Essentials of Diagnosis
- Subacute onset of constitutional complaints (eg, fever, weight loss, malaise, arthralgias), lower extremity nodules and ulcerations, mononeuritis multiplex, and intestinal angina (postprandial pain caused by the involvement of mesenteric vessels).
- Cutaneous polyarteritis nodosa (PAN) is a variant of the systemic disease in which vasculitis is limited to the skin, usually presenting as nodules that break down into ulcers.
- Angiogram or biopsy of an involved organ required for diagnosis.
- Angiography may reveal microaneurysms in the kidneys or gastrointestinal tract.
- Biopsies of the skin and peripheral nerves (with sampling of the adjacent muscle) are the least invasive ways of confirming the diagnosis histopathologically.
General Considerations
Classic PAN is characterized by necrotizing inflammation of muscular arterioles and medium-sized arteries that spares the smallest blood vessels (eg, capillaries). PAN is not associated with glomerulonephritis, although it can cause renovascular hypertension and renal infarctions through its involvement of the medium-sized intrarenal vasculature. Features that distinguish PAN from other forms of systemic vasculitis are confinement of the disease to the arterial as opposed to the venous circulation, the sparing of the lung, and the absence of granulomatous inflammation.
Reported annual incidence rates of PAN range from 2 to 9 cases per million people per year. A higher incidence (77 cases/million) was reported in an Alaskan area hyperendemic for hepatitis B virus (HBV). With the availability of the HBV vaccine, however, the percentage of cases associated with HBV has declined substantially (now <10% of all cases in the developed world). PAN appears to affect men and women with approximately equal frequencies and to occur in all ethnic groups.
Clinical Findings
PAN can involve virtually any organ system with the exception of the lungs. The disease demonstrates a predilection for certain organs, particularly the skin, peripheral nerves, gastrointestinal tract, and kidneys. A nearly universal complaint among patients is some type of pain, caused by myalgias, arthritis, peripheral nerve infarction, testicular ischemia, or mesenteric vasculitis.
Fevers are a common feature of PAN. The characteristics of the fever vary substantially among patients, ranging from periods of low-grade temperature elevation to spiking febrile episodes accompanied by chills (patterns of low-grade fever are more common than are hectic fevers). Tachycardia with or without fever may be another feature of PAN. Malaise, weight loss, and myalgias are also common.
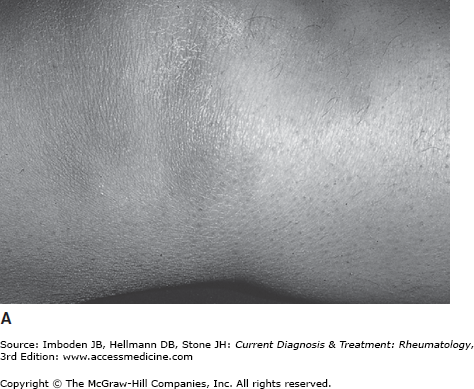
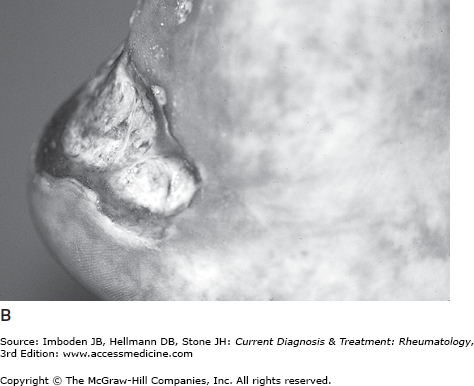
Vasculitis of medium-size arteries may produce several types of skin lesions. These cutaneous findings include livedo racemosa (Plate 48), nodules, papules, ulcerations, and digital ischemia leading to gangrene. All of these findings or combinations of them may occur in the same patient. The livedo racemosa (often termed “livedo reticularis”), which may have a diffuse distribution over the extremities and buttocks, does not blanch with the application of pressure to the skin. Nodules, papules, and ulcers tend to occur on the lower extremities, particularly near the malleoli, in the fleshy parts of the calf, and over the dorsal surfaces of the feet. Nodules frequently evolve into ulcerations that have scalloped borders (Figure 35–1) and heal with scarring.
Figure 35–1.
Cutaneous manifestations of polyarteritis nodosa. A: A nodular lesion. B: An ulcer with scalloped borders. (Reproduced, with permission, from Stone JH, Nousari HC. Essential cutaneous vasculitis: what every rheumatologist should know about vasculitis of the skin. Curr Opin Rheumatol. 2001 Jan;13(1):23–34.)
Although the principal skin manifestations relate to disease caused by arteritis in medium-sized muscular arteries and arterioles, crops of purpura (caused by the involvement of smaller blood vessels) occur in a minority of patients. Digital ischemia, often accompanied by splinter hemorrhages, sometimes leads to tissue loss.
Arthralgias of large joints (knees, ankles, elbows, wrists) occur in up to 50% of patients; however, true synovitis is seen in substantially fewer patients.
Mononeuritis multiplex, the infarction of named nerves by inflammation in the vasa nervorum, occurs in approximately 60% of patients with PAN. The most commonly involved nerves are the sural, peroneal, radial, and ulnar. Vasculitic neuropathy tends to involve the longest (ie, distal) nerves first and usually begins asymmetrically. Thus, the first motor symptoms of vasculitic neuropathy may be a foot or wrist drop (resulting from infarctions of the peroneal and radial nerves, respectively). In advanced stages, the neuropathy may mimic a confluent, symmetric polyneuropathy. Careful history taking, however, may unmask its initial asymmetry. Both sensory and motor findings are characteristic of vasculitic neuropathy because with the exception of the sural nerve (a pure sensory nerve), peripheral nerves typically have mixed sensory and motor fibers bundled within the same nerve.
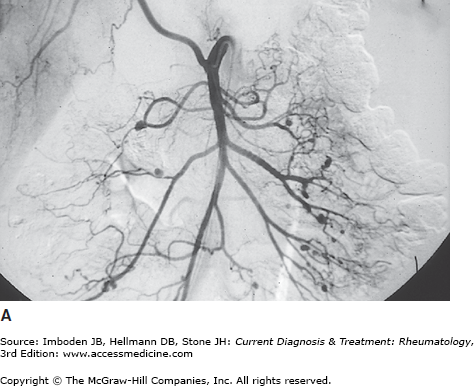
The gastrointestinal manifestations of PAN occur in approximately half of all patients and are among the most challenging symptoms to diagnose correctly because of their nonspecific nature. Postprandial abdominal pain (“intestinal angina”) is common. Involvement of the mesenteric arteries in PAN may lead to the disastrous complications of mesenteric infarction or aneurysmal rupture, each of which is associated with a high mortality rate. Angiography of the mesenteric vessels reveals multiple microaneurysms (Figure 35–2A). These range in size from lesions that are barely visible to the naked eye to several centimeters in diameter. Sometimes PAN is detected at cholecystectomy or appendectomy in the absence of other disease manifestations. In such cases, surgical removal of the involved organ may be curative.
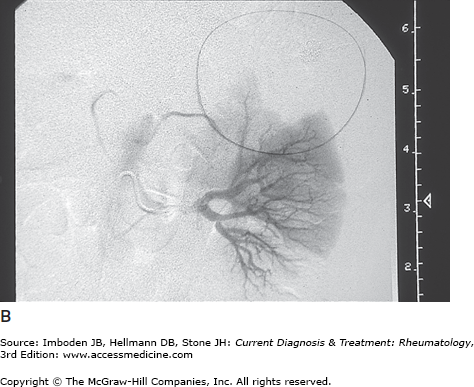
This major feature of PAN is found in 40% of patients. The inflammatory process targets the renal and interlobar arteries (the medium-sized, muscular arteries within the kidney) and occasionally also involves the smaller arcuate and interlobular arteries. Angiography may reveal microaneurysms within the kidney or large, wedge-shaped renal infarctions (Figure 35–2B). Renal artery involvement or involvement of intra-renal arterioles in PAN may lead to renin-mediated hypertension. Red blood cell casts on urinalysis imply glomerulonephritis and thus usually implicate another disease (eg, microscopic polyangiitis). However, both proteinuria and hematuria may be observed in PAN.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree