Abstract
Objectives
Sciatica is a common disease; between 13% and 40% of the general population will experience at least one episode of sciatica due to spinal disc herniation and nerve root irritation. In some specialist centres, percutaneous intradiscal techniques can be applied as an intermediate measure between conservative treatment and surgery, with a view to avoiding the adverse events associated with surgical discectomy. Discogel ® is a percutaneously implanted medical device for the treatment of lumbar sciatica due to a herniated disc. We performed an open, prospective, observational study in order to (a) determine whether the prior use of air disc manometry could limit the risk of nerve root irritation reportedly associated with nucleolysis and administration of Discogel ® and (b) investigate the technique’s efficacy and safety.
Method
A total of 79 Discogel ® -treated patients were systematically reviewed. A nurse anaesthetist evaluated each patient’s pain levels during the procedure itself. The therapist assessed the patient on inclusion and 8 weeks after the Discogel ® procedure. A third assessment was based on a telephone interview (by an independent assessor) at least 4 months after the procedure.
Results
Pain levels immediately after the Discogel ® procedure (1.7 ± 2.0) were markedly lower than before the procedure (5.5 ± 2.3). There were no complications. Two months after Discogel ® administration, the initial pain level had fallen by an average of 74 ± 34%. The outcome was quite stable over time (mean follow-up: 8 months). At the end of the follow-up period, 60.7% of the patients were free of pain, 76% considered the treatment outcome to be good or very good, 74% had returned to work and 76% would recommend the treatment to a friend.
Conclusion
The favourable outcomes associated with the procedure should now be confirmed in a controlled trial.
Résumé
Objectifs
Entre 13 % et 40 % de la population générale présenteront au cours de leur vie un épisode de sciatique par conflit disco-radiculaire. Dans quelques centres spécialisés, les techniques percutanées intra-discales sont proposées. Leur objectif est de réduire les effets secondaires liés à la discectomie. Le Discogel ® est un dispositif médical intra-discal utilisé dans ce contexte pour sécuriser davantage la procédure thérapeutique. Nous avons conduit une étude prospective observationnelle sur une série de 79 patients traités consécutivement : (a) pour observer la capacité d’une disco-manométrie aérique à réduire le risque d’irritation radiculaire décrit lors des nucléolyses et de l’utilisation du Discogel ® (b) pour examiner l’efficacité et la tolérance de ce dispositif.
Patients et méthode
Un suivi systématique a été effectué chez les 79 premiers patients traités par Discogel ® dans notre centre. Une infirmière anesthésiste procédait aux évaluations de la douleur en période périopératoire. Ces données étaient complétées par une évaluation clinique à huit semaines et téléphonique à plus de quatre mois.
Résultats
Le suivi périopératoire montre des intensités douloureuses moyennes qui diminuent rapidement (5,5 ± 2,3 en préopératoire, 1,7 ± 2,0 en postopératoire immédiat) et l’absence de complications. La douleur a diminué de 74 ± 34 % deux mois après la procédure d’injection du Discogel ® . Au terme de l’évaluation, 60,7 % des patients sont asymptomatiques, 76 % considèrent le traitement comme efficace, 74 % retrouvent leurs activités professionnelles et 76 % recommanderaient ce traitement à des proches.
Conclusion
Cette procédure et ces résultats méritent d’être confirmés lors d’une étude contrôlée.
1
English version
1.1
Introduction
Sciatica is a common condition; between 13% and 40% of the general population will experience at least one episode of sciatica due to nerve root irritation at some point in their life. The annual incidence of this condition ranges from 1% to 5%, depending on the study in question . A review of the literature shows that the pain levels associated with sciatica do not decrease over the long-term (5 years) – regardless of whether the patient has been treated or not. The treatment goals are therefore limited to relieving all the symptoms in the short- to mid-term and reducing functional disability in the mid- to long-term . In fact, this is a rather ambitious objective because it seeks to help patients to maintain their professional activity and avoid periods of time off work caused by pain.
At present, there is a hierarchy of treatments for sciatica caused by nerve root irritation as a result of disc herniation; oral treatments may be followed by the spinal infiltration of corticoids, which in turn may be followed by surgery. In certain specialist centres, percutaneous intradiscal techniques (nucleolysis and nucleotomy) can be used after conservative treatment and as an alternative to surgery. These developments are driven by the need for techniques that are less aggressive than discectomy; in sciatica, positive outcomes for discectomy are often compromised by chronic, invalidating, lower back pain and the occurrence of serious postoperative complications . Nucleolysis is defined as the injection of compounds into the middle of the intervertebral disc, with a view to dissolving all or part of the nucleus pulposus. Nucleotomy is defined as the creation of a small cavity within the nucleus pulposus by physical means, such as intradiscal needle aspiration and laser or radiofrequency vaporization. These percutaneous techniques are based on the same supposed principle of action; by destroying or reducing the volume of the nucleus pulposus, they tend to limit the nerve root irritation induced by compression of the nucleus pulposus and its suffusion through the annulus fibrosus . In the 1970s, chemopapain was the first substance to be used in disc nucleolysis. This is the only percutaneous technique to have been validated by a sufficient number of controlled studies . Even though chemopapain has now been withdrawn from the market, it is still considered as the reference technique. Researchers have since investigated a number of other options . In nucleolysis, the risk of radiculitis (related to epidural leakage of the injected product) is a constant concern . Theron et al. have reported several cases of radiculitis (with the occurrence of a burning sensation) during the intradiscal injection of rectified spirit . With a view to limiting the risk of diffusion outside the disc, a viscous gel containing ethylcellulose and tungsten radiopaque suspended in 95% ethanol has been developed . This gel has been approved as a percutaneously administered, CE-marked implantable device (Discogel ® ) for the treatment of lumbar sciatica caused by a herniated disc. According to the product information sheet, Discogel ® has two mechanisms of action. It combines a chemical effect (in which the rectified spirit causes local necrosis of the nucleus pulposus) with a mechanical effect that may be related to the ethylcellulose’s hydrophilic properties (via dehydration of the turgescent, protruding disc).
The tungsten-containing gel can be visualized radiographically. Even when the injection is fluoroscopically guided, leakage is always possible and, indeed, has been reported during vertebroplasty with radiopaque cement . Theron et al. have reported cases of resurgent pain during injection, although he did not specify the number of cases or the intensity of the pain . In fact, Theron et al. suggested that the pain was related to the injection speed . This type of painful episode relates to distension of the disc, which can be revealed by discography . However, when the lumbar or radicular pain occurs during the intradiscal injection of a product that is possibly toxic for the nerve roots, it is difficult to rule our epidural leakage if the disc’s renitence has not been checked beforehand. In theory, discography could be used to check the disc’s renitence a few days before the injection, although this type of procedure would make the treatment more burdensome and would probably increase the risk of infection. On the other hand, intradiscal injection of contrast agent prior to injection of Discogel ® appears to be poorly compatible in terms of the limited disc volume and dilution of the subsequently injected Discogel ® . Furthermore, this procedure appears to be poorly effective because it does not prevent the occurrence of benign radiculitis in 3.7% of cases and severe neurological complications in 0.45% of nucleolysis procedures .
Given this context, we performed an open, observational study designed to:
- •
test the ability of an air discography procedure to limit the risks of epidural leakage;
- •
establish the efficacy and safety of Discogel ® injection by a second medical team.
1.2
Method
1.2.1
Study population
Patients were followed up as part of their routine medical care, which was provided in our department in most cases. A total of 79 consecutive patients met the inclusion criteria, i.e. an indication for the treatment of lumbar sciatica via the percutaneous injection of Discogel ® .
1.2.2
Eligibility criteria
Inclusion criteria:
- •
lumbar sciatica due to nerve root irritation;
- •
onset at least 8 weeks previously;
- •
lack of response to optimal medical treatment;
- •
at least two epidural injections, including at least one under fluoroscopic guidance.
Exclusion criteria:
- •
the presence of herniation with the extrusion or migration of disc material;
- •
observation of markedly narrow pinched intervertebral discs on CT or MRI.
1.2.3
Procedures and techniques
The procedures were performed with neurosedation during day hospitalization in a day surgery service. Using a posterior-lateral approach on the painful body side, an 18-gauge needle (length: 10 cm) was introduced under fluoroscopic guidance. This needle was used as a conduit for the disc puncture. The disc was then punctured with a finer needle (22-gauge, 15 cm in length), the tip of which was located in the centre of the intervertebral disc (as checked by frontal and lateral fluoroscopy). In order to increase the procedure’s safety and efficacy and check the disc’s renitence, filtered air discography was performed with a 10 mL syringe and a bacterial filter. The disc’s renitence was considered to be satisfactory if:
- •
resistance to injection was felt before 10 mL of air had been injected;
- •
the syringe’s piston recoiled by at least two graduations once finger pressure had been released.
Next, in accordance with Discogel ® ’s recommendations for use, 0.7 mL of gel was injected slowly (0.1 mL every 30 seconds, under fluoroscopic guidance). Once the injection had been completed, the needle’s inner shaft guide was put back in place and the needle was left in position for 2 minutes (in order to limit the risk of leakage at the time of removal).
The patients were monitored for 3 hours immediately after the procedure, while the effects of neurosedation dissipated. The patients left hospital with a prescription for a week’s course of anti-inflammatories and analgesics. They were told not to remain seated for long periods. As is generally the case for surgical discectomy procedures, 6 weeks of sick leave were always prescribed. However, the patients were told that they could return to work after 3 weeks if they felt able to do so.
1.2.4
Efficacy criteria
In order to evaluate the percutaneous procedure, we first assessed immediate perioperative pain. A nurse anaesthetist surveyed overall perioperative and immediate postoperative pain levels in the patients. The pain intensity was rated verbally on a numeric scale from 0 (no pain) to 10 (the worst pain imaginable). The pain was rated three times during the procedure and then once an hour during the 3-hour monitoring period in the recovery room.
In a second step, we assessed the change in pain levels over time. In the first 66 patients treated, a nurse anaesthetist evaluated overall pain levels by means of a telephone survey one week after the injection. Furthermore, the physician evaluated the intensity of lumbar and radicular pain during consultations at inclusion and 8 weeks after the injection. A third evaluation (a telephone survey) was performed by an independent assessor at least 4 months after the procedure. Again, the intensities of lumbar and radicular pain were rated verbally on a scale of 0 (no pain) to 10 (the worst pain imaginable). The patients were also invited to reply to the following three questions:
- •
How would you now describe the treatment outcome: very good, good, average or poor?
- •
Did the treatment enable you to resume your previous professional activities?
- •
Would you recommend this treatment to a friend or family member with the same problem ?
1.3
Results
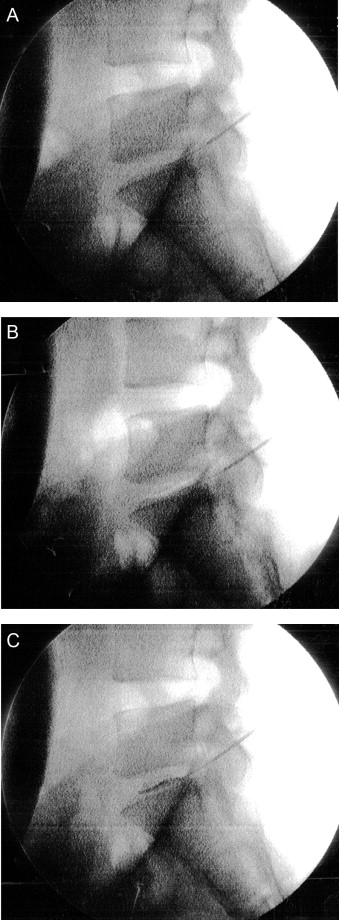
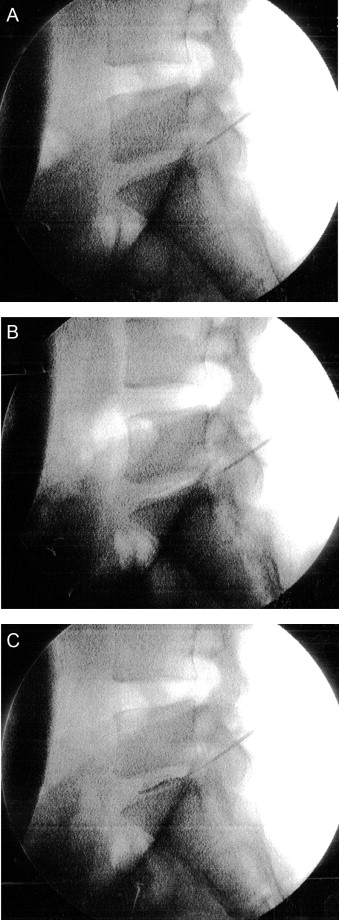
In all, 79 patients (40 women and 39 men; mean age: 40 ± 12 years) were included in the study. On average, they had been suffering from lumbar sciatica for 14 ± 12 months. The injected discs were L4-L5 in 40 patients, L5-S1 in 31 patients and at two sites in eight patients. Fig. 1 gives an illustrative example of a procedure with an L5-S1 disc: disc puncture ( Fig. 1 A), discography through air injection ( Fig. 1 B) and disc opacification induced by injection of Discogel ® ( Fig. 1 C) into the intradiscal air space. The air discography procedure prompted the discovery of a non-renitent disc in two patients (3.7%) and thus Discogel ® was not injected in these cases. The change in perioperative pain over time is described in Table 1 . For the 79 treated patients as a whole, the mean perioperative and immediate postoperative pain levels were significantly lower than the mean preoperative level ( P < 0.0001). During the perioperative period, overall pain levels increased in five patients (by 1 point in two patients and by 2 points in three patients). None of these occurrences prompted a change in the procedure. In the immediate postoperative period, three patients reported an increase pain levels (by 1 point in one patient, by 2 points in one patient and by 4 points in one patient). Again, none of the temporary increases in pain prompted a change in treatment. No sensory or motor impairments were reported during the immediate postoperative period.
| Preoperative pain | Perioperative pain | Immediate postoperative pain | After one week | |
|---|---|---|---|---|
| Overall pain level (mean ± standard deviation) | 5.2 ± 2.3 | 2.6 ± 2.5 a | 1.7 ± 2.0 a | 3.0 ± 1.9 a |
a A significant difference ( P < 0.0001) relative to the preoperative pain level.
The evaluation one week after the procedure revealed a significant decrease in the mean pain level, relative to the mean preoperative level ( P < 0.0001, Table 1 ). However, pain levels increased in four patients (by 1 point in one patient, by 2 points in two patients and by 4 points in one patient). None of these increases in pain required treatment other than that planned in the protocol.
Fifteen patients had undergone Discogel ® injection less than 4 months before collection of the data presented here and thus were not contacted by telephone following the clinical evaluation 8 weeks after the procedure. The other 64 patients were contacted by telephone after a mean (SD) time interval of 8.5 ± 4.5 months (D255). The intensities of nerve root pain and lumbar pain are reported in Table 2 ; both values fell significantly between D0 and D60 ( P < 0.0001) and between D0 and D255. We did not observe a statistically significant change in pain intensity between D60 and D255 ( P > 0.05). Two months after the Discogel ® administration, the mean reduction in the initial pain level was 74 ± 34%. Table 3 (giving the percentage of patients as a function of the degree of pain relief) shows that the results were relatively stable over the 8 months follow-up period. The variations observed during the follow-up period highlighted a tendency for:
- •
initially unsatisfactory outcomes to worsen;
- •
further improvement in patients reporting more than a 50% decrease in pain nerve root during the first 2 months.
| D0 ( n = 79) | D60 ( n = 79) | D255 ( n = 64) | |
|---|---|---|---|
| Nerve root pain | 6.7 ± 1.6 | 2.0 ± 2.5 a | 2.7 ± 3 a |
| Lower back pain | 6.6 ± 2.1 | 2.7 ± 2.5 a | 3.0 ± 3 a |
| Reduction in pain (relative to the initial level) | Percentage of patients in each class after 2 months ( n = 79) | Percentage of patients in each class at the time of the telephone follow-up ( n = 64) |
|---|---|---|
| 0% | 12.6 | 16.4 |
| 1–24% | 0 | 1.3 |
| 25–50% | 6.3 | 6.3 |
| 51–75% | 11.4 | 10.1 |
| 76–99% | 11.4 | 5.0 |
| 100% | 58.2 | 60.7 |
| Total | 100 | 100 |
Only three patients (3.7%) with extreme initial pain levels reported the resurgence of pain during long-term follow-up. At the end of the follow-up period, 60.7% of the patients no longer experienced any pain, 76% considered that the treatment outcome was good or very good ( Table 4 ), 74% had returned to work and 76% would have recommended the treatment to a friend. During follow-up, none of the patients reported the occurrence of sensory or motor impairments.
| The patient’s assessment | Percentage ( n = 64) |
|---|---|
| Poor | 17.7 |
| Average | 6.3 |
| Good | 12.6 |
| Very good | 63.2 |
| Total | 100 |
1.4
Discussion
Our study results emphasized the value of performing air discography prior to percutaneous disc treatments and confirmed the previously reported therapeutic value of Discogel ® in the treatment of sciatica . The air discography procedure prompted the discovery of a non-renitent disc in two cases (3.7%) and so the latter patients did not receive an injection of Discogel ® . No per- or post-procedural pain suggestive of nerve root damage or epidural leakage was observed and none of the Discogel ® injections had to be abandoned once initiated. In the present series, 3.7% of the injections were cancelled because of poor disc renitence. This value corresponds very closely to the proportion of patients with radiculitis reported during papain-based nucleolysis . This similarity suggests that our air discography procedure enabled us to prevent this type of complication from occurring.
For the five patients who reported the recrudescence of preoperative pain, the observed disc renitence and the preoperative aerogram suggested to us that the pain was related to disc distension ; we were therefore able to continue the Discogel ® injection without fear of epidural leakage. Only one patient reported lasting, resurgent pain in the postoperative period (with a 2 point increase that prompted the patient to rate the overall perioperative pain level as 10 out of 10). This extreme pain level was suggestive of radiculitis. Nevertheless, other data collected during follow-up argued against this diagnosis because no immediate change in treatment was required and the check-up after a week revealed a 50% pain decrease (relative to the initial pain level). Hence, in this case, there was a dissociation between the clinical presentation noted in the medical records and our evaluation. It would have been interesting to study the pain’s characteristics because discogenic pain is predominantly lumbar and radicular pain is mainly felt in the legs (i.e. along the nerve path) . Above all, this recrudescence of pain revealed the limitations of our procedure for gathering perioperative data; we had chosen to evaluate overall pain and thus simplify assessment of the patients during each step in the therapeutic procedure.
Discogel ® has much the same advantages and constraints as nucleolysis. However, according to the product information supplied with Discogel ® , its viscous, radiopaque nature reduces the risks of epidural leakage enough to be able to dispense with the discography that is generally recommended before nucleolysis . The absence of serious adverse events in published series appears to confirm the basis of this approach for avoiding serious neurological complications . However, the literature has also mentioned the occurrence of radiculitis linked to Discogel ® leakage .
Nucleolysis is generally less feasible when epidural leakage is discovered during discography with contrast agent. Hence, in this context (including the injection of Discogel ® ), disc manometry with filtered air appears to be able to limit both the risk of epidural leakage and the need to inject contrast agent – the use of which is likely of dilute the nucleolytic agent or delay the injection until the excess intradiscal pressure subsides.
In the present series, 75% of the outcomes were judged to be good or very good by the patients ( Table 4 ). The corresponding values reported by Theron et al. range from 82% to 91.4% (overall average: 89%) . Hence, in comparison, our results appear to be less good. This difference may be due to two parameters. Firstly, there were differences in the treatment procedures. Theron et al. evaluated the effect of a Discogel ® injection combined with a local corticoid injection at a posterior, epidural or foraminal site (chosen as a function of the patient’s symptoms and the imaging data). We did not use a local corticoid injection. Secondly, there were differences between the two sets of treated patients. In our series, the patients had been in pain for an average of 14 months; this is longer than the period of 6 to 8 months post-onset during which the relief of nerve root compression appears to be most effective . In contrast, patients in previously reported series were eligible for Discogel ® injection after just 3 months of nerve root pain.
The 75% reduction in pain reported by the patients treated here agrees well with the literature data. In fact, the reported efficacy of chemopapain ranged between 80% and 85% , although the techniques intended to replace chemopapain are associated with values nearer to 70% .
The extent of pain relief in our series appears to be lower than that reported in the surgical series . This difference may be due to the anatomy of the herniated disc treated in the respective studies. In principle, percutaneous techniques are only indicated for sciatica caused by a subligamentous herniated disc, which is known to be predictive of a poor prognosis in terms of both progression of the sciatica and responsiveness to treatment .
The creation of an intradiscal cavity (in order to decrease nerve root compression) is often cited as the mechanism of action of the percutaneous intradiscal techniques . In that case, and given that the disc is a compressible structure, how then can one imagine that resumption of a weight-bearing posture would not lead to the rapid (or even immediate) recurrence of pain? From a mechanical point of view, the achievement of sustained relief would require the destruction of all of the nucleus pulposus (as occurs with chemopapain); this would lead to pinching of the intervertebral disc . In contrast, the new percutaneous techniques are known not to induce narrowing of the intervertebral disc . One must therefore envisage a mechanism capable of sustainably reducing inflammatory reactions induced by contact between extruded nucleus pulposus and the nerve roots . This is one of the putative mechanisms of action in ozone-alcohol nucleolysis, which appears to be capable of reducing the production of nucleus pulposus and thus limiting its suffusion through the annulus fibrosus . However, the absence of an effect on the permeability of the annulus fibrosus exposes the patient to early relapses and creates the need for repeated injections . In our series, fewer than 5% of the patients suffered a long-term relapse after a single injection. These results are concordant with the relapse rates associated with thermal (vaporization) techniques . It has been suggested that the sustained efficacy of thermal techniques is related to heat-induced scarring of the annulus fibrosus and thus a reduction of the latter’s permeability to the nucleus pulposus . Studies of the CT-guided injection of Discogel ® suggest that viscous gel can migrate towards the herniated breaches and thus reduce the local porosity .
Hence, Discogel ® ’s efficacy appears to be based on two mechanisms of action:
- •
the immediate effect of alcohol-based nucleolysis on the nucleus pulposus;
- •
the longer-term sealing of the annulus fibrosus.
However, animal studies must now be performed in order to better understand the device’s mechanisms of action. Our ability to draw conclusions on the basis of our present results was limited by:
- •
the absence of a topographic pain analysis during the perioperative period (which would probably have enabled us to better differentiate between discogenic pain and nerve root pain);
- •
the absence of a control group (which would probably have enabled us to better evaluate the air discography’s impact on the occurrence of pain during administration and thus better assess Discogel ® ’s therapeutic effect).
1.5
Conclusion
Our present results emphasize the increased safety and ease of use associated with the performance of air discography prior to nucleolysis via Discogel ® injection. The long-term follow-up results (with a cure rate of 60.7%) are encouraging in terms of efficacy and safety and thus encourage us to perform a controlled study.
Disclosure of interest
The main author, Mathieu de Seze has a contract of advice (council) with the laboratories Mertz Pharma France which market the discogel in France.
None of the other authors has conflict of interest.
2
Version française
2.1
Introduction
La sciatique est une pathologie fréquente. Entre 13 % et 40 % des personnes présenteront au moins un épisode de sciatique par conflit disco-radiculaire durant leur vie. L’incidence annuelle correspondante est comprise entre 1 % et 5 % . La revue de la littérature médicale fait apparaître que l’évolution douloureuse des sciatiques est la même à long terme (cinq ans), que les patients aient bénéficiés ou non d’un traitement. L’objectif des traitements peut ainsi être limité à l’amélioration de l’ensemble des symptômes à court et à moyen terme et à réduire les incapacités fonctionnelles à moyen et à long terme . Il s’agit d’un objectif en réalité ambitieux car il est de nature à éviter la désinsertion professionnelle des patients, liée aux limitations d’activité induites par des périodes douloureuses trop longues.
Il existe actuellement une hiérarchie thérapeutique qui passe du traitement médical à la chirurgie en passant par les infiltrations rachidiennes de corticoïdes. Dans certains centres spécialisés les techniques percutanées intra-discales, nucléolyses et nucléotomies, prennent leur place entre les soins conservateurs et la chirurgie. Le développement de ces techniques repose sur la volonté de proposer des techniques moins ‘agressives’ que la discectomie chirurgicale dont le résultat positif sur la sciatique et souvent grevé par des lombalgies chroniques invalidantes et par la survenue de complications graves . Les nucléolyses sont définies par l’injection de substances chimiques au sein du disque intervertébral visant à dissoudre tout ou partie du nucléus pulposus. Les nucléotomies sont définies par la création d’une cavitation partielle au sein du nucleus pulposus par des moyens physiques telle que l’aspiration intra-discale ou la vaporisation du nucleus par une onde laser ou par radiofréquence. Ces techniques percutanées reposent sur le même principe d’action théorique : elles tendent, par la réduction du volume du nucleus pulposus et par sa dénaturation, à limiter l’irritation des racines nerveuses induite par la compression et les suffusions de nucleus pulposus au travers de l’annulus discal . La chemopapaïne fut la première substance utilisée pour réaliser des nucléolyses discales dans les années 1970. C’est la seule technique percutanée qui a bénéficié d’un nombre suffisant d’études contrôlées pour confirmer son intérêt . Malgré l’arrêt de sa commercialisation, elle est toujours considérée comme technique de référence. Les praticiens ont cherché des solutions alternatives nombreuses . En ce qui concerne les nucléolyses, le risque de radiculite liée à une fuite épidurale du produit injecté est un souci constant . Theron et al. ont rapporté quelques cas de radiculites lors d’injection intra-discale d’alcool à 95 %, se traduisant par la survenue de sensations de brûlures radiculaires intenses pendant l’injection de solution alcoolique à 95 % . Pour tenter de limiter les risques de diffusion extra-discale, il a proposé d’utiliser un gel composé d’éthyl-cellulose contenant de l’alcool à 95 % et une suspension de tungstène radio-opaque . Il s’agit depuis 2008 d’un dispositif implantable (Discogel ® ), mis en place par voie percutanée, qui a reçu une certification de conformité au marquage CE, proposé pour le traitement des lombosciatiques par hernie discale. Selon la notice d’utilisation, le mode d’action décrit est double. Il combine une action chimique induite par l’éthanol à 95 %, à l’origine d’une nécrose locale du nucleus pulposus , et une action d’ordre mécanique qui serait liée aux propriétés hydrophiles de l’éthyl-cellulose, via une déshydratation du disque turgescent et protubérant.
Ce gel est visualisable radiologiquement grâce à l’adjonction de tungstène en suspension. Cependant, malgré la visualisation du produit au cours de l’injection, une fuite demeure possible, comme cela a été rapporté lors des techniques de vertébroplasties utilisant des substances radio-opaques . Theron et al. rapportent des cas de recrudescence douloureuse durant l’injection sans en préciser le nombre et l’intensité . Il met ces douleurs en relation avec la vitesse de l’injection du produit . Le processus douloureux évoqué est ici est une distension discale comme cela se voit lors des discographies . Cependant, lorsque des douleurs lombaires ou radiculaires surviennent au cours de l’injection intra-discale d’un produit possiblement toxique pour les racines nerveuses, il est difficile d’exclure un processus de fuites épidurales si on ne s’est pas assuré de la continence discale avant l’injection intra-discale. Dans ce but, la réalisation d’une discographie quelques jours auparavant est théoriquement envisageable mais cette procédure alourdie la prise en charge thérapeutique et en augmentant le nombre d’abord discal augmente le risque infectieux. En revanche, l’injection d’un produit de contraste intra-discal avant l’injection du Discogel ® semble peu compatible pour des raisons de volume discal limité et de dilution du dispositif injecté. De plus, cette procédure s’avère imparfaitement efficace puisqu’elle n’empêche pas la survenue de radiculites bénignes dans 3,7 % des cas et de complications neurologiques sévères dans environ 0,45 % des nucléolyses .
Dans ce cadre, nous avons proposé une étude observationnelle ouverte dont l’objectif était :
- •
de tester une procédure de discographie aérique pour limiter les risques de fuites épidurales ;
- •
de renseigner l’efficacité et la tolérance du Discogel ® par une deuxième équipe.
2.2
Méthode
2.2.1
Population
Le suivi des patients s’inscrivait dans un schéma de soins courants habituellement délivré au sein de notre équipe. Il a été proposé consécutivement à 79 patients répondant aux indications des traitements des lombosciatiques par voie percutanée de bénéficier du Discogel ® .
2.2.2
Critères d’éligibilité
Critères d’inclusion :
- •
patients souffrant de lombosciatique par conflit disco-radiculaire ;
- •
depuis au moins huit semaines ;
- •
résistant au traitement médical bien conduit ;
- •
incluant au moins deux infiltrations épidurales, dont au moins une réalisée sous contrôle scopique.
Critères de non-inclusion :
- •
présence d’une hernie exclue ou migrée ;
- •
observation de disques intervertébraux très pincés sur l’imagerie TDM ou IRM.
2.2.3
Procédure et technique
Le geste était réalisé au cours d’une journée d’hospitalisation, au sein d’un service de chirurgie ambulatoire, sous neurosédation. Le disque traité était abordé sous contrôle scopique, à l’aiguille (18-G, 10 cm), par voie postéro-latérale, du côté de la douleur du patient. L’aiguille mise en place servait de guide pour la ponction discale. Le disque était alors ponctionné au moyen d’une aiguille plus fine (22-G, 15 cm) dont l’extrémité était située au centre du disque intervertébral par un contrôle scopique de face et de profil. Pour augmenter la sécurité du geste sans risquer de diminuer l’efficacité du dispositif, une discographie à l’air filtré était réalisée avec une seringue de 10 mL et un filtre bactérien, afin de s’assurer de la rénitence du disque. La rénitence discale était jugée satisfaisante si :
- •
une sensation de résistance à l’injection survenait avant les 10 mL de volume de la seringue ;
- •
au relâchement de la pression manuelle, le piston de la seringue revenait d’au moins deux graduations.
Puis, selon les recommandations du Discogel ® , 0,7 mL du dispositif était injecté lentement (0,1 mL toutes les 30 secondes sous contrôle scopique). À la fin de l’injection, le guide de l’aiguille était remis en place et l’aiguille était laissée en position pendant deux minutes, pour limiter le risque de fuite au moment du retrait.
Après l’intervention, les patients étaient surveillés trois heures, le temps que les effets de la neurosédation se dissipent. Les patients sortaient avec une prescription d’anti-inflammatoire et d’antalgique pour huit jours. Ils avaient pour consigne d’éviter les stations assises prolongées. Par mesure systématique et de manière similaire aux procédures de discectomie chirurgicale, un arrêt de travail était prescrit pour une durée de six semaines mais les patients étaient informés de la possibilité de reprise professionnelle au bout de trois semaines s’ils s’en sentaient capables.
2.2.4
Critères de jugement
Pour évaluer la procédure percutanée nous nous sommes en premier lieu intéressé à la douleur périopératoire immédiate. L’ensemble des patients a bénéficié d’une évaluation globale de la douleur ressentie en peropératoire et en postopératoire immédiat par l’infirmière anesthésiste. L’intensité de la douleur était évaluée au moyen d’une échelle verbale numérique (0 = pas de douleur ; 10 = douleur maximale imaginable). La question était posée trois fois pendant l’intervention et une fois par heure lors des trois heures de surveillance en salle de réveil.
En second lieu nous avons suivi l’évolution des douleurs. Chez les 66 premiers patients injectés, une évaluation de la douleur globale était réalisée, par une infirmière anesthésiste, par appel téléphonique au huitième jour après l’intervention. Deux évaluations portant sur l’intensité des douleurs lombaire et radiculaires étaient faites par le thérapeute au cours de consultation, le jour de l’inclusion et huit semaines après le geste. Une troisième évaluation était effectuée par remplissage d’un questionnaire téléphonique, soumis au moins quatre mois après le geste par un évaluateur indépendant. Les paramètres alors évalués étaient les intensités des douleurs lombaires et radiculaires, recueillies au moyen d’une échelle verbale numérique (0 = pas de douleur, 10 = douleur maximale imaginable). Les patients répondaient également aux trois questions suivantes :
- •
Avec le recul que vous avez, comment qualifieriez-vous le résultat de ce traitement : très bon, bon, moyen, mauvais ?
- •
Ce traitement vous a-t-il permis de reprendre votre vie professionnelle antérieure ?
- •
Est-ce que vous recommanderiez ce traitement à un ami ou quelqu’un de votre entourage proche qui aurait le même problème ?
2.3
Résultats
Soixante dix-neuf patients (40 femmes et 39 hommes, âge moyen 40 ± 12 ans) ont été inclus. Ils souffraient en moyenne depuis 14 ± 12 mois. Les disques injectés étaient aux niveaux L4-L5 chez 40 patients, L5-S1 chez 31 patients et aux deux niveaux chez huit patients. La Fig. 1 montre un exemple de procédure sur le disque L5-S1 : la ponction du disque ( Fig. 1A ), l’aérogramme discal obtenu par l’injection aérique ( Fig. 1B ) et l’opacification discale induite par le Discogel ® en place ( Fig. 1C ) venant prendre la place de l’aérogramme discal. La procédure de discographie aérique a amené à la découverte d’un disque non rénitent chez deux patients (3,7 %), chez lesquels le Discogel ® n’a donc pas été injecté. L’évolution des douleurs périopératoires est rapportée dans le Tableau 1 . Parmi les 79 patients injectés, les intensités moyennes des douleurs peropératoires et postopératoires immédiates diminuaient de manière significative par rapport à l’intensité moyenne de la douleur préopératoire ( p < 0,0001). Durant la période peropératoire, la douleur globale augmentait chez cinq patients (1 point chez deux patients et 2 points chez trois patients). Aucune de ces douleurs n’a nécessité un ajustement de la procédure. En période, postopératoire immédiate, trois patients ont rapporté une augmentation de leur douleur (1 point chez un patient, 2 points chez un patient et 4 points chez un patient). Aucune des ces augmentations douloureuses temporaires n’a nécessité un ajustement thérapeutique. Aucun déficit sensitif ou moteur n’a été rapporté pendant cette période périopératoire immédiate.