Unfortunately, the literature has little guidance for revision elbow surgery. This article attempts to supplement what is known in the literature with the author’s anecdotal experience. With this article, it is the author’s hope that the reader may learn from his or her successes and his or her failures without having to discover them first hand. There is good reason for angst to overcome surgeons looking at radiographs depicting a traumatized proximal ulna or radius. Surgeons know that there is a good chance they will be seeing these patients for a long time.
Key Points
- •
To prevent certain complications, surgical intervention to a traumatic elbow should be performed within 24 hours from the initial injury.
- •
The elbow remains an unforgiving joint, and the room for error is very small when addressing traumatic injuries to the proximal ulna and radius. Consequently, complications with elbow trauma are inevitable.
- •
Elbow revision surgery is one of the most difficult orthopedic surgeries in the anatomy, both conceptually and technically.
Proximal forearm fractures
Introduction
Traditionally, the discussion pertaining to elbow fractures tends to focus on supracondylar humerus fractures. Receiving less attention is the important, and arguably more complex, distal portion of the joint. This joint comprises 3 separate articulations, the ulnohumeral, radiohumeral, and radioulnar joints, each with their own goals for function and series of complications after trauma. Further, any pathology present in the elbow inevitably influences the function at the adjacent wrist either directly or indirectly. The elbow remains an unforgiving joint, and the room for error is small when addressing traumatic injuries to the proximal ulna and radius. Consequently, complications with elbow trauma are inevitable. Elbow revision surgery is one of the most difficult orthopedic surgeries in the anatomy, both conceptually and technically. This report is intended to assist surgeons in avoiding problems before they happen and managing these problems when they happen.
To prevent certain complications, surgical intervention to a traumatic elbow should be performed within 24 hours from the initial injury. If the patient is medically unstable, delayed intervention may be elected until the patient is more stable. It is also preferable for the initial surgical intervention to be definitive and resist the temptation to return to the operating room for a staged procedure, particularly in the acute phases of the injury. Therefore, if an injury is outside the limits of the surgeon’s comfort level, it is our belief that the patient’s outcome would be better if the surgery was delayed until more expertise may be consulted. In other words, if given the choice of provisionally fixing the elbow or delaying surgery until definitive fixation may be obtained, the surgeon should choose the latter.
The indications for operative treatment vary depending on the particular injury. The following paragraphs summarize the indications for operative intervention for each part of the anatomy.
Indications and Contraindications
Proximal ulna
Olecranon
Only completely nondisplaced olecranon fractures and comminuted fractures in elderly patients with an intact extensor mechanism may be treated nonoperatively. Any displacement of the olecranon cannot be reduced and stabilized by closed means and requires open reduction and internal fixation.
Ulnar metaphyseal/diaphyseal junction
Comminuted fractures and all displaced fractures distal to the midpoint of the semilunar notch are considered unstable and require operative intervention. Although simple, nondisplaced fractures of the metaphyseal/diaphyseal junction may be treated nonoperatively, vigilance is required because these fractures suffer late displacement even with proper immobilization and patient compliance. The degree of fracture displacement in the metaphyseal/diaphyseal junction often is difficult to assess with common radiographs. Despite this challenge, it is imperative that the alignment of the proximal ulna be anatomic or the proximal radioulnar joint will be compromised.
Radial head and neck
The radial head and neck heal very well nonoperatively, making operative intervention only indicated in 3 situations: (1) open fracture, (2) bone fragments blocking supination or pronation, or (3) the buttress of the radial head is required to stabilize the elbow that otherwise has been compromised by associated ligamentous or other bony injuries. Certainly, there are parameters reported in the literature to predict joint blocking or instability, but the most reliable method to definitively determine the need for operative intervention is to take the joints through an arc of motion under local, regional, or general anesthesia. For example, local anesthesia may be administered easily in the office setting to evaluate for bony blockage. General anesthesia should be reserved for cases that are highly suspicious for instability or blockage so that the surgeon is prepared to surgically intervene in the same sitting.
Combination injuries
Combined injuries often impart complex instability patterns to the elbow and usually require operative intervention. If fracture patterns do not necessarily suggest a need for fixation by themselves, but the joint stability remains uncertain, examination under anesthesia tends to be the best way to determine the need for operative management. In these cases, general anesthesia should be used so that the surgeon is prepared to surgically intervene in the same sitting.
Management
Proximal ulna
Olecranon
Operative approach
A longitudinal posterior incision is traditionally required for adequate exposure of the olecranon. The length of incision begins at the most proximal point of the olecranon, curves laterally around the olecranon prominence, and continues distally along the subcutaneous border of the ulna, enough to expose the fracture and place the necessary hardware. The subcutaneous flaps are retracted with the deep fascia and periosteum in a full-thickness manner.
Stable
Transverse, displaced fractures proximal to the midpoint of the semilunar notch may be treated using several options. Traditionally, tension banding techniques have been reserved for this fracture pattern. The technique was described to theoretically convert the bending forces the olecranon fragment to compressive ones. It is important to realize that this conversion of bending to compression forces has not been proven either clinically or in a biomechanics laboratory. Despite this, the technique has been popular for many years. Recently, there has been a trend away from this technique for more rigid constructs, such as plating. Most would agree that plating provides a more rigid construct over tension banding. Although it has been well accepted that tension banding has a lower profile than plating and theoretically will have less need for hardware removal, this has not been shown in the literature. Removal rates of 20%–100% have been reported for tension banding ; nearly equal to that of plating. The recent application of intramedullary nailing to olecranon fractures has been proposed as a method that combines the strength of plating with the relative imperceptibility of nailing. One clinical series with a minimum follow-up of 1 year showed that after implantation of a locked intramedullary nail, patients had no soft tissue irritation, and no occurrences of implant removal were reported.
Fractures usually are reduced with a tenaculum under direct visualization. It is important to expose the fracture medially and laterally to assess the adequacy of reduction and remove any interposed tissue. Extending the elbow and reducing tension of the triceps tendon may facilitate reduction until provisional fixation may be placed. Once reduced, either 2 parallel 0.062-in Kirchner pins or a 7.3-mm partially threaded cancellous screw may be placed antegrade across the fracture site. Traditionally, 18-gauge stainless steel wire is used to tension the construct in a figure-8 fashion. Some surgeons have advocated using #5 braided suture for the same purpose with the intention of avoiding the soft tissue irritability of the metal wire. Whether this is successful is entirely anecdotal.
Unstable
Comminuted fractures or fractures extending distal from the semilunar notch are considered unstable and are not amendable by any form of tension banding. Plating has been the standard fixation for these fractures. Although these implants are strong and reliable, they have high rates of soft tissue irritation and often require hardware removal. One study suggests that surgeons may not be aware of the extent these implants affect patients. In a survey distributed to 538 surgeons, most of them believed their implant removal rate to be less than 30%. Patients, however, reported a removal rate of 65%. Although surgeons believed that they removed the implant they originally placed in 92% of cases, patients reported that they only returned to the original surgeon for removal 13% of the time.
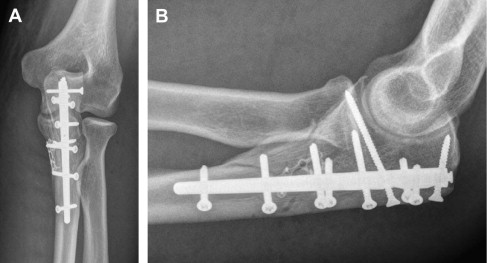
Recently, intramedullary nails have been developed to overcome the shortcomings of traditional olecranon fixations in terms of soft tissue irritation and the subsequent need for removal. Of the 3 intramedullary nails currently on the market, only one (OlecraNail, Mylad Orthopedic Solutions Arlington, VA, USA) is indicated for unstable, comminuted fractures ( Fig. 1 ). Similar to a locking plate, this particular nail has a fixed-angle design and rigidly stabilizes bone fragments in all planes. A recent biomechanical study compared nailing to locked plating for unstable olecranon fracture fixation in a cadaveric model. Both implants controlled fragments equally well and survived an equal number of cycles. The nail, however, held fragments stable under statistically significantly greater maximal loads, suggesting that nailing may be of benefit to patients that must weight bear with their upper extremities in the immediate postoperative period. Clinically, one report showed excellent results of locked intramedullary nailing for unstable proximal ulna fracture, including comminuted fracture-dislocations and fractures involving the coronoid. All fractures achieved union by 8 weeks after surgery, and all patients had motion within 10° in the contralateral elbow within 12 weeks after surgery.
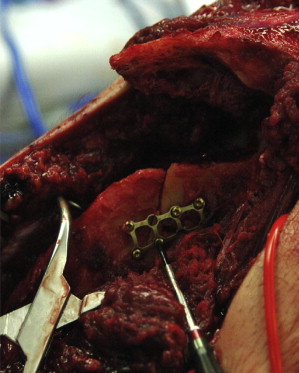
Regardless of the fixation method chosen, most complications arising from unstable olecranon fracture management come from improper reduction. The sigmoid notch must be scrutinized. Anything short of a perfectly anatomic reduction will result in loss of motion in the short term and posttraumatic degeneration in the long term. One common method used by surgeons is to reduce the easily visible posterior cortex and assume that the anterior surface followed. Although this technique may work well for simple fracture patterns, one must realize that, in comminuted fracture patterns, the articular portion of the olecranon often is detached from the posterior cortex. With these fractures, the joint surface may be completely malreduced, despite an anatomic reduction of the posterior cortex ( Fig. 2 ). A more appropriate technique is to reduce the bone in layers beginning with the articular surface ( Fig. 3 ). Once the joint is anatomically reduced, the next layer of fragmented bone just posterior to the joint is reduced before moving on the next layer. Some fragments may be trapped between 2 other fragments, whereas others may need provisional fixation such as 0.045-in Kirchner wire. With this technique, the posterior cortex is the last layer, not the first, to be reduced. After all layers have been reduced and provisionally fixed, definitive fixation is placed, usually using one or more plates and screws or a fixed-angle intramedullary device.

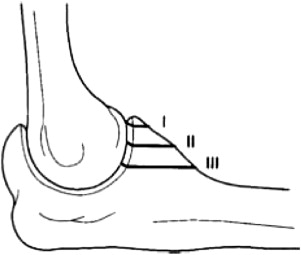
Coronoid
Management of coronoid fractures has been evolving in recent years. Only recently has the importance of its 3 dimensionality been appreciated but still not fully understood. Regan and Morrey proposed a classification system based on the 2-dimensional lateral view of the elbow radiograph ( Fig. 4 ). According to this familiar classification, type I (tip) fractures rarely require surgical treatment, type II (midportion) fractures may require surgical treatment, and type III (base) fractures usually require surgical treatment. The coronoid can no longer be thought of as a 2-dimensional image viewed on the lateral elbow radiograph. Although fractures may appear to fragment in this fashion on plain radiographs, in actuality, coronoid fracture patterns are far more complex and often cannot be fully realized without 3-dimensional imagery. Doornberg and Ring found that stable anatomic fixation of the anteromedial facet of coronoid fractures was associated with better outcomes.
The coronoid may be thought of as 3 separate regions: (1) the coronoid process, (2) the medial facet, and (3) the medial wall. Each region, if compromised, may impart instability to the elbow and consequently must be addressed individually. Deforming forces generally tend to displace fragments anteriorly and distally. Fixation must resist these substantial forces, ideally, to allow early postoperative motion. Unfortunately, early motion may not be possible when dealing with these fractures. Many fixation options are tenuous and may require protection with joint immobilization. Alternatively, hinged external fixation may neutralize the deforming forces during joint motion and should be considered in select cases.
Operative approach
Challenges of managing coronoid fractures reside in 3 categories: (1) identification of fracture pattern, (2) surgical approach and reduction, and (3) rigid fixation. Each category builds on the one before. As previously stated, identification of the fracture pattern and operative planning can be assisted greatly by 3-dimensional imagery techniques. Once it is determined which fragments need to be addressed, surgeons must plan their approach. This may take other associated injuries into consideration. Skin incisions tend to be irrelevant because subcutaneous tunnels may be developed readily and circumferentially around the elbow. The decision to approach the joint through facial planes seems to be more of an important issue.
We rarely use an anterior approach, however, others have used it very well. We prefer to address the coronoid from either a posterior-medial or anterior-medial approach. A posterior-medial approach is adequate for the reduction of smaller coronoid fragments or anchoring the anterior capsule back to bone. After exposing the posterior ulna, the medial portion of the ulna adjacent to the coronoid is dissected in a subperiosteal fashion. At the level of the coronoid, the ulnar nerve typically will lie in the flexor carpi ulnaris (FCU) and should be safe from a dissection remaining on the bone, but care must be exercised. Also at risk is the medical collateral ligament (MCL), which is attached to the medial facet. Detachment of the ligament should be avoided because it will compromise the vascularity of the fragment and sacrifice the stability of the joint. If reduction proves impossible without detachment of the ligament, then it should be detached at its origin on the humerus and reattached with bone tunnels or suture anchors. This proximal repair is far more predictable than reattaching distally. Reduction of the coronoid may be facilitated if there is an associated olecranon fracture. Access to the coronoid may be achieved through the window provided by a displaced olecranon fracture. After the coronoid is reduced and fixed, the olecranon may be repaired. Although this technique makes conceptual sense, its practical execution can be problematic because it is often difficult to reconfigure the semilunar notch without an intact or anatomically reduced olecranon to guide the reduction of the coronoid.
If the coronoid involvement is extensive, more exposure may be necessary. In these cases, we prefer an anterior-medial approach through the FCU. It is preferable for postoperative rehabilitation to leave the posterior aspect of the FCU attached to the medial epicondyles. Once the anterior FCU is detached from the medial epicondyles and reflected distally, the exposed brachialis is retracted anteriorly for a complete view of all portions of the coronoid. We routinely decompress the ulna nerve but do not transpose. The MCL is addressed in the same manner as was previously described for the posterior-medial approach.
Once the fragments are reduced, the surgeon has an assortment of fixation techniques from which to choose. Larger fragments may be secured with screws directed either posterior to anterior or anterior to posterior depending on the particular approach. It is important to understand the limitation of screw fixation. They simply grasp the fragment rather than buttress it. Consequently, in many cases, this fixation must be protected with either temporary immobilization or neutralization with a hinged external fixator for 3 weeks. Plates may be used to buttress the deforming forces, but the amount of hardware necessary to capture all aspects of the coronoid can be substantial if multiple fragments are involved. Small fragments may be excised, and the anterior capsule may repaired to the remaining coronoid using bone tunnels or suture anchors. Although this soft tissue repair can impart stability to the joint, it should be protected by a hinged external fixator for 3 weeks, especially if a relatively large portion of the coronoid is excised.
Garrigues and colleagues examined various coronoid fixation techniques after terrible triad injuries and found that the best results were found using a suture lasso technique. This technique was more stable than repair using suture anchors or lag screws before and after repair of the lateral ulnar collateral ligament. Lag screw fixation was associated with more implant failure, and suture anchors were associated with more nonunion and malunion than the suture lasso technique.
Proximal radius
Operative approach
Radial head and neck fractures may be approached through a Kocher incision. This incision may be extended proximally by detaching the extensor wad from the lateral epicondyles, but the dissection must remain anterior to the lateral collateral ligament to preserve its integrity. Should detachment be necessary, it is removed at its proximal origin on the humerus to be later reattached with suture anchors or bone tunnels. It is preferable to preserve the annular ligament. However, sacrificing the annular ligament does not lead to the instability as previous teachings have stated, but its incision and repair will likely cause more fibrosis that may limit supination and pronation. Distal extension of the Kocher incision may be made by pronating the forearm, which displaces the posterior interosseous nerve out of the operating field. However, a recent cadaver study has shown that pronation of the forearm in a setting in which the proximal radius or radial neck is fractured does not move the posterior interosseous nerve (PIN) out of the operative field, especially if injury to the interosseous membrane is present.
Simple radial head fractures may be treated with headless compression screws. A commonly displaced fragment from the anteromedial portion of the radial head, however, is not directly accessed through a lateral approach. Extreme manipulation in supination and pronation may help gain access to this problematic fragment. In some cases, screws may need to be advanced through intact bone as the displaced fragment is lagged into proper position. Overcompression of osteopenic or comminuted radial head fragments can cause the articular surface to deform and result in loss reduction. Bone grafting used in conjunction with adjustable compression screws currently on the market offer a good solution to this problem.
Plastic deformation of the radial head fragments during the time of injury may compromise reduction and overall outcome. If the radial head does not reduce easily or if it does not appear concentric with the capitellum after reduction attempts, the surgeon must suspect that some degree of plastic deformation has occurred. To remedy this problem, the articular surface must be reduced using the adjacent capitellum as a template.
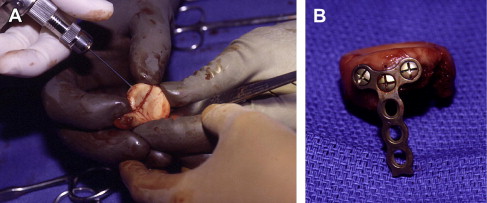
This reduction will inevitably leave gaps at the base of the fragment, which should be grafted with autologous corticocancellous bone from the olecranon or bone substitute. We prefer corticocancellous grafts primarily for the adjuvant stability they provide to the fixation construct. Once the reduction is anatomic and the bone graft in place, definitive fixation is implanted.
In comminuted articular fractures that involve the radial head and neck, it is helpful to assemble the radial head on the back table. Once the articular surface has been repaired, the head can be secured to the shaft with a plate ( Fig. 5 ). Alternatively, screws can be used, but we have found this to be less stable. In especially comminuted cases, rigid fixation is important because union may be delayed. The drawback to this rigid plate fixation is that it requires a significant amount of hardware to remain on the surface of the bone, and soft tissue adhesions could pose a problem. However, Smith and colleagues could not show a significant difference in elbow range of motion when comminuted radial head fractures were treated with screws alone versus plates, although there was a trend toward improved range of motion in the screws alone group. Traditionally, we favor stainless steel, low-profile locking plates, given their strong screw tensile strength in providing a fixed-angle buttress and low propensity for adhesions. Recent titanium implants have improved their polishing processes, which have lessened their adhesion potential, but the tensile strength concerns still remain a question.
There has been a recent trend to replace, rather than repair or excise, radial heads. This trend is especially true in complex fracture dislocations of the elbow and has led to many reports of complications ranging from chronic pain and capitellar degeneration to rotary instability. Improvements in design and techniques have addressed some of these complications, but surgeons should counsel patients that once a prosthetic radial is implanted, it is likely to require removal in the future. Although we prefer to repair the radial head when possible, including up to 4-part fractures, we acknowledge the short-term benefits of replacement. Radial head integrity, either comprised of bone or metal, plays an essential role in traumatic complex elbow instability. Although experts disagree on whether replacement is preferred to excision in cases of chronic radiocapitellar degeneration, most would agree that excision has no place in the acute setting, particularly if the medial collateral ligament has been compromised. It was found that patients who underwent open reduction internal fixation for Mason type III radial head fractures have better forearm rotation and elbow extension strength along with better functional outcomes when compared with those who underwent resection of the radial head. However, in isolated radial head fractures with no elbow instability, satisfactory results have been found in greater than 90% with resection of the radial head.
For these cases in which the radial head is irreparable, replacement greatly helps stabilize the lateral column of the elbow and allows for early postoperative motion. Bipolar radial head prostheses for radial head fractures have been successful in 39 of 51 patients in a series, but osteolysis adjacent to the implant caused alarm when used in young or active patients. Doornberg and colleagues also found radiolucency adjacent to radial head implants but could not correlate this with poor outcome in short-term follow-up. These authors also recommended intentionally loosely implanting the radial head prosthesis. In addition to the use of radial head implants in the acute setting, metallic radial head arthroplasty has shown favorable results when used for chronic posttraumatic proximal forearm disorders.
Our experience with partial or complete allografts has been disappointing, as resorption is common within months, which is consistent with previous reports. Alternatively, we have attempted fashioning autograft iliac crest to resemble partial or complete radial heads ( Figs. 6 A and 6 B). Anecdotally, incorporation of these autografts tends to be slightly more reliable, with partial grafts faring much better than complete grafts. We believe these autografts should only be considered when other options, such as prosthetic head or hinged external fixator, are not available.
Combination injuries/soft tissue injuries
Lateral collateral ligament (LCL) injuries are essentially ubiquitous in simple elbow dislocations and elbow fracture-dislcocations. Fraser and colleagues found that repair of the LCL with suture anchors restored the stability of the elbow in cadaveric subjects. Pollock and colleagues studied 10 cadaveric elbows biomechanically with various coronoid fractures and LCL ruptures and found that in 2.5-mm anteromedial facet coronoid fractures, LCL repair restored elbow stability, whereas in 5-mm anteromedial facet coronoid fractures, stability was not restored. Pollock concluded that small anteromedial facet fractures could be treated with LCL repair alone, whereas larger types needed internal fixation. This theory is also supported by Beingessner and colleagues. In a different biomechanical study done by Pollock and colleagues, the elbow was stable in Morrey type II coronoid fractures as long as both collateral ligaments were intact.
Although studies have found favorable outcomes after nonoperative treatment with early range of motion for simple elbow dislocations, elbows that are unstable after simple dislocation may require repair of the collateral ligaments. Jeon and colleagues repaired the MCL, LCL, or both ligaments in 13 elbows after simple dislocations that were unstable after closed reduction and found favorable results; none of the elbows redislocated. Heterotopic ossification developed in 6 of the elbows, but none of these affected the clinical outcome.
Terrible triad injuries of the elbow
Frequently, injuries to the proximal forearm are not isolated to one structure. These combination injuries can be especially challenging to treat. In terrible triad injuries, where the coronoid and radial head are fractured with an elbow dislocation, results were historically poor, hence the name terrible triad . Treatment algorithms have been developed for treatment of this complex injury. Acutely, many investigators choose to (1) stabilize the coronoid fracture if it is a Morrey type II or III; (2) repair or replace the radial head; (3) repair the LCL and assess for stability; (4) if unstable, then repair the MCL and again assess stability; and (5) if still unstable, consider dynamic external fixation. Some investigators skip step 4 and place an external fixator if the elbow is unstable after repair of the LCL. However, some surgeons repair the MCL after treatment of the radial head, coronoid, and LCL in terrible triad injuries even if the elbow is thought to be stable after repair of the LCL.
The LCL is always torn in terrible triad injuries and should be repaired with suture anchors or intraosseous sutures. Suture anchors and intraosseous sutures have equal failure loads when repairing the MCL, and both have higher failure loads when they are pretensioned. Forthman and colleagues examined 34 patients with intra-articular fracture dislocations of the elbow. Thirty of these patients had terrible triad injuries. Forthman and colleagues 50 (1) treated the coronoid fracture (most frequently with intraosseous sutures), (2) repaired or replaced the radial head, and (3) repaired the LCL. All elbows were considered stable, and the MCL was not repaired. Elbow instability developed in 2 of the patients because of noncompliance, whereas 25 of the remaining 32 patients experienced good or excellent results. Lindenhovius and colleagues treated terrible triad injuries in a similar manner as Forthman and colleagues, 50 although 3 patients in his study were placed in a dynamic external fixator and also showed favorable outcomes. In addition, the Lindenhovius study noted an improved flexion arc in patients treated within 2 weeks of injury versus patients treated more than 3 weeks from the injury.
Proximal forearm fractures
Introduction
Traditionally, the discussion pertaining to elbow fractures tends to focus on supracondylar humerus fractures. Receiving less attention is the important, and arguably more complex, distal portion of the joint. This joint comprises 3 separate articulations, the ulnohumeral, radiohumeral, and radioulnar joints, each with their own goals for function and series of complications after trauma. Further, any pathology present in the elbow inevitably influences the function at the adjacent wrist either directly or indirectly. The elbow remains an unforgiving joint, and the room for error is small when addressing traumatic injuries to the proximal ulna and radius. Consequently, complications with elbow trauma are inevitable. Elbow revision surgery is one of the most difficult orthopedic surgeries in the anatomy, both conceptually and technically. This report is intended to assist surgeons in avoiding problems before they happen and managing these problems when they happen.
To prevent certain complications, surgical intervention to a traumatic elbow should be performed within 24 hours from the initial injury. If the patient is medically unstable, delayed intervention may be elected until the patient is more stable. It is also preferable for the initial surgical intervention to be definitive and resist the temptation to return to the operating room for a staged procedure, particularly in the acute phases of the injury. Therefore, if an injury is outside the limits of the surgeon’s comfort level, it is our belief that the patient’s outcome would be better if the surgery was delayed until more expertise may be consulted. In other words, if given the choice of provisionally fixing the elbow or delaying surgery until definitive fixation may be obtained, the surgeon should choose the latter.
The indications for operative treatment vary depending on the particular injury. The following paragraphs summarize the indications for operative intervention for each part of the anatomy.
Indications and Contraindications
Proximal ulna
Olecranon
Only completely nondisplaced olecranon fractures and comminuted fractures in elderly patients with an intact extensor mechanism may be treated nonoperatively. Any displacement of the olecranon cannot be reduced and stabilized by closed means and requires open reduction and internal fixation.
Ulnar metaphyseal/diaphyseal junction
Comminuted fractures and all displaced fractures distal to the midpoint of the semilunar notch are considered unstable and require operative intervention. Although simple, nondisplaced fractures of the metaphyseal/diaphyseal junction may be treated nonoperatively, vigilance is required because these fractures suffer late displacement even with proper immobilization and patient compliance. The degree of fracture displacement in the metaphyseal/diaphyseal junction often is difficult to assess with common radiographs. Despite this challenge, it is imperative that the alignment of the proximal ulna be anatomic or the proximal radioulnar joint will be compromised.
Radial head and neck
The radial head and neck heal very well nonoperatively, making operative intervention only indicated in 3 situations: (1) open fracture, (2) bone fragments blocking supination or pronation, or (3) the buttress of the radial head is required to stabilize the elbow that otherwise has been compromised by associated ligamentous or other bony injuries. Certainly, there are parameters reported in the literature to predict joint blocking or instability, but the most reliable method to definitively determine the need for operative intervention is to take the joints through an arc of motion under local, regional, or general anesthesia. For example, local anesthesia may be administered easily in the office setting to evaluate for bony blockage. General anesthesia should be reserved for cases that are highly suspicious for instability or blockage so that the surgeon is prepared to surgically intervene in the same sitting.
Combination injuries
Combined injuries often impart complex instability patterns to the elbow and usually require operative intervention. If fracture patterns do not necessarily suggest a need for fixation by themselves, but the joint stability remains uncertain, examination under anesthesia tends to be the best way to determine the need for operative management. In these cases, general anesthesia should be used so that the surgeon is prepared to surgically intervene in the same sitting.
Management
Proximal ulna
Olecranon
Operative approach
A longitudinal posterior incision is traditionally required for adequate exposure of the olecranon. The length of incision begins at the most proximal point of the olecranon, curves laterally around the olecranon prominence, and continues distally along the subcutaneous border of the ulna, enough to expose the fracture and place the necessary hardware. The subcutaneous flaps are retracted with the deep fascia and periosteum in a full-thickness manner.
Stable
Transverse, displaced fractures proximal to the midpoint of the semilunar notch may be treated using several options. Traditionally, tension banding techniques have been reserved for this fracture pattern. The technique was described to theoretically convert the bending forces the olecranon fragment to compressive ones. It is important to realize that this conversion of bending to compression forces has not been proven either clinically or in a biomechanics laboratory. Despite this, the technique has been popular for many years. Recently, there has been a trend away from this technique for more rigid constructs, such as plating. Most would agree that plating provides a more rigid construct over tension banding. Although it has been well accepted that tension banding has a lower profile than plating and theoretically will have less need for hardware removal, this has not been shown in the literature. Removal rates of 20%–100% have been reported for tension banding ; nearly equal to that of plating. The recent application of intramedullary nailing to olecranon fractures has been proposed as a method that combines the strength of plating with the relative imperceptibility of nailing. One clinical series with a minimum follow-up of 1 year showed that after implantation of a locked intramedullary nail, patients had no soft tissue irritation, and no occurrences of implant removal were reported.
Fractures usually are reduced with a tenaculum under direct visualization. It is important to expose the fracture medially and laterally to assess the adequacy of reduction and remove any interposed tissue. Extending the elbow and reducing tension of the triceps tendon may facilitate reduction until provisional fixation may be placed. Once reduced, either 2 parallel 0.062-in Kirchner pins or a 7.3-mm partially threaded cancellous screw may be placed antegrade across the fracture site. Traditionally, 18-gauge stainless steel wire is used to tension the construct in a figure-8 fashion. Some surgeons have advocated using #5 braided suture for the same purpose with the intention of avoiding the soft tissue irritability of the metal wire. Whether this is successful is entirely anecdotal.
Unstable
Comminuted fractures or fractures extending distal from the semilunar notch are considered unstable and are not amendable by any form of tension banding. Plating has been the standard fixation for these fractures. Although these implants are strong and reliable, they have high rates of soft tissue irritation and often require hardware removal. One study suggests that surgeons may not be aware of the extent these implants affect patients. In a survey distributed to 538 surgeons, most of them believed their implant removal rate to be less than 30%. Patients, however, reported a removal rate of 65%. Although surgeons believed that they removed the implant they originally placed in 92% of cases, patients reported that they only returned to the original surgeon for removal 13% of the time.
Recently, intramedullary nails have been developed to overcome the shortcomings of traditional olecranon fixations in terms of soft tissue irritation and the subsequent need for removal. Of the 3 intramedullary nails currently on the market, only one (OlecraNail, Mylad Orthopedic Solutions Arlington, VA, USA) is indicated for unstable, comminuted fractures ( Fig. 1 ). Similar to a locking plate, this particular nail has a fixed-angle design and rigidly stabilizes bone fragments in all planes. A recent biomechanical study compared nailing to locked plating for unstable olecranon fracture fixation in a cadaveric model. Both implants controlled fragments equally well and survived an equal number of cycles. The nail, however, held fragments stable under statistically significantly greater maximal loads, suggesting that nailing may be of benefit to patients that must weight bear with their upper extremities in the immediate postoperative period. Clinically, one report showed excellent results of locked intramedullary nailing for unstable proximal ulna fracture, including comminuted fracture-dislocations and fractures involving the coronoid. All fractures achieved union by 8 weeks after surgery, and all patients had motion within 10° in the contralateral elbow within 12 weeks after surgery.







