Precollision Risk Factors, Illness-Related Cognition, and Recovery After Acute Whiplash Trauma
Tina Birgitte Wisbech Carstensen
Lisbeth Frostholm
Persistent pain and disability after whiplash trauma has become an increasingly significant problem in many industrialized countries as it has comprehensive individual as well as social costs in terms of the patients’ impaired physiological, psychological, economic, and domestic conditions [3, 22]. Of course, those consequences are prevalent in most chronic illnesses. The curious thing about WAD is that the above-mentioned pervasive consequences arise from a relatively minor impact. No dose-response relationship between trauma intensity and subsequent disablement has been shown, and several studies now point to collision severity being of minor importance [3, 6, 17]. Theoretically, cervical sprain (acute whiplash trauma) heals approximately within the same time frame as an ankle sprain, but a substantial proportion of the whiplash-exposed continue to experience symptoms [20].
This gives rise to an interesting question: Why is the impact substantial for some individuals, leaving them with persistent symptoms and disability, whereas for others, it is merely an experience of transient pain? Most acute whiplash-exposed do recover within the first
3 months, and after this time, the recovery rates level off [19]. Despite an exponential increase in research on whiplash during the last sixty years, we still miss substantial pieces of the puzzle.
3 months, and after this time, the recovery rates level off [19]. Despite an exponential increase in research on whiplash during the last sixty years, we still miss substantial pieces of the puzzle.
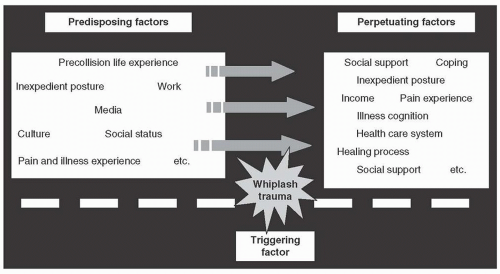
There is strong evidence to suggest that people’s self-rated health and psychosocial factors influence morbidity and mortality independent of biomedical disease parameters [9]. In whiplash research, a biopsychosocial model was introduced in the 1990s by Ferrari and Russell [11]1. Up till then, consequences of the whiplash trauma on the neck (muscles, skeleton, ligaments, etc.) had primarily been seen as the cause of persistent symptoms. The biopsychosocial approach presents several physiological factors (acute neck sprain, inexpedient posture as a reaction to pain, etc.) as the basis for the development of symptoms after whiplash trauma. Ferrari et al. [10], stressed that physiological factors may be viewed as the base on which the psychological factors operate, and physiological factors may elicit the psychological factors, for example, perception of symptoms and reactions to pain (coping strategies), and these reactions can be maladaptive or adaptive. However, there is an ever growing awareness that biopsychosocial interrelationships are much more complicated.
Broadly speaking, the factors involved in developing chronic WAD can be classified into predisposing, triggering, or perpetuating factors
(Fig. 13-1). According to this model, the individual enters the motor vehicle collision as a person from a certain culture, having accumulated experience with health and illness that might leave the individual at risk for developing persistent pain. The whiplash trauma may trigger certain vulnerability factors and interact together with social, psychological, and physiological perpetuating factors after the accident in the course of developing persistent pain after whiplash trauma.
(Fig. 13-1). According to this model, the individual enters the motor vehicle collision as a person from a certain culture, having accumulated experience with health and illness that might leave the individual at risk for developing persistent pain. The whiplash trauma may trigger certain vulnerability factors and interact together with social, psychological, and physiological perpetuating factors after the accident in the course of developing persistent pain after whiplash trauma.
Most research within whiplash has focused on collision-related factors and factors after the collision. Recently, researchers have started to look into factors before the accident to explore predisposing factors that influence recovery. It has been suggested that physiological and psychological vulnerability before the accident may to some extent explain the varied response to acute whiplash trauma [21, 22].
Precollision Social Risk Factors
Only a few studies have explored precollision social factors as risk factors for poor recovery following whiplash trauma. In 2008, a
meta-analysis and a best evidence synthesis concluded that no scientifically admissible studies exploring the effect of social factors on the onset of persistent symptoms following whiplash trauma existed [17, 19]. One of the few social factors that have been studied is the impact of education on recovery. However, these findings are heterogeneous. Some reviews conclude that low education is associated with negative outcome [26], and other reviews present no association or diverging results on associations with recovery [3, 8]. The impact of other precollision socioeconomic factors has been explored. Some studies suggest that unemployment [6] and low family income [16] increase the risk of poor recovery, while other studies find no association between poor recovery and prior earnings [22].
meta-analysis and a best evidence synthesis concluded that no scientifically admissible studies exploring the effect of social factors on the onset of persistent symptoms following whiplash trauma existed [17, 19]. One of the few social factors that have been studied is the impact of education on recovery. However, these findings are heterogeneous. Some reviews conclude that low education is associated with negative outcome [26], and other reviews present no association or diverging results on associations with recovery [3, 8]. The impact of other precollision socioeconomic factors has been explored. Some studies suggest that unemployment [6] and low family income [16] increase the risk of poor recovery, while other studies find no association between poor recovery and prior earnings [22].
Only two studies have explored the impact of receiving welfare benefits before the whiplash trauma, for example, sick pay and disability pension. Myrtveit et al. [24] retrieved self-reported data on welfare benefits and the latter from a national register on welfare benefits. They found that short-term health-related benefits increased the risk of chronic neck pain by 65%, while long-term health-related benefits and unemployment benefits did not predict recovery [24]. We found that receiving accumulated sickness benefit of 12 weeks or more during a five-year period before the accident was associated with both negative change in provisional situation OR (CI) = 3.8 (2.1;7.1) and considerable neck pain OR (CI) = 3.3 (1.8;6.3) 1 year after the accident [5]. Receiving unemployment benefit and social assistance within the last 5 years before the accident did not predict future negative change in provisional situation or neck pain [5]. These findings suggest that receiving short-term health-related benefits as sick pay before the collision is an important risk factor for poor recovery following whiplash trauma regardless of data being self-rated or obtained from other sources.
Precollision Psychological Risk Factors
A range of studies have examined the association between precollision psychological distress (e.g., previous psychological problems, anxiety, depression, psychiatric factors) and recovery [8, 21], and reviews state
that results are inconclusive [27]. The focus, however, has been on single specific psychological dimensions or disorders (e.g., anxiety or depression), and only a few studies have explored accumulated precollision psychological distress. We found that experiencing accumulated psychological distress before the collision predicted poor recovery 1 year after the collision OR (CI) = 2.1 (1.1;4.2) [6]. Surprisingly, poor recovery was predicted solely if distress was accumulated of several psychological distress factors. Most of the individuals experiencing accumulated distress showed symptoms of more than five out of seven psychological problems (anxiety, depression, hostility, obsessive compulsive disorder, somatization, emotional psychiatric disorder, illness worry). 11.4% ( n = 84) of this cohort of persons with acute whiplash had precollision accumulated psychological distress. However, accumulated psychological distress was only found to predict future neck pain and did not affect work capability 1 year after the accident. Psychological distress before the collision might be a predisposing factor for poor recovery, in particular accumulation of psychological distress, but these findings have to be replicated and explored in other cohorts of patients with whiplash.
that results are inconclusive [27]. The focus, however, has been on single specific psychological dimensions or disorders (e.g., anxiety or depression), and only a few studies have explored accumulated precollision psychological distress. We found that experiencing accumulated psychological distress before the collision predicted poor recovery 1 year after the collision OR (CI) = 2.1 (1.1;4.2) [6]. Surprisingly, poor recovery was predicted solely if distress was accumulated of several psychological distress factors. Most of the individuals experiencing accumulated distress showed symptoms of more than five out of seven psychological problems (anxiety, depression, hostility, obsessive compulsive disorder, somatization, emotional psychiatric disorder, illness worry). 11.4% ( n = 84) of this cohort of persons with acute whiplash had precollision accumulated psychological distress. However, accumulated psychological distress was only found to predict future neck pain and did not affect work capability 1 year after the accident. Psychological distress before the collision might be a predisposing factor for poor recovery, in particular accumulation of psychological distress, but these findings have to be replicated and explored in other cohorts of patients with whiplash.
Precollision Physiological Risk Factors
With respect to precollision physiological factors, research has indicated that some of the strongest associations with poor recovery are factors that are present before the accident, for example, back pain [21], neck pain [1, 6, 26], unspecified pain [1, 6], self-rated poor general health [1, 16, 24], high frequency of attendance to general practitioner [1, 21], high use of health care [22, 24], and use of medications [24]. High levels of physical fitness before the collision have been shown to be a protecting factor [14, 24]. It can be disputed whether, for example, pain and use of medical care can be seen as physiological factors, as there is substantial psychology involved in these issues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree