Abstract
Objective
The main objective of this study was to describe the distribution of referrals offered to patients assessed in the “Post-Acute Stroke program” of Bordeaux University Hospital (France). This program was developed in 2008 to organize the dispensation of care in rehabilitation units specialized in neurological diseases.
Material and methods
This was a single-centre observational study. Between July 2008 and December 2012, data on the number of stroke patients hospitalized at the Bordeaux University Hospital and their post-acute referral were collected from the local hospital discharge database. Some of these patients were assessed by Physical Rehabilitation and Medicine physicians participating in the program. Proposed and actual referrals, time from admission to assessment and functional status were also collected.
Results
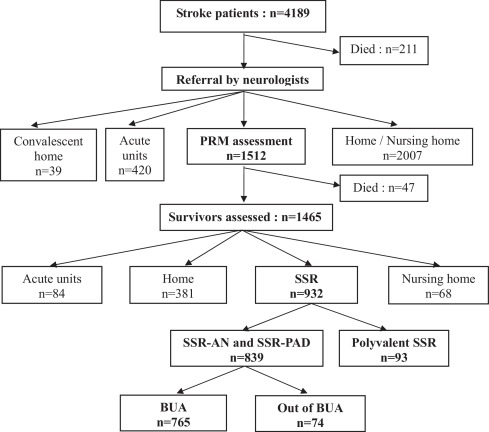
Among 4189 stroke patients, 1465 (35%) survivors were assessed, of whom 932 (22.2%) were discharged to inpatient rehabilitation facilities. There were no patients discharged to this type of unit without an assessment. Among the 1465 patients who were assessed, 57.2% were referred to specialized rehabilitation units, 6.3% were discharged to non-specialized rehabilitation units and 26% returned home directly. The median total length of stay in acute units varied from 10 to 15 days depending on referral orientation.
Conclusion
Patients that were assessed were more likely to be transferred to specialized rehabilitation units than to non-specialized rehabilitation units. The Post-Acute Stroke program has the particularity of combining private and public specialized rehabilitation units in a common collaborative referral system while retaining the control and flexibility of personalised referral for each patient in the light of local care availability.
1
Introduction
The incidence of strokes has increased markedly with the ageing of the population . Organisation of care provision for stroke patients has become a major challenge. Emphasis is placed in particular on the need to organise communication between the different elements in the care provision chain in order to ensure fluidity . In France, the “Plan d’actions national accidents vasculaires cérébraux 2010–2014” (national stroke programme) has promoted a regional organisation of care provision intended to cover all regions. In fact, the organisation of care provision varies considerably from one region to another .
Furthermore, it has been shown that specialised rehabilitation implemented at an early stage significantly improves autonomy and quality-of-life for stroke patients . In some countries, Stroke Units based on definitions agreed upon by the Stroke Unit Trialists’ Collaboration combine acute care and rehabilitation in one and the same place. In France, the system is organised differently and requires the transfer of patients from short-stay (acute) facilities to follow-up care and rehabilitation facilities (Soins de suite et réadaptation, hereafter SSR), when the condition of the patient requires it. Since the reorganisation of SSR facilities via the decrees and enforcement of 2008, patients can be oriented either to specialised SSR establishments, typically for nervous system damage or for dependent elderly, or else to non-specialised or polyvalent SSR facilities .
The French academic societies have developed recommendations to assist clinicians in the task of referring stroke patients to the most suitable facility. Criteria were defined in a national expert conference in Mulhouse in 2008, and more recently an optimum care itinerary for stroke patients was proposed by SOFMER (Société français de médecine physique et de réadaptation) .
Thus far, the studies performed at national level have merely shown that only a third of the patients were referred to SSR facilities after the acute phase of a stroke, and that among these the majority was taken into care in polyvalent facilities that were not specialised in damage to the nervous system . Few studies have looked at post-acute stroke care provision on a local scale in the different territories across France .
In July 2008 a common programme specific to referral of stroke victims was set up at Bordeaux University Hospital (CHU) to improve the fluidity of access to care. The “Post-Acute Stroke” programme was intended to develop coordination among structures upstream (short-stay units) and downstream (SSR facilities), and to harmonise secondary care provision for these patients in the different specialised SSR facilities in the Bordeaux urban area (known as Bordeaux-Métropole since January 2015). There are 28 municipalities in the Bordeaux urban area. The main objective of the present study was to describe the distribution of the different types of referral offered to patients assessed within this programme. The secondary objective was to describe the clinical and functional characteristics of patients that were referred to specialised SSR facilities, and their outcomes.
2
Materials and methods
2.1
Type of study
The study was observational, descriptive and single-centred. It was performed using two types of database: the PMSI databases (Programme de médicalisation des systèmes d’information) for short-stay hospitalisations in Bordeaux CHU, and the computerised follow-up database of the Post-Acute Stroke programme.
2.2
Study population
Patients consecutively hospitalised in a short-stay facility in the clinical neuroscience pole of Bordeaux CHU between July 2nd 2008 and December 12th 2012 were included in the study, provided they met the following inclusion criterion: a main diagnosis of stroke, whether ischaemic or haemorrhagic.
2.3
Patient referral process in the Post-Acute Stroke programme
2.3.1
Assessment by neurologists
All patients hospitalised in Bordeaux CHU for a stroke in the acute phase are provided for in the different short-stay (acute) units in the neuroscience pole. Among these units, a neurovascular unit was created in 2008. It is specifically dedicated to the management of strokes and comprises an intensive care sector. An initial selection for referral of patients at discharge from short-stay units is performed by the neurologists. Within the collaboration organised with the SSR facilities, the neurologists have been fully informed of the referral criteria produced by the experts in the Mulhouse conference . Using these criteria the neurologists can decide:
- •
either to orient patients directly to a return home (with paramedical care in the community), or to refer them to a long-stay care facility (Unité de soins de longue-durée [USLD]) or to a facility for the dependent elderly (Établissement d’hébergement pour personnes âgées dépendantes [EHPAD]);
- •
or to offer an assessment within the Post-Acute Stroke programme with a view to transfer to a SSR unit.
2.3.2
Assessment by physical and rehabilitation medicine specialists
Three SSR units in the Bordeaux urban area specialised in damage to the nervous system (SSR-AN) collaborate with the Post-Acute Stroke programme: one unit in Bordeaux CHU, one private SSR-AN facility with recognition for public usefulness (an ESPIC), and one private, profit-making SSR-AN. One CHU unit specialised in the care of the dependant elderly (SSR-PAD) with a wing devoted to stroke patients, also participates.
Physical and rehabilitation medicine (PRM) specialists working in these SSR units take turns once a week to attend the clinical neuroscience pole in Bordeaux CHU to assess patients pre-selected by neurologists in each unit.
These physicians assess deficits and limitations in activity in collaboration with paramedical staff in the units concerned, in particular occupational therapists. They also meet patients’ families and social workers.
A common referral form is used, comprising information on the patient (medical history, social environment), the medical assessment (deficits, limitations in activity) and a proposed orientation–transfer to a specialised SSR, transfer to a non-specialised SSR, return home or transfer to an institution (EHPAD–nursing home–or USLD–long-stay facility). If referral to a specialised SSR is considered, the choice of the facility (one or several proposals per patient) takes into account the particular characteristics and specific mandate of each facility, the choice of the patient and his/her family, and also the recommendations for care provision after a stroke . When the patient’s condition requires it, a new assessment is suggested at the next PRM physician visit. The physician performing the assessment circulates the assessment forms to all the specialised SSR units taking part in the programme. If required, they can also be circulated to other SSR units, depending on the patient’s place of residence. Within 24 hours, the SSR units approached undertake to confirm whether or not they can take on the patient and circulate this information to the applicant and to the other specialised SSR units in the programme.
2.4
Collated data
2.4.1
PMSI data
Using the PMSI database for hospitalisations in short-stay facilities in Bordeaux CHU, we searched for patients hospitalised with stroke as the main established diagnosis, ischaemic or haemorrhagic, between July 2nd 2008 and December 12th 2012. We used ICM-10 codes to classify them, and recorded age, gender, and length of stay, and the distribution of referrals at discharge.
2.4.2
Assessment forms and computerised medical files
Using the PRM evaluation forms collected between July 2nd 2008 and December 12th 2012 and the corresponding computerised medical files, the elements collated were as follows: the facility making the application, age and gender of the patient, the date of occurrence of the stroke, the date when the patient was assessed by the PRM physician, the type of stroke (ischaemic or haemorrhagic), deficits presented by the patient (left/right hemiplegia, cerebellar syndrome, unilateral neglect syndrome, aphasia, swallowing difficulties, sphincter disturbances), initial NIHSS score (National Institute of Health Stroke Scale), place of residence before the stroke (either home, single or with a partner, or in an institution), the length of stay in the short-stay facility, the orientation offered, and the actual destination, Barthel’s index at admission to and at discharge from specialised SSR units, length of stay, and destination at discharge from specialised SSR units: home, geriatric institution (EHPAD, USLD), other hospital or medico-social facility.
2.5
Statistical analyses
Descriptive analyses for quantitative values were expressed as mean (± standard deviation, and median with interquartile interval [quartile 1; quartile 3]. Patient characteristics were compared using the Chi 2 test for qualitative variables and variance analysis for the quantitative variables. A logistic regression multivariate analysis was performed to study independent factors associated with hospitalisation in specialised SSR units. Results were considered statistically significant when P < 0.05. The statistical analyses were performed on Statistica 7.1 (StatSoft ® ).
2
Materials and methods
2.1
Type of study
The study was observational, descriptive and single-centred. It was performed using two types of database: the PMSI databases (Programme de médicalisation des systèmes d’information) for short-stay hospitalisations in Bordeaux CHU, and the computerised follow-up database of the Post-Acute Stroke programme.
2.2
Study population
Patients consecutively hospitalised in a short-stay facility in the clinical neuroscience pole of Bordeaux CHU between July 2nd 2008 and December 12th 2012 were included in the study, provided they met the following inclusion criterion: a main diagnosis of stroke, whether ischaemic or haemorrhagic.
2.3
Patient referral process in the Post-Acute Stroke programme
2.3.1
Assessment by neurologists
All patients hospitalised in Bordeaux CHU for a stroke in the acute phase are provided for in the different short-stay (acute) units in the neuroscience pole. Among these units, a neurovascular unit was created in 2008. It is specifically dedicated to the management of strokes and comprises an intensive care sector. An initial selection for referral of patients at discharge from short-stay units is performed by the neurologists. Within the collaboration organised with the SSR facilities, the neurologists have been fully informed of the referral criteria produced by the experts in the Mulhouse conference . Using these criteria the neurologists can decide:
- •
either to orient patients directly to a return home (with paramedical care in the community), or to refer them to a long-stay care facility (Unité de soins de longue-durée [USLD]) or to a facility for the dependent elderly (Établissement d’hébergement pour personnes âgées dépendantes [EHPAD]);
- •
or to offer an assessment within the Post-Acute Stroke programme with a view to transfer to a SSR unit.
2.3.2
Assessment by physical and rehabilitation medicine specialists
Three SSR units in the Bordeaux urban area specialised in damage to the nervous system (SSR-AN) collaborate with the Post-Acute Stroke programme: one unit in Bordeaux CHU, one private SSR-AN facility with recognition for public usefulness (an ESPIC), and one private, profit-making SSR-AN. One CHU unit specialised in the care of the dependant elderly (SSR-PAD) with a wing devoted to stroke patients, also participates.
Physical and rehabilitation medicine (PRM) specialists working in these SSR units take turns once a week to attend the clinical neuroscience pole in Bordeaux CHU to assess patients pre-selected by neurologists in each unit.
These physicians assess deficits and limitations in activity in collaboration with paramedical staff in the units concerned, in particular occupational therapists. They also meet patients’ families and social workers.
A common referral form is used, comprising information on the patient (medical history, social environment), the medical assessment (deficits, limitations in activity) and a proposed orientation–transfer to a specialised SSR, transfer to a non-specialised SSR, return home or transfer to an institution (EHPAD–nursing home–or USLD–long-stay facility). If referral to a specialised SSR is considered, the choice of the facility (one or several proposals per patient) takes into account the particular characteristics and specific mandate of each facility, the choice of the patient and his/her family, and also the recommendations for care provision after a stroke . When the patient’s condition requires it, a new assessment is suggested at the next PRM physician visit. The physician performing the assessment circulates the assessment forms to all the specialised SSR units taking part in the programme. If required, they can also be circulated to other SSR units, depending on the patient’s place of residence. Within 24 hours, the SSR units approached undertake to confirm whether or not they can take on the patient and circulate this information to the applicant and to the other specialised SSR units in the programme.
2.4
Collated data
2.4.1
PMSI data
Using the PMSI database for hospitalisations in short-stay facilities in Bordeaux CHU, we searched for patients hospitalised with stroke as the main established diagnosis, ischaemic or haemorrhagic, between July 2nd 2008 and December 12th 2012. We used ICM-10 codes to classify them, and recorded age, gender, and length of stay, and the distribution of referrals at discharge.
2.4.2
Assessment forms and computerised medical files
Using the PRM evaluation forms collected between July 2nd 2008 and December 12th 2012 and the corresponding computerised medical files, the elements collated were as follows: the facility making the application, age and gender of the patient, the date of occurrence of the stroke, the date when the patient was assessed by the PRM physician, the type of stroke (ischaemic or haemorrhagic), deficits presented by the patient (left/right hemiplegia, cerebellar syndrome, unilateral neglect syndrome, aphasia, swallowing difficulties, sphincter disturbances), initial NIHSS score (National Institute of Health Stroke Scale), place of residence before the stroke (either home, single or with a partner, or in an institution), the length of stay in the short-stay facility, the orientation offered, and the actual destination, Barthel’s index at admission to and at discharge from specialised SSR units, length of stay, and destination at discharge from specialised SSR units: home, geriatric institution (EHPAD, USLD), other hospital or medico-social facility.
2.5
Statistical analyses
Descriptive analyses for quantitative values were expressed as mean (± standard deviation, and median with interquartile interval [quartile 1; quartile 3]. Patient characteristics were compared using the Chi 2 test for qualitative variables and variance analysis for the quantitative variables. A logistic regression multivariate analysis was performed to study independent factors associated with hospitalisation in specialised SSR units. Results were considered statistically significant when P < 0.05. The statistical analyses were performed on Statistica 7.1 (StatSoft ® ).
3
Results
3.1
General characteristics of the cohort and referral post short-stay
Over the period of 54 months, 4189 patients with a main diagnosis of stroke (PMSI data) were hospitalised in Bordeaux CHU. Men accounted for 57.8%. Mean age was 65.8 ± 14.1 for men and 70.6 ± 15.6 for women. The mean duration of short-stay hospitalisation was 22.7 ± 14.2 days. Among these 4189 patients, 211 (5%) died during their initial hospitalisation, and 2466 patients (58.9%) were directly oriented by neurologists on discharge from neurology department. Most of these went directly home, or returned to their usual institution. The other 1512 patients (36.1%) all underwent a PRM assessment within the Post-Acute Stroke referral programme, performed on request from neurologists ( Fig. 1 ).
Among these 1512 patients assessed, the majority were men (57.4%). Median age was younger in men than in women, respectively 67 years [58;76] and 76 years [66;82] ( P < 0.001). The stroke was diagnosed as ischaemic for 1242 patients (82.2%), haemorrhagic for 264 (17.4%), and indeterminate for 6 (0.4%). The mean initial NIHSS score ( n = 770) was 11.1 ± 7.2 (median = 10 [5;17]).
The request for evaluation originated for 77.8% from the neurovascular unit (NVU) ( n = 1176), and 336 requests were from two other units in the clinical neuroscience pole of Bordeaux CHU. The time lapse between the stroke occurrence and the PRM assessment was on average 8.5 ± 13.6 days (median 6 days [4;9]. Forty-seven of the patients assessed died before leaving the short-stay unit.
Among the 1465 surviving assessed patients, orientation towards a specialised SSR was offered for 69.8% ( n = 1023), in 91.5% of cases after the first assessment and in 8.5% ( n = 87) after re-assessment. Finally, 57.2% were actually admitted to this type of facility, most of them to one of the 4 specialised SSR units taking part in the Post-Acute Stroke programme ( Fig. 1 ). The second most frequent orientation was a return home with care provision in the community for 26%. Only 6.3% of the patients were transferred to polyvalent (non-specialised) SSR units, and 4.6% to an EHPAD facility (nursing home). There were no patients transferred to a USLD (long-stay) facility.
The mean time lapse to transfer to a specialised SSR unit in the Bordeaux urban area following the assessment was 7 days [5;12], and the proportions of patients distributed across the 4 specialised SSR units were equivalent. The median duration in short-stay units ranged from 10 days [6;17] for a return home to 36.5 days [24.5;57] for transfer to an EHPAD facility. The mean time lapse was 14 days [11;20] for a transfer to specialised SSR, and 15 days for a transfer to polyvalent SSR [11;19].
Thus, for the 4189 patients hospitalised in Bordeaux CHU for stroke in the period concerned, 22.2% were referred to a SSR facility, of whom 90% were referred to a specialised SSR unit and 10% to a polyvalent SSR unit. All patients admitted to SSR facilities underwent prior PRM assessment within the Post-Acute Stroke programme ( Fig. 1 ).
3.2
Characteristics of the patients assessed in the Post-Acute Stroke programme according to their referral destination on discharge from short-stay unit
Patients who went directly home on discharge from short-stay unit and those transferred to polyvalent SSR units had lower NIHSS scores, and were less likely to have sustained a haemorrhagic stroke, less likely to exhibit motor deficit in both upper and lower limbs, and to exhibit hemispatial neglect, swallowing or sphincter difficulties, than patients transferred to specialised SSR units ( Table 1 ). Alongside, motor deficit in both upper and lower limbs, aphasia, swallowing and sphincter disturbances were more frequent in patients transferred to EHPAD facilities. Median age was older, and the proportion of women greater among patients transferred to SSR-PAD, polyvalent SSR or EHPAD. The proportion of patients who had been living alone at home before the stroke was smaller among patients transferred to specialised SSR (AN [neurological] or PAD [dependent elderly]).






