Quantifying Dysfunction in Whiplash Injury: Old Questions, New Methods
James M. Elliott
David M. Walton
It is currently estimated that approximately 50% of people who report neck pain or related symptoms (“Whiplash-Associated Disorder,” WAD) following a motor vehicle collision (MVC) will continue to experience persistent symptoms 12 months later [9, 91], with 20-25% experiencing significant long-term interference in daily activities [20, 73, 74, 75]. The signs and symptoms of persistent WAD vary from inconsistent to mystifying, running the gamut from localized neck tenderness or stiffness to cognitive and balance disorders with or without widespread sensory hyperalgesia [74, 76, 77, 78]. Despite the continued engineering advancements in the manufacturing of safer cars with improved seat designs aimed at preventing injury or death, the incidence of chronic or persistent WAD does not appear to be waning [81].
Adding to the complexity of the condition are inconsistent associations between subjective complaints and objective findings on traditional diagnostic imaging [15, 79]. Further, there has yet to be convincing empirical evidence that any form of active intervention is effective at improving the rates of recovery [36, 41, 50]. Several systematic reviews have concluded that the mechanisms of the event itself (e.g., direction of impact, speed of impact, awareness of collision) have little effect on the posttraumatic trajectory [88], while exaggerated negative affect appears to be one of the most consistent predictors of a poor outcome [7, 8]. The confluence of such findings has led to exploratory
investigations centered on the key biopsychosocial factors that may drive the clinical course for some patients with WAD [17].
investigations centered on the key biopsychosocial factors that may drive the clinical course for some patients with WAD [17].
While the current literature in the field is offering promising new directions for understanding the etiology of this complex condition, much of it is being conducted in isolation or on one or few pathways, with few notable exceptions [38, 61, 83]. Although diverse, these advancements are offering potential points of interprofessional convergence that could be harnessed and applied practically toward knowledge transfer. This chapter presents an integrated perspective of WAD from biological, psychological, and social sciences that are intended to highlight potential points of convergence. By doing so, the intention is to highlight the complexities of the condition and propel whiplash research and treatment into a new era of understanding.
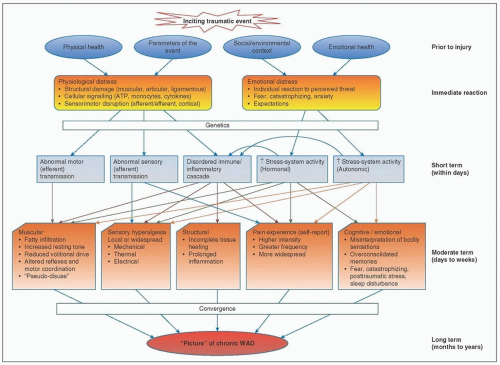
The broad spectrum of WAD signs and symptoms, including pain, sensory hypersensitivity, balance and neuromotor deficits [29], cognitive interference [3], and mood disorders [72], among others, suggests a multifactorial etiology. Foundational models to explain the genesis and maintenance of chronic posttraumatic pain (broadly) or WAD (specifically) range from purely cognitive [52] to purely biological [85], with recent attempts to integrate evidence from different fields [47]. A new adapted model is described in Fig. 6-1, describing the inciting event as a “trauma” that occurs within the premorbid biological (genetic, personal factors) and socio-environmental (medicolegal environment, support systems) context of the individual. Drawing from well-established models of stress and homeostasis [10, 42], the new model recognizes the experience of trauma and injury, whether physiological, psychological, or both, as a natural stressor to the organism that necessarily elicits activity in stress-response systems. The magnitude of the response is mediated by the magnitude or type of tissue injury, the genetic profile or physical habitus of the injured individual, peritraumatic emotional status, learned cognitions or coping strategies
from a lifetime of experience, or even the responses from other important individuals such as family members, clinicians, attorneys, insurers, and others.
from a lifetime of experience, or even the responses from other important individuals such as family members, clinicians, attorneys, insurers, and others.
The terms are chosen intentionally to avoid judgment regarding the “correctness” of the stress response. Rather than choosing judgment labels such as “exaggerated” or “avoidant,” the model describes such responses as adaptive or maladaptive, which demands consideration of the individual context; not all responses can be considered universally good or universally bad for all people. Consistent with previous models, two pathways are then proposed, one favorable and the other unfavorable. Even this may be an oversimplification, as human outcomes can rarely be dichotomized as clearly good or clearly bad, but it serves the purposes of this foundational discussion.
To understand the pathway from trauma to recovery, it is prudent to first consider the outcome of, and definition for, recovery. There has yet to be consensus on the correct operationalization of recovery after traumatic injury. We feel a reasonable definition of recovery could include a satisfying end to the injury experience with the individual resuming, with little restriction, their preinjury life trajectory, including participation in valued roles and future goals [89]. This conceptualizes the experience of injury as necessitating a short-term deviation from life trajectory, but allows resolution of the dysfunction or, in some cases, redefinition or readjustment to a new satisfactory health status with or without medical/rehabilitative management.
We believe this is most likely to be the case when tissue damage is limited to contractile (e.g., muscle) or noncontractile (e.g., tendon or ligament) “soft tissue” with a stress response that is adaptive given the context. In this case, physiological or psychological processes, regardless of initial pain intensity, facilitate the restoration of relative allostasis (realignment with pretrauma status) through mobilization of key immune/inflammatory, endocrine, neural, and psychobehavioral resources, as will be described below. Notably, the sensorimotor system is
largely spared in this pathway, in contrast to the unfavorable pathways described below. The coordinated adaptive efforts of stress-response pathways facilitate soft-tissue repair, encourage appropriate behavioral coping strategies, and provide a sound environment for a satisfactory outcome in a reasonable time frame.
largely spared in this pathway, in contrast to the unfavorable pathways described below. The coordinated adaptive efforts of stress-response pathways facilitate soft-tissue repair, encourage appropriate behavioral coping strategies, and provide a sound environment for a satisfactory outcome in a reasonable time frame.
In this model, an unfavorable pathway can arise from damage affecting the peripheral and/or central nervous system (sensorimotor) in isolation from or in tandem with maladaptive stress- system activity. For purposes of clarity, these pathways are described as separate but parallel, although it is more likely that a bidirectional causal relationship exists between sensorimotor and stress dysregulation, where activity in one influences activity in the other. Accordingly, each will be described in turn.
Sensorimotor
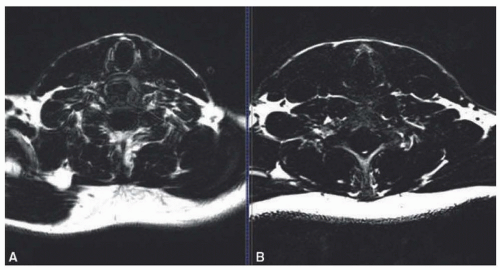
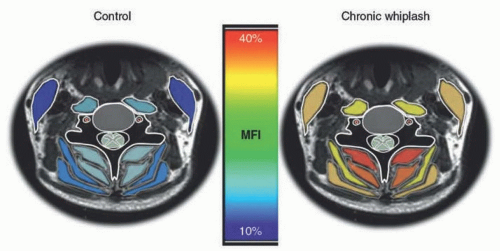
Conceptually, the spinal cord is subject to the same mechanical forces as other spinal structures, yet it is one of the least elastic tissues in the region [16]. It is thus plausible that mild damage involving the ascending or descending white matter tracts of the cervical cord occurs during high-energy transfer of motion through the head and neck as occurs during MVC, leading to subclinical impairments in sensory and/or motor pathway signaling. Damage affecting the sensorimotor pathways may explain many of the signs and symptoms recently identified as part of the complex picture of chronic WAD, including thermal or mechanical local hyperalgesia [76] and widespread pain or hypersensitivity [67]. Damage to the motor pathways may represent a candidate lesion for explaining recent findings of muscle fatty infiltration in the neck (Figs. 6-2A, B and 6-3) [19, 20, 21, 23] or other muscles of subjects with chronic WAD (Fig. 6-4A-C) [22]. Such interference would also impair feed-forward activation (slowed time-to-activation) of the deep cervical flexors, which appears to be a consistent feature of chronic neck pain [27].
Preliminary evidence from our Chicago laboratory supports involvement of the cervical spinal cord in a subset of the population with severe chronic WAD symptoms [22]. Similar to other evidence involving patients with cervical myelopathy [34], spondylosis [65],
and spinal cord injury [14], we have identified a subset of people with severe chronic symptoms that show signs of subclinical spinal cord damage using magnetic resonance spectroscopy [24] and magnetization transfer imaging (MT) [22]. Furthermore, using electric twitch interpolation techniques of the gastrocnemius-soleus complex, some subjects with severe chronic WAD demonstrated noticeable deficiencies in their ability to volitionally and maximally activate their plantar-flexor muscles, a metric referred to as the Central Activation Ratio (CAR) [22]. These preliminary observations of reduced CAR as determined with electrically elicited twitch interpolation, suggest signs of disrupted descending neural commands [5, 44] While preliminary, low CAR values in our participants (58-62% volitional activation) are consistent with previous results for quadriceps in those with known SCI [35]. Moreover, these reduced CARs have shown laterality preference related to the side opposite to which the head was turned at the time of impact, adding preliminary evidence for cause-and-effect. Supporting this, occupant postures of cervical rotation in addition to rapid hyperflexion/extension would appear to provide a prime environment for potential damage to various tissues [68] including regions of the cord that contain white matter motor pathways (Fig. 6-5A, B).
and spinal cord injury [14], we have identified a subset of people with severe chronic symptoms that show signs of subclinical spinal cord damage using magnetic resonance spectroscopy [24] and magnetization transfer imaging (MT) [22]. Furthermore, using electric twitch interpolation techniques of the gastrocnemius-soleus complex, some subjects with severe chronic WAD demonstrated noticeable deficiencies in their ability to volitionally and maximally activate their plantar-flexor muscles, a metric referred to as the Central Activation Ratio (CAR) [22]. These preliminary observations of reduced CAR as determined with electrically elicited twitch interpolation, suggest signs of disrupted descending neural commands [5, 44] While preliminary, low CAR values in our participants (58-62% volitional activation) are consistent with previous results for quadriceps in those with known SCI [35]. Moreover, these reduced CARs have shown laterality preference related to the side opposite to which the head was turned at the time of impact, adding preliminary evidence for cause-and-effect. Supporting this, occupant postures of cervical rotation in addition to rapid hyperflexion/extension would appear to provide a prime environment for potential damage to various tissues [68] including regions of the cord that contain white matter motor pathways (Fig. 6-5A, B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree