Percutaneous Submuscular Plating of the Humerus
Bruce H. Ziran
David W. Robinson
INDICATIONS FOR SUBMUSCULAR PLATING
Open plating of the humerus has been the favored treatment method amongst most orthopaedic traumatologists. Humeral nailing, while still a very successful modality, is less favored amongst traumatologists, but by virtue of its strong commercial success, would imply that it is a popular modality in general orthopaedics. Why this rift in treatment exists is difficult to explain, but may be due to the minimally invasive nature of nailing and its appeal to general orthopaedic surgeons. The issues of shoulder problems may be a function of technique and implant design, and the slightly lower union rate may possibly be due to mechanobiology or fracture gaps. Open plating is ideal for fracture patterns that allow for compression and direct bone healing. However, there is also a theoretical risk that bone healing may be impaired with open reduction due to greater disruption of the fracture site vascularity and soft tissue attachments. Other associated drawbacks include greater morbidity,1 due to a larger incision and dissection, and postoperative elbow complaints.2,3 Plating techniques require knowledge of fracture mechanobiology, such as whether absolute stability or relative stability is the desired environment for healing. In general, the stiffer the construct created, the more anatomic the reduction required. Very stiff constructs with fracture gaps may lead to nonunion. Similarly, nonunion rates are increased with canal-filling nails and associated fracture gaps. Relative stability is achieved with long bridging plates or small, non-canal-filling nails (i.e., flexible nails). With both of these modalities, stability is sacrificed, especially with traditional plates using long spans and nonlocking screws.
Recently, submuscular (Minimally Invasive Percutaneous Plate Osteosynthesis, MIPPO) plating of humeral shaft fractures has been introduced by Livani and Belangero4 with excellent results. Their technique utilizes a safe anterior corridor of the humerus that is relatively unpopulated with neurovascular structures. Through two small windows, proximally and distally, a plate is inserted deep to the brachialis muscle, the fracture is reduced, and stabilized to the plate. Surprisingly, even with nonlocked screws in comminuted fractures, Livani and Belangero reported excellent healing. It may be due to the preservation of fracture biology with the judicious creation of relative stability with nonrigid constructs. In order to further enhance stability, without compromising biology, Ziran et al.5 further modified the technique to incorporate newer technology of locked screws. Other studies corroborated these findings6,7 though it was initially reserved for fracture patterns with a low strain modulus, for example, comminuted fractures. However, other evidence has shown good outcomes using this technique even with simple fracture patterns.5 In addition, the percutaneous technique is aesthetically more acceptable and may have the benefits of closed nailing, where the muscle envelope is less violated, but does not incur the shoulder problems associated with intramedullary nails.
The authors cannot identify any absolute contraindications to using minimally invasive technique except those applicable to traditional open reduction and internal fixation of the humerus, but caution its use with very distal humerus fractures. Proximal humerus fractures that are amenable to proximal humeral plate fixation can also be treated with the submuscular technique, but the position of the proximal plate needs to be modified to be placed anteriorly, and a long plate is required (Fig. 5.1). These plates are 3.5 mm in size, and the entire construct may not be suitable for immediate weight-bearing. Some recent studies have noted that using 3.5-mm plates for humeral shaft fractures may be acceptable in certain cases and
in smaller-sized patients. While the authors prefer a 4.5-mm plate, the ability to use a single plate for such complex fractures, and in a minimally invasive method, may outweigh the disadvantage of the smaller plate. Relative contraindications include neurovascular injury requiring surgical exploration, open fractures with substantial soft tissue involvement necessitating aggressive debridement, and segmental fractures with insufficient bone proximally and distally for stable fixation.
in smaller-sized patients. While the authors prefer a 4.5-mm plate, the ability to use a single plate for such complex fractures, and in a minimally invasive method, may outweigh the disadvantage of the smaller plate. Relative contraindications include neurovascular injury requiring surgical exploration, open fractures with substantial soft tissue involvement necessitating aggressive debridement, and segmental fractures with insufficient bone proximally and distally for stable fixation.
The purpose of this present report is to describe in detail the authors’ method of submuscular plating of the humerus. Since the technique may be unfamiliar to most surgeons, the authors recommend beginning with a standard open anterior approach, and then gradually decreasing the sizes of the skin portal as comfort with the technique and anatomy improve (Fig. 5.2).
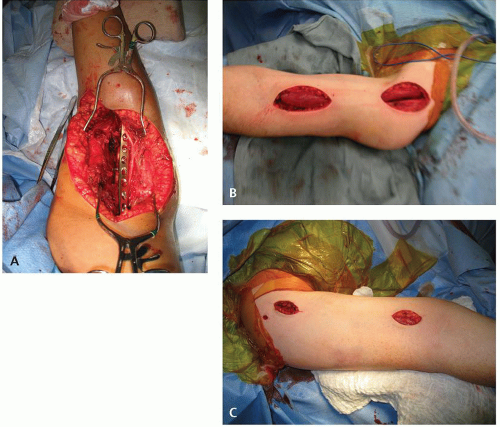 Figure 5.2 A: Standard open anterior approach. B: Minimally invasive approach—larger skin portals. C: Minimally invasive approach—smaller skin portals. |
PATIENT POSITIONING
The room is best set up such that the scrub technician/nurse and surgical equipment are on the contralateral side of the patient or at the foot of the bed, with fluoroscopy (sterilely draped) positioned on the ipsilateral side. The patient is supine with a hand table that allows imaging from its underside (no legs). The fluoroscopy machine should be positioned to move in and out of the field from the distal aspect of the hand table. The full arm should be prepped and the patient draped from the ipsilateral nipple to the ipsilateral angle of the jaw to below the axilla. In Livani and Belangero’s original technique, they positioned the arm at approximately 60 degrees of abduction, and a sterile bump (such as a stack of sterile towels wrapped with Coban) was placed under the fracture site as a fulcrum to overcome gravitational apex posterior deformity (Fig. 5.3). In our modified technique, an external fixator (mini-distractor) is used to maintain the reduction. A tourniquet is not used (or needed) since it invariably overlays the location of the proximal incision. If necessary, especially when an external fixator is not used, a third assistant may provide gentle in-line traction with the elbow flexed (this relaxes the biceps brachii, brachialis, and brachioradialis) to achieve and maintain length during the case.
SURGICAL APPROACHES
Most surgeons are hesitant to consider submuscular plating when considering the neurovascular structures of the arm. But when one looks at cross-sectional anatomy, there is a safe anterior window that can be utilized safely to apply and fix a plate to the humerus. The authors do not advocate submuscularly inserting the plate in any other anatomic corridor, such as lateral, or posterior due to the dangers of injuring a vital structure.
Identification of the skin incisions is done by placing the plate over the anterior aspect of the arm with the elbow flexed to 90 degrees (Fig. 5.4). The plate is centered over the fracture zone, utilizing fluoroscopic guidance (Fig. 5.5). The
appropriate length of plate is then determined depending on the caliber of plate used. For 3.5-mm systems, the plate length is usually 10 to 16 holes, while for 4.5-mm systems, the plate length is usually 9 to 14 holes (narrow plate, not wide). The ends of the plate are marked on the skin using a sterile pen (Fig. 5.6).
appropriate length of plate is then determined depending on the caliber of plate used. For 3.5-mm systems, the plate length is usually 10 to 16 holes, while for 4.5-mm systems, the plate length is usually 9 to 14 holes (narrow plate, not wide). The ends of the plate are marked on the skin using a sterile pen (Fig. 5.6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree











