Percutaneous Plating of the Proximal Humerus
G. Yves Laflamme
Dominique Rouleau
INDICATIONS
Proximal humeral fractures represent up to 5% of all fractures occurring most often in elderly patients over the age of 60 years as the result of a simple fall.1 Even among experts, controversy exists regarding the indications for surgical management since evidence-based treatment guidelines are lacking.2
Percutaneous plating was developed in an attempt to address the issues of humeral head necrosis associated with open reduction through an extensive approach and insufficient primary stability associated with previous attempts at limited exposure and minimal internal fixation.3 A locking plate provides stable fixation for early range of motion reducing soft tissue scarring and loss of the gliding surfaces.
Surgery is generally indicated when fracture instability prevents early motion or when fracture displacement is sufficiently great that functional impairment is likely. With a minimally invasive approach, indirect reduction techniques are needed to achieve an acceptable reduction. For this reason, we caution against the use of this technique for complex fracture -dislocations, head-split, four-part fractures, and nonunions of the proximal humerus. Displaced unstable two-part surgical neck fractures, isolated greater tuberosity fracture, and valgus-impacted (three- or four-part) fractures are ideal fracture types that can be easily reduced through a mini-incision especially during the learning curve period. With increased experience with this percutaneous technique, three-part fractures and some four-part fractures can be tackled but sometimes extending this approach to an extended lateral deltoid split approach is needed to obtain adequate reduction.4 A minimally invasive incision should not be used if the best obtainable reduction is suboptimal.
PATIENT POSITIONING
The patient is positioned in a supine position on a radiolucent table with a soft bump placed behind the patient’s chest. This positioning is ideal for multiply injured patients especially if cervical spine issues complicate head positioning or if associated fractures to the extremities need fixation. Simultaneous surgery is possible without the need to reposition. The entire upper extremity is draped to allow free mobility for reduction maneuvers and for optimal imaging during surgery. The setup is checked before draping with the C-arm unit brought on the opposite side to ensure complete visualization of the proximal humerus including a modified axillary view.
Alternative Positioning
The patient is placed in a beach chair position on a specialized operating room table that allows access to the shoulder. The head is immobilized in a head holder. The image intensifier is placed parallel to the table at the patient’s head on the injured side. This setup allows adequate fluoroscopic visualization of the shoulder (axillary view) and conversion to a hemiarthroplasty if the fracture is unreconstructible but limits the access to the operative site.
SURGICAL APPROACH
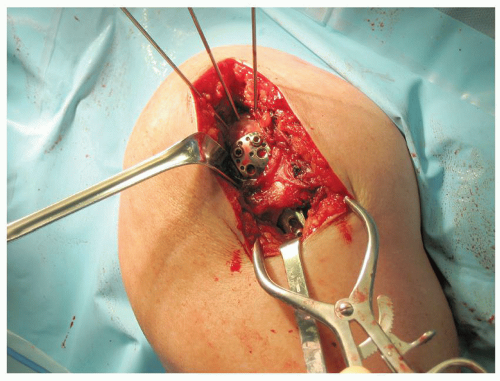
This minimally invasive technique allows limited disruption of soft tissue with application of the plate on the lateral side of the humeral head away from the primary vascular supply, the ascending branch of the anterior humeral circumflex artery that runs adjacent to the bicipital groove. A hypovascular bare spot of 3 cm in width was identified by Gardner et al.5 on the greater tuberosity and a plate applied to this region may minimize iatrogenic vascular injury when treating these fractures. After proper positioning of the patient, we proceed with a direct minimally invasive lateral approach to the proximal humerus with two separate mini-incisions: The proximal window exposes the greater tuberosity and the humeral head and the distal window exposes the humeral shaft and distal part of the plate. Internal or external rotation with abduction facilitates exposure through these mobile windows.
PROXIMAL INCISION
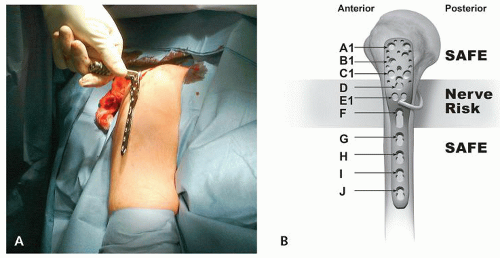
The anterior edge of the acromion is palpated and used as a landmark (Fig. 6.1). Starting 1 cm distal from this point, a direct lateral longitudinal incision is made distally for 4 cm in-line with the middle of the humeral head. The subcutaneous tissue is incised, and the deltoid fascia is visualized and transected parallel to the underlying deltoid muscle fibers. The deltoid muscle fibers are bluntly split until the underlying subdeltoid bursa is exposed. Finger dissection is then needed to elevate the deltoid muscle from the proximal humerus. The fracture lines are able to be palpated at this point, but it is critical to identify the axillary nerve (Fig. 6.2).
The average distance from the lateral edge of the acromion to the axillary nerve is 7 cm (range, 62 to 85 mm).6 This cord-like band is located in the posterior aspect of the wound as it exits the quadrangular space and then runs on the undersurface of the deltoid around the humerus as it innervates the deltoid muscle. If scarring or hematoma prevents palpation of the nerve, the surgeon should consider extending the incision and directly identifying the nerve using the extended lateral or anterolateral (AL) deltoid splitting approach.4,5
DISTAL INCISION
Mapping the second window is facilitated by the plate used as a template over the skin (Fig. 6.3). A 2-cm incision is made in-line and distal to the previous incision and is centered over the distal three screw holes (Fig. 6.4). The correct location is confirmed using fluoroscopy. The subcutaneous tissue and deltoid musculature are bluntly dissected. This incision is well below the course of the axillary nerve.
 Figure 6.4 The proximal and distal incisions are made, one proximal and one distal to the crossing axillary nerve. |
ALTERNATIVE APPROACH
The extended AL acromial approach allows minimally invasive access to the proximal humerus. The AL acromial approach uses the anterior deltoid raphe between the anterior and middle deltoid heads as a surgical plane, which allows direct visualization of the axillary nerve.5 With the shoulder in neutral rotation, an approximately 10-cm incision is made beginning at the AL corner of the acromion and carried distally. After splitting the raphe approximately6 cm distally in the wound, the axillary nerve is identified and protected (Fig. 6.5). This is our preferred approach for complex fractures or nonunions of the proximal humerus. The axillary nerve is visualized and can be mobilized to insert the inferomedial oblique “calcar” screws.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree