Prosthetic Management of Dysfunctional Instability and Periarticular Nonunions
Syed A. Hasan
Matthew L. Ramsey
INTRODUCTION
Background of the Topic
A stable and mobile elbow joint is a requirement for normal upper-extremity function. Stability is conferred on the elbow by the unique architecture of the articular surfaces and surrounding soft tissues. Motion through the elbow requires an intact joint to provide a fulcrum for the muscles crossing the elbow joint to exert their power. Disruption of the elements that confer mobility and stability to the elbow joint will compromise the ability to position the hand in space for functional activities.
Destruction of the fulcrum may result from a variety of causes. At the furthest extreme, the forearm is dissociated from the arm, resulting in loss of angular and longitudinal stability of the extremity, which results in a flail elbow. Less
severe joint destruction results in a pattern of instability where a modest degree of elbow motion can occur with the arm adducted against the side. However, when the arm is abducted away from the body, the fulcrum is insufficient to maintain stability with resultant dysfunctional instability.
severe joint destruction results in a pattern of instability where a modest degree of elbow motion can occur with the arm adducted against the side. However, when the arm is abducted away from the body, the fulcrum is insufficient to maintain stability with resultant dysfunctional instability.
The defining feature in patients with dysfunctional instability is the inability to position the arm in space because of inadequacy of the joint fulcrum required for useful function of the elbow. Useful function of the elbow can be restored by reestablishing a stable fulcrum. It is usually preferred if the fulcrum can be reestablished while sparing the native joint; however, there are circumstances where this is not possible or desirable. In these situations, total elbow arthroplasty is considered. Total elbow arthroplasty for patients with dysfunctional instability has evolved over the past decade into a reliable treatment option in carefully selected patients.
PATHOPHYSIOLOGY
As stated earlier, dysfunctional instability of the elbow describes a condition where the stable fulcrum required for elbow function is lost. Etiologies include severe rheumatoid involvement of the elbow, nonunion of the distal humerus, traumatic bone loss, and the surgical excision of the distal humerus in the management of infection.
A classification system is impractical because of the diversity of pathologies leading to dysfunctional instability. However, treatment is unified by the need to reestablish a stable fulcrum.
The problem of dysfunctional instability is rare. However, because of the varus force imparted on the elbow by the weight of the arm, the clinical significance of dysfunctional instability to the functional ability of an affected patient is profound. Depending on the degree of the instability, the patient may be able to perform certain nonweighted activities with the arm splinted against the side, only to manifest instability with the arm away from the body. With more profound degrees of dysfunctional instability, no activity can be performed efficiently.
EVALUATION
History
In eliciting a history from a patient with dysfunctional instability of the elbow, it is helpful to determine the mechanism of injury. Younger patients with dysfunctional instability usually have higher energy trauma than patients with rheumatoid arthritis. In this later group, preexisting disease deteriorates the subchondral and supracondylar bone to such a degree that minor trauma can cause a pathologic fracture of the supracondylar column resulting in dysfunctional instability.
Many patients considered for total elbow arthroplasty have had multiple previous surgeries. A careful chronology of the previous surgeries should be elicited. The number and type of previous surgery provides insight into previous efforts at stabilizing the elbow. Supporting documentation including office notes from previous treating physicians and operative notes should be obtained if one has not treated the patient previously.
A history of infection should be sought and thorough evaluation for infection should be performed before considering arthroplasty. If the preoperative workup for infection is negative and concern for infection remains high, a staged debridement of the elbow should be performed. At the initial surgery, cultures and tissue specimens are collected for analysis. Definitive implantation of the elbow arthroplasty is delayed until intraoperative cultures demonstrate no infection.
Physical Examination
The physical examination is directed at determining the magnitude of the instability and any associated findings that affect surgical decision making. The condition of the soft tissues should be carefully assessed. The location of previous surgical incisions and the integrity of the skin need to be evaluated.
Careful neurologic evaluation is mandatory. The ulnar nerve, in particular, needs to be thoroughly assessed. The ulnar nerve may have been repeatedly manipulated at previous surgery or may be scarred at the nonunion site. Additionally, the deformity that accompanies dysfunctional instability can cause traction on the ulnar nerve, resulting in a tardy ulnar nerve palsy.
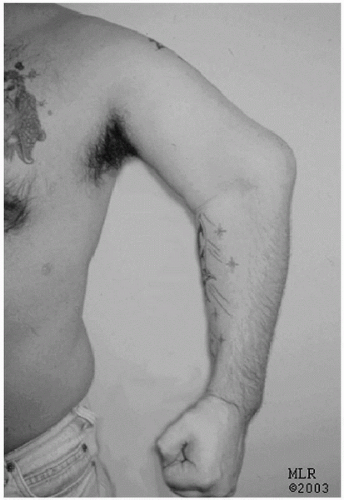
Range of motion in the sagittal plane with the arm adducted against the side is assessed. Patients with minor degrees of instability have enough of a fulcrum at the side to demonstrate active range of motion. Abduction of the shoulder creates a varus moment across the elbow, which compromises the fulcrum with resultant instability (Fig. 28-1). Patients with a flail elbow have dissociation of the forearm from the arm, resulting in loss of angular and longitudinal stability of the arm. The forearm displaces medially relative to the brachium and eventually shortens because of the pull of the flexors and extensors of the arm.
Imaging Studies
Standard anteroposterior (AP) and lateral radiographs are usually sufficient to provide an appreciation of the degree of pathology. The goal of imaging studies is to identify the underlying cause of dysfunctional instability and assess the integrity of the elbow joint, in particular the ulnohumeral joint.
Fixed deformities of the elbow can make standard imaging difficult to interpret. The inability to fully extend the elbow projects the humeral shaft in a true AP plane,
whereas the distal humerus fragment is projected out of plane making it appear smaller than it actually is. This may erroneously lead to the conclusion that the joint is not salvageable. Advanced imaging, including computed tomography (CT) or magnetic resonance imaging (MRI), is rarely indicated and provides little additional information that aids clinical decision making.
whereas the distal humerus fragment is projected out of plane making it appear smaller than it actually is. This may erroneously lead to the conclusion that the joint is not salvageable. Advanced imaging, including computed tomography (CT) or magnetic resonance imaging (MRI), is rarely indicated and provides little additional information that aids clinical decision making.
Other Studies
Additional diagnostic studies are occasionally required preoperatively. If careful neurologic examination documents motor or sensory abnormalities of the peripheral nerves to the upper extremity, electromyography and nerve conduction evaluation are helpful. This allows documentation of nerve function or dysfunction and allows for preoperative discussion about the surgical management and the expected results of treatment.
If the history provided by the patient and the physical examination of the patient raises the question of infection, aspiration of the elbow and hematologic evaluation including complete blood count with differential, erythrocyte sedimentation rate (ESR), and C-reactive protein level should be performed. A negative infection workup does not completely rule out infection. If the index of suspicion for infection is high, intraoperative cultures and frozen section may aid decision making.
SURGICAL INDICATIONS
The indications for total elbow arthroplasty have changed dramatically over the past decade. The success of total elbow arthroplasty as a primary and secondary reconstructive procedure has resulted in its application to more demanding pathologies (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11). The expansion of the indication for total elbow arthroplasty has grown out of the limitations of other reconstructive procedures that have proved less reliable. The options for the surgical management in patients with dysfunctional instability include open reduction and internal fixation for nonunion of the distal humerus (12, 13, 14, 15), resection arthroplasty, arthrodesis (16), allograft reconstruction (12,17, 18, 19), or total elbow arthroplasty (2,20,15,21,22).
The primary indication for total elbow arthroplasty is instability that precludes useful function of the arm because of inability to position the hand in space. The typical patient is older than 60 years of age with low functional demands. However, younger patients willing to cooperate with the activity restrictions can be considered for total elbow arthroplasty. Pain is a variable complaint in patients with dysfunctional instability but tends to be mild to moderate in nature and rarely is the primary indication for surgery.
There are few absolute contraindications for total elbow arthroplasty for dysfunctional instability of the elbow. Active infection is an absolute contraindication for joint replacement. A history of previous infection is a relative contraindication to joint replacement. It is critical that the infection is completely eradicated prior to undertaking joint replacement. The ability of the patient to cooperate is critical, particularly in young, active patients. These patients are at risk for mechanical failure of the implant because of demanding work and recreational activities.
Nonoperative Treatment
External bracing of the extremity is an option in those patients that choose nonoperative management or are not appropriate surgical candidates. External bracing may provide a sense of stability to the patient. However, the benefit of braces is limited because re-creating an anatomically accurate axis of rotation that provides stability and mobility is not possible.
Braces are difficult to fit and do not stay affixed to the elbow with daily use, particularly in a large extremity. They are generally poorly tolerated as a permanent treatment for dysfunctional instability.
Implant Choices
The choice of implants is critical to the success of treatment. Unlinked, resurfacing implants rely on the integrity of the native bone and surrounding soft tissues for stability. Because patients with dysfunctional instability have deficiency of the distal humerus, these implants have no place in this clinical circumstance.
Linked, semi-constrained implants provide stability through the coupled articulation of the ulnar and humeral components. All implants are primarily fixed to bone by cementing the implants into the humerus and ulna. Secondary fixation on the humerus is achieved through medial and lateral fins in the supracondylar region or an anterior flange. These design features minimize the rotational and posteriorly directed forces across the elbow.
Distal humeral bone stock is absent or resected in all patients with dysfunctional instability. Bone loss up to the level of the olecranon fossa compromises the medial and lateral supracondylar columns limiting the utility of implants that obtain secondary stability through the supracondylar columns. Implants that use an anterior flange maintain their ability to counteract forces across the elbow because they achieve fixation against the anterior aspect of the humerus above the supracondylar level.
The position of the humeral yoke distal to the level of humeral insertion restores the distal level of the axis of flexion even with bone loss up to the level of the roof of the olecranon fossa (Fig. 28-2). Shortening of the humerus up to 2 cm proximal to the olecranon fossa is permitted, eliminating the need for custom implants (23,24). Bone loss greater than 2 cm can be managed with an implant with an extended anterior humeral flange (Fig. 28-3). This allows the humeral length to be reestablished while still providing the stabilizing effect of the anterior flange in preventing the forces that tend to rotate and displace the implant posteriorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree