Prosthetic Replacement for Proximal Humerus Fractures
Jay D Keener
Leesa M Galatz
INTRODUCTION
Proximal humerus fractures are common orthopedic injuries with an incidence that is increasing as the population ages. Over the last half of the 20th century there has been considerable advancement in the understanding of the principles regarding the pathoanatomy and healing of these injuries and the development of more uniform methods of classification and treatment. However, there remain many unanswered questions regarding the appropriate treatment of some proximal humerus injuries. The purpose of this chapter is to discuss the role of prosthetic humeral replacement in the management of selected proximal humerus fractures.
Interest in proximal humeral arthroplasty for the treatment of severe proximal humerus fractures began in the 1950s (1, 2, 3). Most early reports dedicated to the treatment of severe proximal humerus injuries produced uniformly poor results regardless of the method of treatment (4,5). At that time a variety of treatments were used including closed reduction and immobilization, open reduction and internal fixation, primary arthrodesis, or humeral head excision with variable but consistently unsuccessful outcomes. In 1955 Neer reported good results in the treatment of severe proximal humerus fractures with a metal prosthesis (1). His series of prosthetic replacement in 27 patients with proximal humerus fracture-dislocations was the first to note consistently good results with these severe injuries.
Redesign of the original prosthesis led to improvement in clinical outcomes in Neer’s series reported in 1986 (6). Current components reflect further advancements in the restoration of proximal humeral anatomy by introducing modularity to prosthetic designs.
Redesign of the original prosthesis led to improvement in clinical outcomes in Neer’s series reported in 1986 (6). Current components reflect further advancements in the restoration of proximal humeral anatomy by introducing modularity to prosthetic designs.
ANATOMY
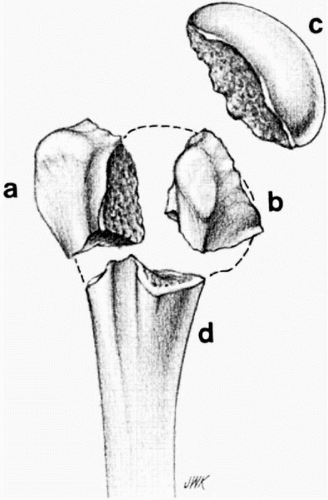
Re-creation of normal anatomy optimizes functional outcome after arthroplasty for proximal humerus fractures. Therefore, the surgeon should have a detailed knowledge of these anatomic relationships. The proximal humerus is composed of the humeral head, greater tuberosity, lesser tuberosity, and humeral metaphysis. The bicipital groove, an important anatomic landmark during surgical reconstruction, is located between the lesser and greater tuberosities along the anterolateral aspect of the proximal humerus. The anatomic neck is located at the junction of the tuberosities and the humeral head and serves as the attachment of much of the glenohumeral joint capsule. The surgical neck, a common site of fracture, is located distal to the tuberosities as they merge with the proximal humeral metaphysis. The lesser tuberosity forms the medial wall of the bicipital groove and serves as the insertion for the subscapularis muscle. The greater tuberosity forms the lateral wall of the bicipital groove and serves as the insertion for the supraspinatus, infraspinatus, and teres minor muscles (Fig. 12-1). The average medial-lateral width of the greater tuberosity is 9 ±2 mm, and the most superior aspect of the tuberosity lies 6 ±2 mm inferior to the superior aspect of the humeral head (7). This relationship must be reestablished for optimal outcome following proximal humeral arthroplasty.
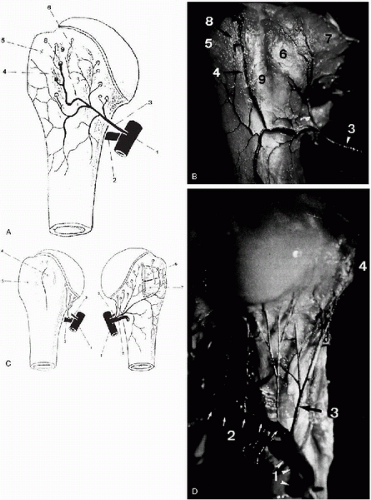
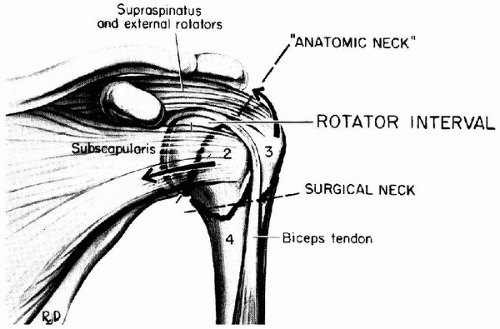 Figure 12-1 Anatomy of the proximal humerus. Drawing illustrating the rotator interval and the four major fragments of proximal humerus fractures: humeral head (1), lesser tuberosity (2), greater tuberosity (3), and shaft (4). Retraction of both tuberosities tears the rotator interval and involves both the surgical neck and anatomic neck levels. (Reprinted from Neer CS. Displaced proximal humerus fractures. Part 1—classification and evaluation. J Bone Joint Surg 1970;52A:1078, with permission.) |
The humeral head is elliptically shaped and oriented medially, superiorly, and posteriorly. The head is inclined 120 to 145 degrees in relation to the shaft with an average of 135 degrees inclination (8). The degree of humeral retroversion is highly variable with a range of 0 to 60 degrees and a mean of 20 degrees (9). A study using finedetail computed tomography (CT) scan demonstrated that normal humeral head retroversion ranges between 9 and 31 degrees with a mean of 19 degrees (7). The average vertical dimension of the articular surface of the humeral head is 48 mm with a radius of curvature of 25 mm. The average transverse diameter is 45 mm with a radius of curvature of 22 mm. The canal of the proximal humeral metaphysis is elliptical in shape with a variable degree of retroversion that correlates with the degree of humeral head retroversion (7). The glenoid articular surface is shallow, slightly concave, and shaped like an inverted comma. The articular surface area of the glenoid is approximately one third to one fourth that of the humeral head (10).
The vascularization of the humeral head is accomplished through an extensive extraosseous and intraosseous network supported by generous anastomoses. Despite the rich vascular network nourishing the humeral head, avascular necrosis can accompany displaced proximal humeral fracture-dislocations. The primary blood supply to the humeral head arises from the anterior humeral circumflex artery, a branch of the third portion of the axillary artery (11, 12, 13). This vessel travels laterally along the lower aspect of the subscapularis muscle and then ascends along the lateral side of the intertubercular groove to penetrate the bone at the superior junction of the greater tuberosity and intertubercular groove. The arcuate artery, the primary intraosseous branch, supplies the majority of the humeral head (13). Branches of the posterior humeral circumflex artery supply the posteromedial aspect of the humeral head. This vessel will anastomose with the arcuate artery in the region of the greater tuberosity and surrounding capsule (11). The humeral head is also nourished to a lesser degree from tendo-osseous anastomoses of the rotator cuff insertions at the greater and lesser tuberosities. Gerber and colleagues demonstrated that vascularization of the entire humeral head is only possible via the anterolateral branch (arcuate) of the anterior humeral circumflex artery (11). Brooks and associates showed that the humeral head could often be vascularized through intraosseous anastomoses between metaphyseal vessels and the arcuate artery after ligation of the anterior humeral circumflex artery (13) (Fig. 12-2).
The humeral head articulates with the glenoid through a dynamic interplay of capsuloligamentous restraints and muscular support afforded by the rotator cuff and deltoid muscles. The rotator cuff tendons along with the glenohumeral joint capsule and ligaments play a critical role in kinematics and dynamic stability. The subscapularis muscle inserts into the lesser tuberosity, whereas the supraspinatus, infraspinatus, and teres minor insert into
the three facets of the greater tuberosity. Tuberosity fractures display predictable patterns of displacement based on the pull of the attached rotator cuff musculature. Greater tuberosity fragments migrate in a superior and posterior direction from the pull of the supraspinatus and infraspinatus. Severely displaced fractures are often accompanied by a longitudinal tear in the rotator cuff. Lesser tuberosity fractures displace medially from the attachment of the subscapularis muscle. Surgical neck fractures are associated with anterior angulation as well as medial displacement of the humeral shaft created by the deforming force of the pectoralis major muscle.
the three facets of the greater tuberosity. Tuberosity fractures display predictable patterns of displacement based on the pull of the attached rotator cuff musculature. Greater tuberosity fragments migrate in a superior and posterior direction from the pull of the supraspinatus and infraspinatus. Severely displaced fractures are often accompanied by a longitudinal tear in the rotator cuff. Lesser tuberosity fractures displace medially from the attachment of the subscapularis muscle. Surgical neck fractures are associated with anterior angulation as well as medial displacement of the humeral shaft created by the deforming force of the pectoralis major muscle.
Pathologic Anatomy
A variety of coexisting pathologic conditions will influence the decision-making regarding the treatment of proximal humerus fractures, including the need for prosthetic replacement of the proximal humerus. Osteoporotic bone is common in elderly patients with low-energy proximal humerus fractures and often compromises the ability to obtain rigid internal fixation of the fracture fragments. Preexisting glenohumeral arthritis may necessitate glenoid resurfacing if prosthetic replacement of the proximal humerus is undertaken. Preexisting rotator cuff tears are often seen in the elderly and may have significant implications with regard to final strength and range of motion of the shoulder. Degenerative lesions or acute disruption of the long head of the biceps tendon may require tenodesis to the proximal humerus following fracture reconstruction.
PATHOPHYSIOLOGY
Classification
The classification of proximal humerus fractures is based on Codman’s identification of four major fracture fragments: the anatomic head, lesser tuberosity, greater tuberosity, and humeral shaft (14) (Fig. 12-3). Expanding on the work of Codman, Neer introduced his classification system for proximal humerus fracture-dislocations based on his observation of 300 fractures over a 14-year period (15). This is the most widely used classification system for proximal humerus fractures used today. His system takes into account fracture anatomy and fragment displacement, two factors that dictate choice of treatment options and provide valuable information about the prognosis of the fracture (10).
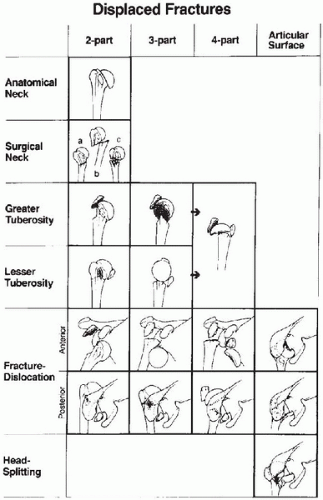
According to the Neer classification system, a fracture fragment is considered present only when it is displaced from the remaining proximal humerus or other fracture fragments. Displacement is noted when the fragment is separated by 1 cm or more or there is 45 degrees of angulation of the fragment. The clinical implication of displacement suggests potential instability of the fracture or possible disruption of the vascular supply to the humeral head. The majority of proximal humerus fractures are minimally displaced (15). Nondisplaced fracture lines or fragments with less than the previously mentioned displacement are classified as one-part injuries. Two-part fractures involve the greater tuberosity, lesser tuberosity, or surgical neck. Three- and four-part fractures involve a variety of combinations of the possible fracture fragments and are associated with higher rates of humeral head avascular necrosis. Neer also described proximal humerus fracture-dislocations that can occur with two-, three-, and four-part fractures. Dislocations are classified according to the direction of dislocation of the head fragment (anterior or posterior). In addition, Neer reported articular surface injuries including
head splitting and impression fractures. Both of these types of injuries can involve varying amounts of the humeral head with obvious implications regarding the viability of the articular surface (Fig. 12-4).
head splitting and impression fractures. Both of these types of injuries can involve varying amounts of the humeral head with obvious implications regarding the viability of the articular surface (Fig. 12-4).
The AO group has proposed a thorough system of classification of proximal humerus fractures based on the precise location of the fracture fragments, direction and severity of fracture displacement, and associated dislocation of the articular surface (16). Fractures are initially group into isolated extraarticular unifocal (Type A), extraarticular bifocal (Type B), and articular isolation (Type C) fractures. The groups are then further classified based on fracture alignment, direction and amount of displacement, and the presence of head impaction or dislocation (18). The emphasis of this system is on the vascular supply of the humeral head and the subsequent risk of osteonecrosis. Avascular necrosis of the humeral head is uncommon after Type A and B fractures but frequently complicates Type C fractures. Although more descriptive than the Neer classification system, the AO classification of proximal humerus fractures has not gained widespread popularity for clinical application because of its complexity and limited reproducibility.
Incidence
Proximal humerus fractures represent approximately 4% to 5% of all skeletal fractures (17). The majority of recent epidemiologic literature notes an increasing incidence of proximal humerus fractures that is felt to be related to osteoporosis in the aging population (17, 18, 19). Studies from Rochester, Minnesota, and Malmo, Sweden, have shown the age-adjusted incidence of proximal humerus fractures in adults to be 104-105 per 100,000 person-years (18,20). Proximal humerus fractures represent more than 75% of all humerus fractures in those older than age 40 years, with an incidence of approximately 70% of the reported rate of proximal femur fractures (18). The relationship of proximal humerus fractures to osteoporosis is confirmed by the correlation of a greater proportion of humerus fractures occurring proximally with advancing age and the age-related increase in osteoporosis. Additionally, there is a rapid increase in the incidence of proximal humerus fractures seen in postmenopausal women reflecting the common pattern of osteoporosis-related fractures (18,21,22).The incidence of proximal humerus fractures is likely to increase as the average lifespan of the population continues to grow, further emphasizing the need for effective treatments of these injuries to maintain the functional independence of affected individuals.
Pathogenesis and Related Injuries
The majority of proximal humerus fractures occur as the result of a fall. In younger patients with good bone stock, high-energy mechanisms are common and the fractures are often accompanied by other injuries. In multi-trauma victims, proximal humerus injuries are often overlooked because of the presence of more severe musculoskeletal or other life-threatening injuries. Older patients typically sustain proximal humerus fractures as a result of minimal to moderate trauma, such as a fall from standing height. Proximal humerus fractures have also characteristically been associated with seizure disorders or electric shock (23,24).
Associated injuries to the brachial plexus and axillary artery can accompany proximal humerus fractures (25,26). Stableforth reported a 4.9% incidence of axillary artery
injury in displaced proximal humerus fractures (27). Neer’s series of displaced proximal humerus fractures had no associated vascular injuries (15). The most common site of injury is proximal to the branch of the anterior humeral circumflex artery (28). Arterial injury, although rare, has also been reported even with minimally displaced fractures (29).
injury in displaced proximal humerus fractures (27). Neer’s series of displaced proximal humerus fractures had no associated vascular injuries (15). The most common site of injury is proximal to the branch of the anterior humeral circumflex artery (28). Arterial injury, although rare, has also been reported even with minimally displaced fractures (29).
Clinically detectable nerve injuries following proximal humerus fractures have been reported in up to 45% of cases (30). Stableforth reported a 6.1% incidence of brachial plexus injuries following displaced proximal humerus fractures (27). Isolated injuries to the axillary nerve have been reported as well (31). A recent electromyography study revealed a very high incidence of occult nerve injury following both nondisplaced (52%) and displaced (82%) fractures (32). The axillary and suprascapular nerves were most commonly involved. Often these injuries are incomplete and may manifest as temporary weakness that recovers along the same course of time as fracture healing. The risk of neurovascular injury following fractures of the proximal humerus is greater in high-energy injuries, fracture-dislocations, and penetrating trauma.
Although rare, concomitant chest-wall injuries have been reported with high-energy proximal humerus fractures (15,27). These include rib fractures, pneumothorax, and/or hemothorax. There have been several reports of intrathoracic humeral head penetration following displaced surgical neck fractures (33, 34, 35).
EVALUATION
History
The majority of proximal humerus fractures occur secondary to acute events well recognized by the patient. A thorough history can provide valuable information regarding the mechanism of injury and the likelihood of associated injuries. Younger patients typically sustain higher energy injuries such as motor vehicle accidents or falls from heights. These fractures can result from direct blows to the shoulder or more commonly from indirect mechanisms such as a fall to the outstretched hand. A high index of suspicion during the history can help the clinician identify symptoms of a more serious injury such as upper-extremity paralysis or paresthesias, open wounds, or dyspnea.
Older patients typically have lower energy injury mechanisms. Falls are the most frequent cause of fracture in this age group (21). A history of frequent falls or amnesia to the events surrounding the fall may signal cardiac or central neurologic problems. A history of head trauma or prior seizure disorder should be elicited as well. Altered sensorium noted during examination after a fall warrants immediate neurologic evaluation and imaging to rule out acute injury to the brain.
Physical Examination
The physical examination of the shoulder following proximal humerus fractures can be quite variable reflecting the wide spectrum of injury seen with this fracture. The majority of patients will complain of local pain in the upper arm and shoulder areas. Soft-tissue swelling occurs early, whereas ecchymosis is usually seen after 24 to 48 hours in gravity-dependent areas. Fracture-dislocations can alter the normal soft-tissue contours of the upper extremity. There is usually generalized tenderness to palpation of the proximal humerus that may be more localized with isolated fractures of the tuberosities. Attempted motion of the shoulder is painful and may be associated with crepitus and muscle guarding. The entire upper extremity, neck, and chest wall should also be examined for evidence of associated injuries.
A careful neurovascular examination is critical in the initial evaluation, especially with high-energy fractures. Timely identification and treatment of vascular injuries is critical in avoiding the complications of a dysvascular limb. The radial pulse is palpated and compared to the opposite arm when possible. Because of the extensive collateral circulation of the upper arm, a radial pulse may be palpated in the presence of a significant arterial injury (28). Doppler ultrasonography or angiography can be used to further assess the vascular anatomy in cases with diminished or absent pulses. Diffuse distal paresthesias are a sign of inadequate circulation and should raise the suspicion of vascular injury (28). The neurologic examination should encompass all components of the brachial plexus. Axillary nerve integrity is assessed by both sensory and motor function, although the latter is often inhibited by pain. Atony of the deltoid after proximal humerus fracture creating inferior subluxation of the humeral head is common and usually recovers in the subacute period (36, 37, 38). Distal motor and sensory examination of all peripheral nerves allows the clinician to assess each component of the brachial plexus and should be repeated at regular intervals if abnormalities are discovered.
Imaging Studies
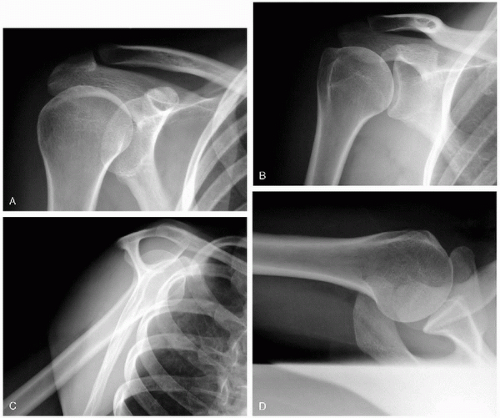
Radiographic evaluation of proximal humerus fractures is the foundation of proper patient evaluation and treatment. Plain radiography is the gold-standard method of initial evaluation and will serve to direct appropriate treatment. The standard series obtained to evaluate these injuries has been coined the “trauma series” and includes the anteroposterior (AP) and lateral views in the plane of the scapula and the axillary view. Alternatively, the authors recommend a standard AP view of the shoulder, an AP view of the scapula, and an axillary view. These orthogonal views allow multiplanar assessment of the fracture allowing appreciation of fracture lines and fragment displacement as well as orientation of the humeral head articular surface in relation to the glenoid (Fig. 12-5).
The scapula rests obliquely on the chest wall angled medially (toward the opposite shoulder) 35 to 40 degrees from the coronal plane. To obtain the AP and scapular lateral views, the angle of the beam and cassette should match the orientation of the scapula. The scapular AP view is taken with the cassette along the posterior aspect of the scapula and the beam angled perpendicular to the cassette. This view shows the true AP view of the glenohumeral joint with no superimposition of the humeral head and glenoid in the normal setting. The scapular lateral (scapular
Y) view is taken with the cassette along the anterolateral shoulder with the beam directed from posterior and medial toward lateral along the axis of the scapular spine. Displacement of tuberosity and shaft fragments and humeral head to glenoid orientation can be appreciated on this view. Both the AP and scapular lateral views may be obtained while the patient remains in a sling and can be performed in a variety of positions if needed. The standard AP view of the shoulder is taken with the cassette placed along the posterior shoulder parallel to the thorax while the beam is directed from anterior to posterior perpendicular to the thorax. Because of the orientation of the scapula on the chest wall, this image creates an oblique view of the glenohumeral joint. Because the arm usually rests in a position of internal rotation against the trunk, this provides an excellent view of the greater tuberosity. The axillary view provides valuable information that may not be seen on the AP and lateral views. Although this view is obtained with the glenohumeral joint abducted, only a small degree of elevation is necessary for an adequate radiograph and can usually be obtained in the acute setting. Physician assistance is sometimes required for proper handling of the acutely injured extremity. The cassette is placed superior to the shoulder, and the beam is directed to the cassette through the axilla. The axillary view best shows the relationship of the humeral head to the glenoid as well as posterior displacement of greater tuberosity fractures, anteriorly displaced lesser tuberosity fractures, head impression injuries, and associated glenoid rim fractures.
Y) view is taken with the cassette along the anterolateral shoulder with the beam directed from posterior and medial toward lateral along the axis of the scapular spine. Displacement of tuberosity and shaft fragments and humeral head to glenoid orientation can be appreciated on this view. Both the AP and scapular lateral views may be obtained while the patient remains in a sling and can be performed in a variety of positions if needed. The standard AP view of the shoulder is taken with the cassette placed along the posterior shoulder parallel to the thorax while the beam is directed from anterior to posterior perpendicular to the thorax. Because of the orientation of the scapula on the chest wall, this image creates an oblique view of the glenohumeral joint. Because the arm usually rests in a position of internal rotation against the trunk, this provides an excellent view of the greater tuberosity. The axillary view provides valuable information that may not be seen on the AP and lateral views. Although this view is obtained with the glenohumeral joint abducted, only a small degree of elevation is necessary for an adequate radiograph and can usually be obtained in the acute setting. Physician assistance is sometimes required for proper handling of the acutely injured extremity. The cassette is placed superior to the shoulder, and the beam is directed to the cassette through the axilla. The axillary view best shows the relationship of the humeral head to the glenoid as well as posterior displacement of greater tuberosity fractures, anteriorly displaced lesser tuberosity fractures, head impression injuries, and associated glenoid rim fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree