third of the joint. With axial migration, the femoral head migrates axially along the axis of the femoral neck, and there is diffuse loss of articular space. This classification system relies on changes seen on the frontal radiograph. Anterior or posterior migrations of the femoral head, as seen on lateral radiographs or with computed tomography or magnetic resonance imaging (MRI), may accompany these changes.
Although the pattern of movement of the femoral head with respect to the acetabulum may be variable in OA, thereby influencing the distribution of morphologic changes, the basic radiographic and pathologic changes are similar. These include joint space narrowing, osteophytosis, buttressing, sclerosis, and cyst formation21,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67 (Fig. 8-8). The cysts can be single or multiple and are of varying size; they are located on either the femoral or the acetabular side of the joint, or both. Large cystic lesions in the acetabulum are occasionally seen.
Synovial membrane alterations in OA are generally mild, although considerable osseous and cartilaginous debris may become embedded in the synovium of osteoarthritic hips, particularly in the recesses associated with the capsular reflection on the femoral neck.28 Hypertrophied synovium containing detritus may become prominent in these areas.65
Arthrography is occasionally used to outline the location and extent of cartilage loss in OA of the hip,68 although similar abnormalities may be detected on routine radiography. Arteriography has been used to elucidate the vascular abnormalities of OA of the hip,69,70 which are manifested as increased number, length, and width of periarticular and intraosseous vessels. Venography may be used to identify a deviation in the normal pattern of venous drainage from the femoral head and neck.71,72,73,74 In OA, increased flow
initially occurs by way of the femoral shaft; subsequently, pooling of injected contrast material with decreased or absent venous outflow is seen. Radionuclide examination demonstrates increased uptake in periarticular osseous tissue.75,76 The scintigraphic pattern may be more sensitive, although relatively nonspecific, in detecting the presence and extent of OA. Computed tomography in conjunction with arthrography may be useful in detecting osteocartilaginous debris and in delineating the extent of anteversion of the femoral neck.77,78,79 MR imaging or MR arthrography may demonstrate areas of cartilage thinning, tears of the acetabular labrum, increased bone marrow signal on long TE pulse sequences indicative of reactive edema, and presence of intra-articular osteochondral loose bodies.80,81,82,83
initially occurs by way of the femoral shaft; subsequently, pooling of injected contrast material with decreased or absent venous outflow is seen. Radionuclide examination demonstrates increased uptake in periarticular osseous tissue.75,76 The scintigraphic pattern may be more sensitive, although relatively nonspecific, in detecting the presence and extent of OA. Computed tomography in conjunction with arthrography may be useful in detecting osteocartilaginous debris and in delineating the extent of anteversion of the femoral neck.77,78,79 MR imaging or MR arthrography may demonstrate areas of cartilage thinning, tears of the acetabular labrum, increased bone marrow signal on long TE pulse sequences indicative of reactive edema, and presence of intra-articular osteochondral loose bodies.80,81,82,83
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree