Abstract
Objectives
To determine the influence of orthopedic treatment on quality of life (QoL) in children and adolescents with idiopathic scoliosis and treated with either the carbon brace (CMCR, corset monocoque carbone respectant la respiration ) or the Lyon brace. To compare these braces.
Patients and methods
A cross-sectional study on a population of 120 patients with idiopathic scoliosis, visiting for routine evaluation following the onset of an orthopedic treatment at the Centre des Massues in Lyon. Eighty-two patients used the carbon brace and 38 patients used the Lyon brace. The patients completed the SRS-22 questionnaire (where a low score means a bad QoL), an evaluation scale of QoL specific to spinal deformities, and visual analogue scales (VAS) for pain, motivation and QoL ranging from 0 to 100 mm.
Results
The QoL of Lyon brace-treated patients is significantly worse than that of patients treated with a carbon brace for the overall score (mean ± SD, 4.05 ± 0.37 vs 3.77 ± 0.46, P = 0.002) as well as for function ( P = 0.01), pain ( P = 0.001), and appearance ( P = 0.004). These results are confirmed by the VAS for QoL ( P = 0.001).
Conclusion
The use of the carbon brace and of the Lyon brace induces a reduction in QoL whatever the evaluation tool, either SRS-22 or VAS. However, the use of the Lyon brace impairs QoL more than the use of the carbon brace.
Résumé
Objectifs
Déterminer l’influence du traitement orthopédique sur la qualité de vie (QDV) des enfants et des adolescents porteurs d’une scoliose idiopathique et traités par corset monocoque carbone respectant la respiration (CMCR) ou corset lyonnais. Comparer les corsets entre eux.
Patients et méthode
Étude transversale portant sur une population de 120 sujets porteurs d’une scoliose idiopathique, en visite de contrôle suite à la mise en place d’un traitement orthopédique au centre des Massues à Lyon. Quatre-vingt-deux patients sont traités par CMCR et 38 patients sont traités par corset lyonnais. Les patients ont complété le questionnaire SRS-22 (un score bas signifie une mauvaise QDV), échelle d’évaluation de la QDV spécifique aux déformations du rachis ainsi que des échelles visuelles analogiques (EVA) de douleur, de motivation et de QDV graduées de 0 à 100 mm.
Résultats
La QDV des patients traités par corset lyonnais est significativement moins bonne que celles des patients traités par CMCR pour le score global (moyenne ± ET, 4,05 ± 0,37 vs 3,77 ± 0,46 avec p = 0,002) ainsi que dans les domaines de la fonction ( p = 0,01), de la douleur ( p = 0,001) et de l’image corporelle ( p = 0,004). Ces résultats sont confirmés par l’EVA QDV ( p = 0,001).
Conclusion
Le port du CMCR et du corset lyonnais entraîne une diminution de la QDV quel que soit l’instrument d’évaluation, SRS-22 ou EVA. Le port du corset lyonnais altère cependant plus fortement la QDV que le port du CMCR.
1
English version
1.1
Introduction
Taking into account the patients’ quality of life in the evaluation of our practices effects is not a novelty. In daily practice, the assessment by the caregivers of the quality of life of their patients has always – or at least for a long while – been part of the routine: it is naturally inscribed in the doctor–patient relation. It is the famous “How are you?” But it is informal, intuitive, and is lacking rigor. Introducing the concept of quality of life ( i.e. the patient’s degree of satisfaction/dissatisfaction and the importance it takes in the patient’s daily life) into the evaluation of the prescribed treatments, and all the more so in that of the candidate-drugs is, on the other hand, a quite recent practice which started only in the years 1940 and was reinforced by the definition given by the World Health Organization in 1994: “A measure of the individual’s perception of their position in life in the context of the culture and the value systems in which they live and in relation with their goals, expectations, standards and concerns”.
As far as scoliosis is concerned, quality of life is mostly measured through specific questionnaires . The most currently used is the one developed by the Scoliosis Research Society (SRS) which evaluates the specific problems related to scoliosis and gives a global view of well-being. SRS-24 was the first version with six questions in each of the domains concerning pain and function, as well as three questions about self image . Afterwards, nine questions were added for postoperative assessment. The development of this version resulted in questionnaire SRS-22 which was refined several times, validated, and translated in several languages .
Our concern is the impact of the onset of an orthopedic treatment on quality of life. Is quality of life with a brace influenced by the choice of the orthesis? Climent et al. in 1999 showed that the quality of life score is better with Milwaukee than with Boston or TLSO. The Cheneau brace induces a significant decrease in quality of life . Our study focuses on the Lyon brace and the corset monocoque carbone respectant la respiration (CMCR) , as these are the two most prescribed braces in our department.
1.2
Patients and methods
This is an epidemioclinical, cross-sectional study on 120 patients aged 7 to 20 years with idiopathic scoliosis of different clinical forms (double major, thoracic, thoracolumbar, double thoracic or triple) followed-up in the children-adolescents department of the Centre médicochirurgical des Massues in Lyon. The patients were recruited during their follow-up evaluation of orthopedic treatment between November 2008 and February 2009, at least 3 months after treatment start and until orthosis removal. The questionnaire was given during administrative registration to the consultation. We only enrolled children and adolescents wearing a CMCR or a Lyon brace. All patients with non-idiopathic scoliosis were not enrolled in this study, neither were those with associated disturbances. The informed consent of the children and of their parents was collected.
The study is non-randomized as there can be no random allocation between the two braces, the indications being different.
SRS-22 is a questionnaire specific to spine deformities. It has been validated in different languages among which French , and very recently German and Polish . Its five domains evaluate respectively function, pain, self image, psychosocial status and satisfaction with the treatment. Each of the 22 items are assessed from 1 to 5, 1 corresponding to the worst experience and 5 to the best experience. Lower scores mean worse quality of life. Maximal score is 110. This score is then divided by the number of items to which the patient answered, giving a maximum score of 5.
We have excluded the patients who did not answer to at least two questions in a sub-part, as the results would not be representative anymore.
We have also used a visual analogue scale (VAS) for pain due to the brace, a VAS for motivation and a VAS for quality of life graded 0 to 100 mm. For pain, 0 represents absence of pain, for motivation, 0 represents the best motivation, and for quality of life, 0 represents absence of discomfort in daily life.
The statistical analysis was performed with R software. A first analysis including the 120 patients was carried out, then a second one separating the population in two groups: the first one including the patients with the CMCR brace, the second including the patients with the Lyon brace. A level of significance of 0.05 was selected.
1.3
Results
The investigations were conducted at the Centre médicochirurgical des Massues in Lyon between November 2008 and February 2009.
The patients’ characteristics are shown in Table 1 . The most frequently used brace is CMCR (68%). Our population consists mainly of girls (85%), which is representative of scoliotic patients in France, and scolioses are mostly combined, followed by thoracolumbar and thoracic, and finally lumbar, triple curve or double thoracic scolioses.
| Parameter | Mean (SD) | Number (%) |
|---|---|---|
| Gender | ||
| Girl | 102 (85) | |
| Boy | 18 (15) | |
| Brace | ||
| Lyon brace | 38 (32) | |
| CMCR | 82 (68) | |
| Age (yrs) | 13.7 (2.3) | |
| Lyon brace | 14.7 (1.6) | |
| CMCR | 13.2 (2.5) | |
| Type | ||
| Combined | 71 (59) | |
| Thoracic | 20 (17) | |
| Thoracolumbar | 22 (18) | |
| Triple | 4 (3) | |
| Double thoracic | 1 (1) | |
| Lumbar | 2 (2) | |
| Cobb angle before treatment | 28.7 (8.4) | |
| Lyon brace | 37.21 (7.1) | |
| CMCR | 24.7 (5.5) | |
| Cobb angle on evaluation day | 24.3 (11.7) | |
| Evolution | ||
| Good | 99 (91) | |
| Bad | 10 (9) | |
| Risser | ||
| 0 | 32 (27) | |
| 1 | 12 (10) | |
| 2 | 13 (11) | |
| 3 | 12 (10) | |
| 4 | 33 (28) | |
| 5 | 16 (13) | |
| NA | 2 (1) | |
| Theoretical wear time | 17.6 (4.3) | |
| Actual wear time | 15.1 (5.8) | |
| Compliance to treatment | ||
| Good | 83 (69) | |
| Bad | 37 (31) | |
| Treatment duration (months) | 23.8 (19.8) | |
| Estimated remaining treatment duration (months) | 27.2 (25.7) | |
| Estimated total treatment duration (months) | 51.0 (32.3) |
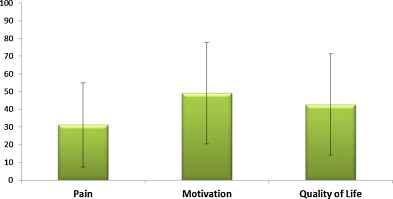
The VAS results are presented in Fig. 1 . As a reminder, 0 is considered as absence of pain, highest motivation, and absence of discomfort in daily life, respectively in the pain, motivation and quality of life VAS. We observe very high standard deviations in the three categories (pain, motivation and quality of life).
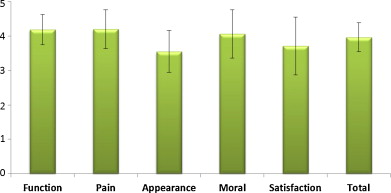
We now present the results obtained from questionnaire SRS-22 ( Fig. 2 ) made of five parts evaluating function, pain, self image, psychosocial status and satisfaction with the treatment. The mean of these five parts gives the total score. It is the self image which is the most impaired.
The population was separated in two subgroups, an MCR group and a Lyon group. There is a significant difference between the SRS-22 total score in brace and the type of brace ( P = 0.002). We then compared the results obtained with the different VAS according to the brace used ( Fig. 3 ).
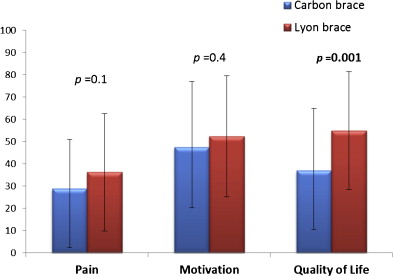
We note that pain is superior with the Lyon brace, and that motivation as well as quality of life are less good with the Lyon brace. We observe significant differences in the VAS for quality of life, the estimated quality of life being significantly better in CMCR.
In Fig. 4 , we represent the results obtained in questionnaire SRS-22 according to the brace used.
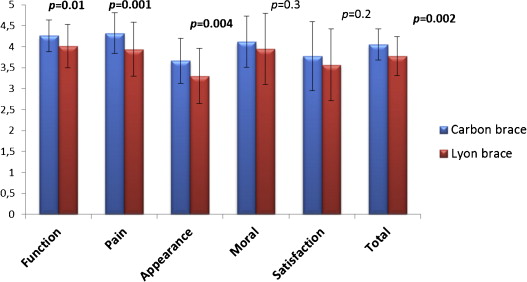
We observe that all results are inferior with the Lyon brace.
Regarding SRS-22, the differences are significant for:
- •
function;
- •
pain;
- •
self image;
- •
total score, always with a lesser impact with CMCR.
1.4
Discussion
Several publications focus on quality of life with a brace but show opposite results. Some authors have shown that wearing a brace does not alter quality of life. On the opposite, others have noted psychological impact and negative consequences on quality of life. Our results show that there is a negative influence of wearing a brace on quality of life when considering the scores of questionnaire SRS-22. These results are correlated with those found in literature but concerning other types of braces. The Lyon brace is studied in an article by Aulisa et al. , but is compared to the PASB brace, which seems to less negatively impact the quality of life than the Lyon brace (with questionnaire BRQ). Without mentioning the type of brace used in their study, the Climent team has shown, by using another scale for quality of life (Quality of Life Profile for Spine Deformities), a significant alteration of the global score of quality of life, of the psychosocial status and of back flexibility . Other authors have noted an impairment of self image.
Reichel and Schanz have shown in a study published in 2003 that groups of psychological support or individual sessions with a psychologist had a positive effect in the prevention of psychosocial disturbances in a population of scoliotic patients . In the children and adolescents physical and rehabilitation medicine department of the Centre des Massues , the setting up of a brace is performed on the basis of 1 to 2 weeks of hospitalization, and physicians, physiotherapists and orthoprosthesists work in close collaboration. The department psychologist may intervene at the request of one of the practitioners, of the children or of their parents.
In our population of 120 scoliotic children and adolescents orthopedically treated, it is the self image which is the most altered, then the psychosocial status; thereafter the presence of pain and finally the alteration of the function. In the found studies, there is no scoring of the subparts of the questionnaires. We only know that the results of the study by Pham et al. in 2008 have shown that wearing a brace and the daily duration of its wearing have a negative influence on global quality of life and on the following specific domains: psychosocial status, sleep disturbances, self image and back flexibility . The influence of the type of brace has well been shown by Climent et al. in 1999 . In this study, the patients treated with a Milwaukee brace had a better quality of life score than the patients with a Boston brace or a TLSO. Moreover, the patients with a Charleston brace had the worst quality of life scores. Our results show that the global score of quality of life is better with the CMCR than with the Lyon brace ( P = 0.002); likewise in the specific domains such as function ( P = 0.01), pain ( P = 0.001) and self image ( P = 0.004); but CMCR bracing induces a decrease of the quality of life score despite all its advantages (lightness, estheticism, respect of the respiration).
Still in the same study, Climent et al. have shown that quality of life was significantly correlated with age. We were able to verify it in our study, but contrarily to them, we have not found a correlation between global score and bone maturity (Risser), and treatment duration and evolution. On the other hand, we found a significant correlation between global score and the estimated remaining treatment duration ( P = 0.0001) which was not assessed in their study.
We have chosen for our study to compare two “underarm” braces, which are, despite their differences in indication, very close in terms of mobility while wearing the brace and of location of the pressure points. Unlike us, Climent et al. in 1999 compared completely different braces: the Milwaukee being a brace with a neck collar (visible when dressed) and therefore very badly tolerated by the adolescents but allowing a great freedom of movement of the upper limbs as well as of the ribcage; the Boston and the TLSO being “underarms”, and the Charleston being a brace in hypercorrection .
In our work regarding the VAS, all results are in favor of the CMCR with a significant difference for quality of life. These results are correlated with those found in the SRS-22 questionnaire.
All domains of the SRS-22 are reached, whatever the type of brace. The lowest mean is that obtained in the “self image” part, with either the CMCR or the Lyon brace.
A significant difference in function ( P = 0.01) is observed in favor of the CMCR, supposedly thanks to the mobile hands of the CMCR which, as it should be confirmed by an ongoing study performed at the Centres des Massues , would less decrease the respiratory vital capacity than the fixed pressure points of the Lyon brace.
The significant difference in the pain part of SRS-22 ( P = 0.001), which is not found in the VAS, may be explained by the fact that the angles at start are superior with the Lyon brace (mean of 37° in Lyon brace and 25° in CMCR), the pressure at the leaning points being therefore superior since there is more to correct. In addition, it can be assumed that the fixed pressure points are more painful as they restrict more the movements of the ribcage.
Regarding self image ( P = 0.004), this significant difference may have a two-fold explanation. The first is that the initial angles are more important in the Lyon brace group: the external deformations are therefore more important and less esthetic. The second is that the Lyon brace is made of masts, of metal rods, and of latches with hinges and screws, unlike the CMCR which is made of recent and discrete material (carbon, high density polyethylene) and closes with self-gripping bands.
Our study is open to criticism since some of its methodological aspects deserve to be discussed.
Our two groups are significantly different in terms of age, Cobb angle before treatment, Cobb angle on the day of evaluation, theoretical wear time, real wear time and estimated remaining wear time. This is explained by the fact that the two selected braces do not have the same indications: the Lyon brace is an integral part of the Lyon orthopedic treatment and is prescribed after start of puberty for the stiff scolioses and of an angulation greater than 25°. The CMCR is prescribed from early childhood for clinically reducible scolioses and of moderate angulation.
Despite this, we have performed our study, reinforced by the publication of Nachemson and Peterson in 1995 who insisted on the fact that a methodology in which the physicians adhere to their treatment method is considered as a better alternative to randomization .
Our results are certainly biased by the fact that the daily wear time is inferior in CMCR and that the initial deformations are different. Therefore it would have been interesting to know the quality of life scores in children and adolescents with idiopathic scoliosis non-orthopedically treated, as well as in a population of children and adolescents without any spinal pathology. Moreover, SRS-22 contains items adapted to a population of 7 to 99 years. This questionnaire does not take into account important domains of the children’s and adolescents’ life such as the quality of the sleep, sports activities, compliance to treatment and the parents’ role in the treatment acceptance. According to different authors indeed , a limitation of the physical and social activities may appear during bracing treatment. The role of the parents in the acceptance of the brace seems on the other hand to be of importance.
1.5
Conclusion
Wearing the CMCR brace induces a less important alteration of the quality of life score than the Lyon brace in the treatment of idiopathic scolioses in children and adolescents. The quality of life aspect must now be an integral part of the brace designing requirements. This study shows that progress is still to be made in terms of esthetics, pain, and acceptance of the brace. Further thoughts need to be given within a multidisciplinary team: physicians, physiotherapists, ergotherapists and orthoprosthesists for the brace design, and psychological support must be systematically proposed to the children and their family for a complete acceptance of the proposed treatment.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






