Percutaneous Pinning of Distal Radius Fractures
Peter H. DeNoble
Louis W. Catalano III
INDICATIONS
Distal radius fractures are common and various treatment options exist. Successful management must consider patient factors and fracture pattern. Percutaneous reduction and fixation are indicated for AO/ASIF extra-articular fractures A2, A3, three- and four-part fractures C1, C2. It is most effective for fractures that can be closed reduced via traction manipulation and ligamentotaxis. As a less expensive alternative to plates and screw fixation or external fixation, closed reduction and percutaneous pinning (CRPP) is currently the most cost-effective option for the treatment of distal radius fractures. In the authors’ hospital system, the average cost of a 1.58-mm (0.0625-in) K-wire is $23, bringing a three- to fivewire construct to a total of $69 to $115. This compares favorably to a volar plate plus 8- to 12-screw construct, which cost an average of $1,255, and various forms of external fixators that can range from about $600 to $1,300.
Some distal radius fractures are not amenable to percutaneous treatment alone. Contraindications to CRPP include fractures with severe dorsal metaphyseal or intra-articular comminution, fractures in patients with poor bone stock, especially with fracture comminution, and AO/ASIF type B fractures (e.g., Volar Barton fracture).
PATIENT POSITIONING
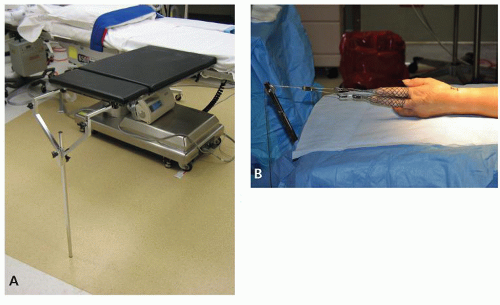
The patient is positioned supine with a hand table that accommodates an outrigger for longitudinal traction (Carter Hand Surgery Table, Innovation Sport, Foothill Ranch, CA) (Fig. 3.1A). Finger traps on either the thumb and index finger or index and long fingers are attached to a wire that runs over a pulley on the traction outrigger (Fig. 3.1B). A traction of 2.27 to 4.53 kg (5 to 10 lb) is applied to the wire, and the limb is horizontal on the hand table.
REDUCTION TECHNIQUES
The mini C-arm image intensifier (Fig. 3.2) is sterilely draped and brought into the field.
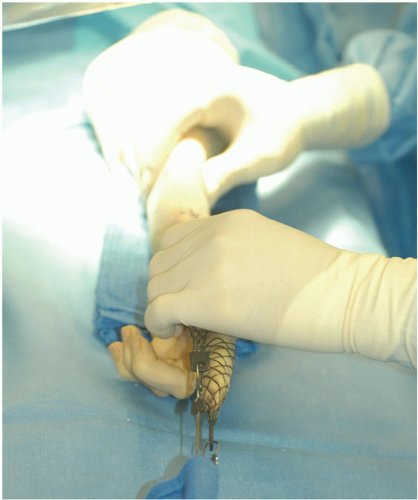
Posterior-anterior (PA) and lateral images of the distal radius are obtained. The fracture is manipulated with a volarly directed pressure on the dorsal aspect of the distal fracture
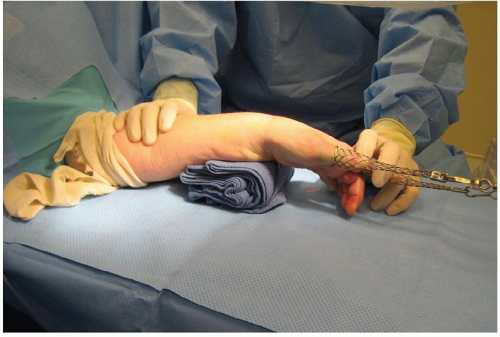
fragment in an effort to restore length and volar tilt (Fig. 3.3). In instances where there is radial translation of the distal fragment, a small bump fashioned from a folded stack of towels and is placed under the ulnar aspect of the proximal fragment to serve as an additional fulcrum for reduction. One hand stabilizes the forearm proximally while the other applies an ulnarly translating force to the wrist and hand distally (Fig. 3.4). Reduction is monitored fluoroscopically (Fig. 3.5). If good alignment is achievable via closed reduction, then the surgeon may proceed with the planned percutaneous pin fixation. If the fracture is not reducible closed, then open reduction and internal fixation may be required.
fragment in an effort to restore length and volar tilt (Fig. 3.3). In instances where there is radial translation of the distal fragment, a small bump fashioned from a folded stack of towels and is placed under the ulnar aspect of the proximal fragment to serve as an additional fulcrum for reduction. One hand stabilizes the forearm proximally while the other applies an ulnarly translating force to the wrist and hand distally (Fig. 3.4). Reduction is monitored fluoroscopically (Fig. 3.5). If good alignment is achievable via closed reduction, then the surgeon may proceed with the planned percutaneous pin fixation. If the fracture is not reducible closed, then open reduction and internal fixation may be required.
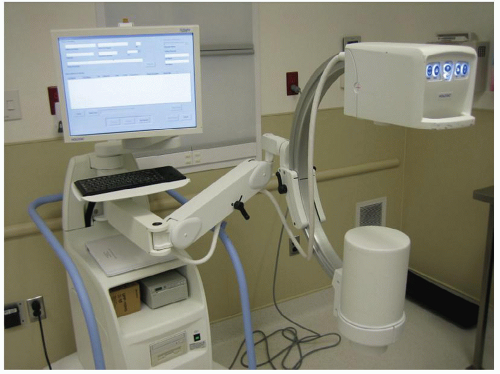 Figure 3.2 A mini-fluoroscopy unit is ideal for visualizing the distal radius and allows the surgeon and assistant to easily maneuver around it during the pin placement. |
SURGICAL APPROACHES/PINNING TECHNIQUES
The authors prefer to use 1.58-mm (0.0625-in) K-wires exclusively and prefer to place pins in the radial styloid first. In order to avoid injury to the superficial sensory branch of the radial nerve, the pins are placed under direct vision using a 1.5-cm longitudinal incision extending from the tip of the radial styloid distally (Fig. 3.6). A dissecting scissor is used the spread through the subcutaneous tissue and isolate the underlying branches of the superficial radial nerve and first extensor compartment tendons (Fig. 3.7). Ragnell retractors are then used to
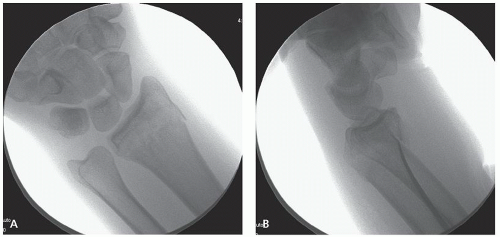
bluntly retract the nerve branches and tendons. This exposure also allows the starting points to vary in the volar-dorsal direction according to the needs of the fracture pattern without risk of nerve injury.1 The first pin is usually started at the tip of the styloid, just dorsal to the first extensor compartment (Fig. 3.8). This pin may also be placed volar to the tendons depending on the fracture pattern and the position of the sensory nerve. In addition, the trajectory of the first pin may need to accommodate for some loss of volar tilt reduction that often occurs after the initial closed reduction. Thus, the first pin should be advanced through the distal fragment in a more volarly angulated fashion in order to allow for appropriate reorientation in the sagittal plane following re-reduction. In the coronal plane, this pin is passed at a relatively shallow oblique angle to the level of the fracture site (Fig. 3.9A). Full manual reduction pressure is then reapplied, and fracture reduction is confirmed on the PA and lateral views. The K-wire is subsequently advanced into the ulnar cortex of the radius proximal to the fracture (Fig. 3.9B). Typically a second 1.58-mm (0.0625-in) K-wire is placed in a similar but slightly divergent trajectory to the first pin in both planes, maximizing construct stability. During wire placement, the first wire may substitute for a retractor, freeing an assistant’s hand (Fig. 3.10). Reduction is confirmed on PA and lateral fluoroscopy (Fig. 3.11).
bluntly retract the nerve branches and tendons. This exposure also allows the starting points to vary in the volar-dorsal direction according to the needs of the fracture pattern without risk of nerve injury.1 The first pin is usually started at the tip of the styloid, just dorsal to the first extensor compartment (Fig. 3.8). This pin may also be placed volar to the tendons depending on the fracture pattern and the position of the sensory nerve. In addition, the trajectory of the first pin may need to accommodate for some loss of volar tilt reduction that often occurs after the initial closed reduction. Thus, the first pin should be advanced through the distal fragment in a more volarly angulated fashion in order to allow for appropriate reorientation in the sagittal plane following re-reduction. In the coronal plane, this pin is passed at a relatively shallow oblique angle to the level of the fracture site (Fig. 3.9A). Full manual reduction pressure is then reapplied, and fracture reduction is confirmed on the PA and lateral views. The K-wire is subsequently advanced into the ulnar cortex of the radius proximal to the fracture (Fig. 3.9B). Typically a second 1.58-mm (0.0625-in) K-wire is placed in a similar but slightly divergent trajectory to the first pin in both planes, maximizing construct stability. During wire placement, the first wire may substitute for a retractor, freeing an assistant’s hand (Fig. 3.10). Reduction is confirmed on PA and lateral fluoroscopy (Fig. 3.11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree