Abstract
Introduction
Polio survivors in France are estimated at 50,000. This study aimed at describing their needs from their clinical and vocational conditions.
Method
A retrospective study of our physical and rehabilitation medicine (PRM) consultation activity.
Results
One hundred and fifteen women/85 men, with a mean age of 51 years ± 14.3 (17 to 82). Paralysis involved only one lower limb in 108 patients, the two lower limbs in 56 patients and only one upper limb in 4. At the time of the first consultation 137 patients had experienced functional worsening. The complaints were pain (105 subjects), fatigue (59) and new paresis (58). Only 25% had retired. Post-polio syndrome criteria were present in 46 subjects (23%). Patients who had contracted poliomyelitis in France (56%) differed from the other subjects with regard to age (58.4 versus 41.5), professional status and frequency of PPS (30.9% versus 12.6%).
Conclusion
These polio survivors were not particularly aged and they had often experienced functional worsening. The evolution of their disease shall represent a public health issue over the decades to come.
Résumé
Introduction
Le nombre de personnes vivant avec des séquelles de poliomyélite en France peut être estimé à 50 000. Cette étude avait pour but de décrire l’état clinique et le statut professionnel de ces personnes.
Méthode
Étude rétrospective d’une première consultation en médecine physique et de réadaptation.
Résultats
Cent quinze femmes/85 hommes, moyenne d’âge 51 ans ± 14,3 (17–82 ans). Les paralysies touchaient un seul membre inférieur chez 108 patients, les deux membres inférieurs chez 56 patients et un seul membre supérieur chez 4 patients. Cent trente-sept patients se plaignaient de dégradation fonctionnelle, de douleurs (105 sujets), de fatigue (59) et d’aggravation de parésies existantes (58) ; 25 % seulement étaient retraités. Les critères d’un syndrome post-poliomyélitique (SPP) étaient présents chez 46 sujets (23 %). Selon que la poliomyélite avait été contractée en France ou hors France, il y avait des différences concernant l’âge (58,4 versus 41,5), le statut professionnel et la fréquence du (SPP) (30,9 % versus 12,4 %).
Conclusion
Cette population de patients n’est pas particulièrement âgée, mais une dégradation fonctionnelle est très souvent exprimée. L’évolution des déficiences et de leurs conséquences constitue une question de santé publique pour les décennies à venir.
1
English version
1.1
Introduction
People living with the sequels of poliomyelitis often experience new difficulties related to the ageing process and/or actual post-polio syndrome (PPS). Numerous studies have been devoted to these symptoms . Nevertheless, the problems encountered by these subjects often fail to be recognized or are underestimated by medical teams and health authorities. There exists a need, particularly in France, to better define and anticipate public health needs over the coming years, but the exact number of persons involved remains unknown, and can only be roughly estimated from different sources.
The eradication of poliomyelitis throughout the world could not be completed, as WHO had hoped, by 2000, and there have even been new cases reported since the turn of the century (1352 in 2010, 223 in 2012) in Nigeria, Afghanistan and Pakistan . On the other hand, in June 2002 the WHO European region was declared polio-free. In France since 1949, information is drawn from a national register for mandatorily declared new cases. From 1949 to 1961, around 1500 cases were declared each year, with peaks in 1955 (1834), 1957 (4109) and 1959 (2566), followed by a gradual decrease from 1961 until the last reported case in 1989 . All in all, 28,468 cases were declared (personal communication by Dr Antona from the French national health institute InVS). Over the same period 3251 deaths directly due to poliomyelitis were declared. Vaccination has been compulsory since 1964.
The total number of polio survivors throughout the world has been estimated by the WHO at 20 million . As concerns Europe, the European Polio Union estimates the number of survivors at 700,000 . In France an estimate of 55,000 is generally given, but no national register exists. The only definite number is that of patients registered by the French national health insurance organ for salaried workers (Caisse Nationale d’Assurance Maladie des Travailleurs Salariés [CNAMTS]) as being impaired by post-polio sequelae and consequently having the right to reimbursement of expenses for treatments connected with these sequelae: 12,906 in 2010 ( , and personal communication by Dr Gissot from the CNAMTS). While 85% of the French population (65.436 million) fall under the responsibility of the CNAMTS, a considerable number of polio survivors are clearly not registered therein.
In order to more precisely describe the clinical and vocational status of subjects having consulted in our physical and rehabilitation medicine (PRM) unit, we have endeavoured to provide precise indications of their deficiencies (paralysis and orthopaedic deformations), complaints (weakness, pain, fatigue), activity limitations (ambulation) and vocational conditions. Attention has also been focused on any differences with regard to the place where poliomyelitis was contracted and to the modalities of primary care.
1.2
Method
This is a retrospective study of all the records of patients having consulted from 2002 to 2011 in our PRM department. The main pathologies prompting the consultations were systematically registered (stroke, head trauma, poliomyelitis…) and the population we have described represents close to the totality of the population involved. With a specially constructed grid for data recording, one of us (CA) reviewed the original files of the patients who had presented themselves on account of polio sequelae and were given a long and particularly attentive consultation. The grid had been designed (AY, CA) so as to record the information pertaining to the initial infection (age, where it was contracted, site of paralysis, surgical treatments and orthotic appliances) and also information gathered during the initial consultation in our unit (age, height, weight, vocational status, reason for consultation, key complaints such as new paresis, fatigue, pains and functional worsening, paralytic impairments, orthopaedic deformations, capacity and means of ambulation, associated diagnoses, prescriptions for complementary tests, treatments, rehabilitation and appliances). Only a few files failed to contain sufficient information and were not included in the analysis. Data analysis consisted exclusively in calculation of the number of participants and standard deviation of the means.
1.3
Results
Two hundred and seventeen files of polio survivors were examined but only 200 provided enough information to be analysed.
1.3.1
Characteristics of the population
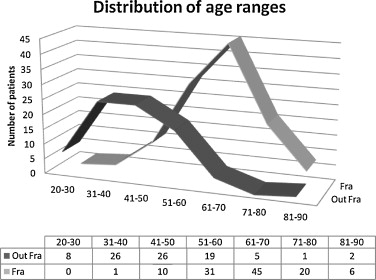
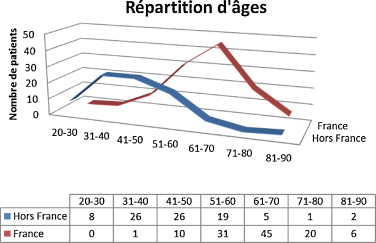
One hundred and fifteen women/85 men, with a mean age of 51 years ± 14.3 (17 to 82), 35% under 50 years ( Fig. 1 ). Their mean height was 165 cm ± 9.6 (1.45–1.97) and the mean body mass index (BMI) was 25 ± 4.6 (14.9 to 43).
1.3.2
Reasons for the consultation
One hundred and thirty-seven patients experienced functional worsening and/or pain, 58 wanted advice and 5 patients came mainly because they had encountered social difficulties. Forty-six patients (22%) were referred by a general practitioner, 39 (19.5%) being referred by a specialist and 115 having come on their own; 147 patients (73.5%) had never consulted any PRM specialist, 53 had consulted such a specialist but wished to make a change or were seeking another opinion.
1.3.3
Information with regard to the initial phase of poliomyelitis
1.3.3.1
Place where poliomyelitis was contracted
One hundred and thirteen in France (56%), 87 elsewhere (44%) including 32 in North Africa.
1.3.3.2
Age
The disease was contracted at under 1 year by 29 patients (14%), during the 2nd year by 51 (25%), during the 3rd year by 22 (11%), during the 4th and 5th years by 36 (18%), during the 6th and 7th years by 32 (16%), between the 8th and 10th years by 14 (7%), during and after the 10th year by 16 (8%).
1.3.3.3
Site of paralyses
The right lower limb was affected in 141 patients, the left lower limb in 131, the right upper limb in 37, the left upper limb in 33, the spinal muscles in 37, the abdominal muscles in 19 and the respiratory muscles in 10.
1.3.3.4
Surgery
Ninety-eight patients had undergone surgery at least once. Surgery had consisted in: 25 lower limb osteotomies, 20 lower limb lengthening, 63 ankle arthrodesis, 26 muscular transfers including 3 in the upper limb, 14 Achilles’ tendon lengthening, 9 osteosynthesis for scoliosis, 5 tenotomies.
1.3.3.5
Orthotic appliances
Eighty-six patients had been given orthopedic shoes, orthesis and/or orthopedic corset. Ten patients could not walk and were using a wheelchair.
1.3.4
Clinical status at the time of the first consultation
1.3.4.1
Deficiencies
The paralyses of which note was taken did not necessarily correspond to the initially reported medical conditions; while some had apparently regressed, others had remained unknown.
1.3.4.1.1
Paralysis
Only one lower limb was paralyzed in 108 patients (64 right, 44 left), only one upper limb in 4 (1 right, 3 left), the two lower limbs were affected in 56 patients, one lower limb and one upper in 9; the 2 upper limbs in 3; the 2 upper and one lower in 3; the 2 lower and one upper in 10; the four limbs in 7. The paralysis involved the right lower limb (141 patients), the left lower limb (116 patients), the right upper limb (27 patients), the left upper limb (22 patients), the spinal muscles (10 patients) and the abdominal muscles (35 patients).
1.3.4.1.2
Orthopedic deformations
The orthopedic deformations of the lower limbs observed were: leg length inequality in 106 subjects with a mean disparity of 3.6 cm; genu recurvatum (28 subjects, 11.1° mean); genu flessum (41, 11.7°); ankle equinus (36, 15.9°); ankle varus (6); hip flessum (12). Among the 16 patients with an initial scoliosis treated by orthopedic corset, only 10 still had a scoliosis necessitating clinical monitoring because of pain or respiratory disorders.
1.3.4.1.3
Complaints
Even in cases where the first reason for consultation was not pain or functional worsening, questioning of the patient revealed a number of physical disorders: pain in 105 patients (52%), fatigue in 59 (29%), and new muscle weakness in 58 (29%). The three main symptoms, fatigue, pain and weakness, were present together in 20 patients. Pain was present in 85 other subjects, isolated (53), associated with fatigue (18) or associated with weakness (14). Pain involved the upper or lower limbs in 102 (51%) subjects including 9 cases pertaining to identified overloaded shoulder and 40 cases of coxarthrosis and/or osteoarthritis. Forty subjects presented with chronic isolated low back pain and 9 with lumbar radicular pain. Fatigue was present in 39 other subjects: isolated (9 subjects), associated with pain (18) or associated with weakness (12). New muscle weakness or aggravated paresis was observed in 38 other subjects, whether isolated (12 subjects), associated with pain (14) or associated with fatigue (12). Walking worsening was reported by 87 (43.5%) subjects and cold intolerance by 3. A diagnosis of PPS based on the existence of at least one new muscle weakness after an indeterminate interval of more than 15 years and 2 added symptoms was put forward in 46 subjects (23%).
1.3.4.2
Activities
Ninety subjects (45%) were able to walk without orthesis or device, 32 (16%) walked with an assistive device alone (usually crutches), 39 (19.5%) needed orthesis alone and 22 (11%) needed both orthesis and crutches. Nine could not walk at all and were wheelchair-dependent, 8 used orthesis and crutches for indoor walking and a wheelchair outside.
1.3.4.3
Professional status
Complete information was available in only 176 files. Most of the patients were still active: 86 (48.9%) subjects were still at work, 12 (6.8%) were engaged in adult vocational training, 27 (15.3%) were unemployed, 7 (4%) were on sick leave and only 44 (25%) had retired.
1.3.4.4
Characteristics according to patient origin
According to the place where poliomyelitis was contracted, in France versus outside of France, they did not markedly differ with regard to initial treatments undergone. But at the time of the consultation, the 113 patients who had caught poliomyelitis in France differed from the other 87 with regard to: age (58.4 ± 10.2 versus 41.5 ± 12.5); professional status since there were more retirees in the first group (35% versus 7%) and more unemployed in the second group (9% versus 24.7%); frequency of post-polio syndrome (30.9% versus 12.6%).
1.3.4.5
Prescriptions
Only the prescriptions arising from the initial consultation were taken into account and they are not indicative of prescriptions taken as a whole, many of which were issued at a later date. A specific medical treatment (pyridostigmine, immunoglobulins) without analgesics or anti-inflammatory drugs was prescribed for only 3 patients. The requested complementary examinations included: biological check-up for 108 patients, bone x-rays for 85, MRI for 9, electromyography for 9, polysomnography for 9 and functional breathing tests for 11. Fifty patients (25%) walking without equipment were offered new equipment (orthesis, orthopedic shoes and/or corset) and for 36 patients the existing equipment was renewed. Rehabilitation essentially consisting in physiotherapy was prescribed for 106 (53%) subjects, surgical advice was requested for 29 (14.5%), specialized dietetic advice requested for 20 (10%) and a social worker was called in 30 cases (15%).
1.4
Discussion
This study was aimed at describing the needs of polio survivors in France through the experience of a consultation in a PRM department, focusing attention on their deficiencies, complaints, activity limitations, vocational condition and on differences that may have been related to the place where poliomyelitis was contracted. The results draw attention to the severity of the paralysis, the frequency of orthopedic surgery during their early years, the frequency of the main complaints such as new muscle weakness, fatigue and pain, and the consequences on ambulation.
The population is relatively young, 61% of the patients being under 60; since their health exigencies are likely to evolve, they warrant further investigation. The increasing number of new patients consulting over the last 10 years highlights an increasingly serious public health problem, which is related not only to the ageing of polio survivors and but also to the influx of a new, migratory population. In fact, it clearly appears that our population may be divided into two distinct groups. The first is composed of subjects having contracted poliomyelitis in France. In this group, fear of PPS was quite frequently the main reason for consulting. The second group is younger, composed of migrant subjects who had contracted poliomyelitis in their native countries. Regarding their professional status, in the first group 35% were retired and a small number were unemployed (9%) while in the second group only 7% were retired and 24.7% were unemployed.
The complaints of polio survivors have been described at length in other studies, and the most effective therapeutic approaches have been indicated . The usual symptoms are functional worsening, muscle weakness, physical or overall fatigue, and pain in the muscles and joints. Some of them may be related to ageing or to other disorders, but the question of a specific post-polio syndrome (PPS) remains to be investigated. The criteria for the diagnosis of PPS associate a prior episode of poliomyelitis confirmed by patient history, clinical examination and typical EMG findings, a period of partial or complete neurological recovery, an extended interval of neurological and functional stability lasting over 15 years, a gradual or sudden onset of new muscle weakness; other signs such as general fatigue, muscle and joint pain, cold intolerance or amyotrophy may also be present .
In our population, 23% of the subjects fulfilled the diagnosis of PPS, a rather low percentage in comparison with the literature, where it ranges from 20% to 31% , 36% and even 52% . This is probably due to the relatively young age of our subjects. In the one published study in France, which was conducted in 1993, 77% among the 248 who replied to a questionnaire reported deterioration in terms of functional loss, especially during walking and exertion, but the existence of a problem such as a specific “post-polio syndrome” remained open to discussion . The European Polio Union recently proposed a somewhat less restrictive definition, basing diagnosis on the existence of at least 2 of these symptoms, muscle weakness being non-mandatory .
That said, polio survivors who do not fulfil the diagnostic criteria for PPS may still have substantial loss of motor function requiring care . Muscle weakness is the cardinal symptom, as strength deteriorates among polio survivors at an accelerated rate, in the upper as well in the lower limbs regardless of age , and it has been a cause for complaint in 29% of our patients. Fatigue is also a common, severe and multidimensional complaint occasioned by physical and psychological factors , and it was present in 30% of our subjects. Moreover, it would appear that fatigued post-polio patients may be considered as a sub-group among patients with PPS, with recent studies having shown that fatigue among these patients is not related to age and that the time elapsed after onset of their initial polio is of shorter duration than in other PPS subjects . Pain is also one of the more common complaints, involving over 50% of PPS subjects and reported by 51% of our patients. The corpulence often observed in our population is likewise a major problem since it entails heightened fatigability and walking difficulties. In addition, psychological aspects call for consideration , given the fact that in fatigued subjects, mental fatigue has greater impact on vitality than physical fatigue . An association in these patients of fatigue and sleep-disordered breathing syndrome has been observed . Furthermore, subjects with polio sequels show pronouncedly higher mortality and morbidity than the general population . To summarize, even though the needs of polio survivors cannot be comprehensively described in the framework of our retrospective study, the recorded complaints and the frequency of prescription of a first orthotic appliance — along with physical therapy, surgery consultation and recourse to a social worker — are illustrative of the present and future requirements of the subjects.
In France, only at the end of the 1990s were treatments related to late consequences of poliomyelitis officially recognized as giving the right to total reimbursement by national health insurance of the medical expenses incurred by salaried workers. There nonetheless still exist localities in which polio survivors may have difficulties finding a physician or physiotherapist familiar with their issues and questions. Different factors produce and reinforce widespread ignorance among medical teams along with public officials and insurance companies as to the repercussions of poliomyelitis sequelae. The first has to do with the eradication of poliomyelitis in Europe; as a result, both medical professionals and the general public may tend to feel that the poliomyelitis question is settled, and are consequently largely unaware of the problems faced by those living with poliomyelitis sequelae. Future doctors are no longer trained in poliomyelitis, and many of today’s practicing physicians have never carried out a thorough examination of a polio survivor. Another factor is that polio survivors were “supposed” to manage their lives as successfully as healthy people, and are used to trying to meet these expectations; moreover, they don’t necessarily look different, and their handicap is relatively “invisible”. As for more severely impaired survivors, their negative memories of the long years spent in hospitals where they were treated and schooled induce them to indefinitely postpone and even avoid consulting a neurologist or PRM specialist for many years, until the functional worsening leaves them with no choice but to do so .
The results presented in this study have no more than indicative value, its main weakness consisting in its retrospective design. Following previous works on the subject, it underscores the deferred functional and professional consequences of poliomyelitis that need to be better known by the medical community so that suitable care may be provided by PRM teams . It would be important to determine the exact number of subjects involved, but this information is not easy to ascertain. Based on the number of declared polio cases since 1945 and on the aforementioned migratory movements, a plausible estimate in France might be 50,000. In conclusion, and notwithstanding the impact of the hoped-for eradication of acute poliomyelitis, the long-term sequelae of this disease are sure to constitute a major public health issue over the coming decades. Comprehensive description of the biopsychosocial conditions of polio survivors will require further and more extensive multiprofessional investigations.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Les personnes vivant avec des séquelles de poliomyélite ressentent le plus souvent de nouvelles difficultés liées à l’âge ou à un réel syndrome post-poliomyélite (SPP). De nombreuses études ont été consacrées à ces symptômes . Néanmoins, ces nouvelles difficultés sont souvent sous-estimées ou non reconnues par le milieu médical et les autorités administratives. Il y a besoin, particulièrement en France, de mieux définir et d’anticiper les besoins de santé publique pour les années à venir mais le nombre exact de personnes concernées est inconnu et ne peut être qu’estimé à partir de différentes sources.
L’éradication de la poliomyélite à travers le monde n’a pas pu être achevée comme l’avait espéré l’OMS en l’an 2000 et il y a toujours de nouveaux cas rapportés depuis le début du XXI e siècle (1352 en 2010, 223 en 2012), au Nigéria, Afghanistan et Pakistan . En Europe, la région a été déclarée indemne de nouvelle poliomyélite en juin 2002. En France les connaissances sont basées sur le registre national de déclaration obligatoire des nouveaux cas existants depuis 1949. Entre 1949 et 1961, 1500 cas/an ont été déclarés en moyenne, avec des pics importants en 1955 (1834), 1957 (4109) et 1959 (2566), suivis par une diminution progressive depuis 1961, date d’introduction de la vaccination orale, jusqu’au dernier cas rapporté en 1989 . Au total, ce sont 28 468 cas qui ont été déclarés (communication personnelle par le Dr Antona de l’Institut national de la veille sanitaire [INVS]). Sur la même période 3251 décès directement liés à la poliomyélite ont été déclarés. La vaccination a été rendue obligatoire en 1964.
Le nombre total de personnes survivant avec des séquelles de poliomyélite à travers le monde a été estimé par l’OMS à 20 millions . L’European Polio Union estime à 700 000 le nombre de survivants en Europe . En France, leur nombre est estimé généralement à 55 000 mais il n’y a pas de registre national. Le seul nombre précis de personnes concernées est celui enregistré par la Caisse nationale d’assurance maladie des travailleurs salariés (CNAMTS) comme bénéficiant d’une prise en charge pour une affection de longue durée au titre des séquelles de poliomyélite : 12 906 en 2010 ( , et communication personnelle par le Dr Gissot de la CNAMTS). Attendu que 85 % de la population française (65 436 000) relèvent de la responsabilité de la CNAMTS, il y a manifestement un grand nombre de survivants de poliomyélite non déclarés à cet organisme.
Cette étude a été conduite pour tenter de mieux décrire les conditions cliniques et professionnelles de personnes ayant consulté dans notre service de médecine physique et de réadaptation (MPR) en décrivant précisément leurs déficiences (paralysies et déformations orthopédiques), leurs plaintes (faiblesse musculaire, douleurs, fatigue) et limitations d’activité (marche) et les conditions professionnelles. Les éventuelles différences liées au lieu de contraction de la poliomyélite et des premiers soins ont également été étudiées.
2.2
Méthode
Il s’agit d’une étude rétrospective de tous les dossiers de patients ayant consulté dans notre service entre 2002 et 2011. Les principales pathologies motivant les consultations étant systématiquement enregistrées (accident vasculaire cérébral, traumatisme crânien, poliomyélite…), la population décrite ici est très proche de l’exhaustivité de cette consultation. À l’aide d’une grille spécialement construite, l’un d’entre nous (CA) a revu tous les dossiers originaux des patients qui ont consulté dans le cadre des séquelles de poliomyélite ayant été l’objet d’une longue consultation attentive. La grille avait été conçue (AY, CA) pour consigner les informations concernant l’atteinte initiale (âge, lieu de contraction, siège des paralysies, traitements chirurgicaux et appareillages) et celles recueillies lors de la première consultation dans notre service (âge, taille, poids, statut professionnel, motif, plaintes principales notamment nouvelle paralysie, fatigue, douleurs et dégradation fonctionnelle, atteintes paralytiques, déformations orthopédiques, capacité et mode de déambulation, diagnostics associés, prescriptions d’examens complémentaires, traitements, rééducation et appareillages). Les quelques dossiers qui ne contenaient pas assez d’information concernant le statut clinique n’ont pas été retenus pour l’analyse. L’analyse des données a comporté uniquement des calculs d’effectifs et de moyenne avec écarts types.
2.3
Résultats
Deux cent dix-sept dossiers ont été examinés mais seulement 200 contenaient toutes les informations pour être analysés.
2.3.1
Caractéristiques de la population
Cent quinze femmes/85 hommes, avec une moyenne d’âge de 51 ans ± 14,3 (17 à 82), 35 % ayant moins de 50 ans ( Fig. 1 ). La taille des sujets était en moyenne de 165 cm ± 9,6 (1,45 à 1,97) et l’indice de masse corporel (IMC) était de 25 ± 4,6 (14,9 à 43).