Percutaneous Pelvic Ring Fixation
Jason M. Evans
INDICATIONS
Management of injured patients with pelvic ring disruptions is driven by both deformity and the treating physician’s interpretation of pelvic stability. As such, the goals of operative intervention for pelvic fractures are based on reducing deformity and providing enough stability to the injured pelvis to allow for patient mobilization. Any discussion regarding the utility of minimally invasive stabilization must be made with respect to the necessity of obtaining a reduction. If the deformity cannot be corrected through minimally invasive techniques, then a formal open reduction should be utilized. This will frequently carry additional surgical morbidity, including the potential for increased blood loss and deep infection or wound dehiscence. Therefore, even when planning a percutaneous procedure, discussion should be had with the patient regarding the potential need to convert to an open procedure, and consent should be obtained for both options. In addition, patients with pelvic ring disruptions frequently have injuries to other organ systems. The coordinating intensive care service, typically the general trauma surgeons should also be made aware of the potential need to convert to an open procedure. In the common scenario of ongoing resuscitation or incomplete resuscitation, they may feel that a patient may be able to tolerate only a percutaneous procedure, and open discussion should then proceed regarding what may be the optimal timing for the procedure. Generally speaking, minimally invasive techniques can be considered for both anterior and posterior ring pathology, including both ligamentous injuries (symphysis and sacroiliac disruptions) and fractures (sacral fractures, posterior iliac fractures, pubic ramus fractures).
Pelvic ring disruptions with minimal displacement are frequently managed nonsurgically; however, some demonstrate considerable instability to stress under anesthesia.1 These patterns are particularly well suited for percutaneous management. While displacement is not a contraindication to definitive minimally invasive treatment, the surgeon should acknowledge that as the displacement becomes more dramatic, reductions do become more difficult to obtain by closed or limited open means. This is potentially due to a number of factors, including interposed periosteum, fascia, or nerves.
Severely displaced pelvic ring disruptions frequently involve injury to the symphysis, and patients with these types of high-energy pelvic ring disruptions commonly present in hemorrhagic shock. Rapid angiographic embolization of arterial bleeding is employed at many trauma centers and plays a key role in resuscitation. Venous bleeding, however, is much more common and can result in significant loss of blood volume. Minimally invasive means of diminishing pelvic volume with the use of circumferential sheeting, percutaneous “C-clamp,” or percutaneous application of an external fixator are effective at minimizing ongoing bleeding and are theorized to provide enough stability to allow clotting to occur to tamponade the bleeding.
Application of an external fixation frame to the pelvis in an attempt to manage the physiologically unstable patient by controlling pelvic volume and stabilizing clot has historically been the most common application of minimally invasive techniques for managing pelvic fractures. Technologic advances such as therapeutic embolization, and application of ‘lowtech’ circumferential wraps using either hospital linens or commercial binders, have increasingly limited the use of a “resuscitative” anterior pelvic external fixator or the closely related posterior pelvic “C-clamp.” Drawbacks to anterior pelvic external fixation are many, and include: Improperly positioned pins, interference with future operative approaches, pin tract infections, potential for septic seeding of joints, and negative impact on patient positioning.
These have led to an increasing utilization of percutaneous insertion of internal fixation. In addition to minimizing the potential complications of external fixation, internal fixation adds superior biomechanics to the definitive construct.2, 3, 4 and 5 Recently a technique for rapid stabilization of an unstable patient with a pelvic ring disruption has been described, utilizing a “damage-control iliosacral screw,” demonstrating the expanding indications for minimally invasive stabilization of the injured pelvis.6
These have led to an increasing utilization of percutaneous insertion of internal fixation. In addition to minimizing the potential complications of external fixation, internal fixation adds superior biomechanics to the definitive construct.2, 3, 4 and 5 Recently a technique for rapid stabilization of an unstable patient with a pelvic ring disruption has been described, utilizing a “damage-control iliosacral screw,” demonstrating the expanding indications for minimally invasive stabilization of the injured pelvis.6
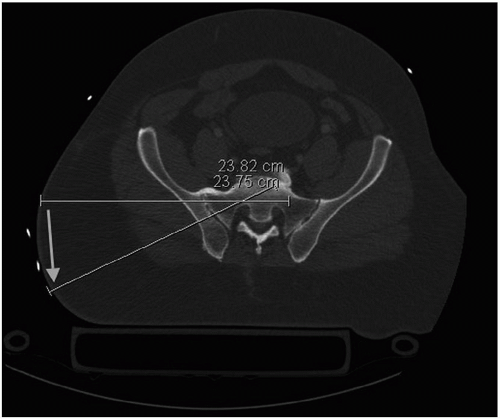
Specific indications for minimally invasive pelvic surgery vary based on surgeon experience and technical ability. In addition, hospital resources, such as appropriate preoperative and intraoperative imaging capabilities, play a substantial role. As patient anatomy is variable, it is vital to have imaging information that can be properly interpreted with regard to various feasible pathways for fixation. Inability to safely place an implant, either due to inaccurate reduction, inadequate imaging, or incompatible patient anatomy, is an absolute contraindication to percutaneous surgery.
PATIENT POSITIONING
Patients with pelvic ring injuries frequently will have multiple associated injuries that may complicate patient transfer and intraoperative positioning.7 Perhaps the most inconvenient of these is associated unstable spine injuries; however, nonskeletal injuries can also pose a problem when planning percutaneous surgery. Placement of chest tubes, cystostomy tubes, and ostomies can pose difficulties in both positioning and creating and maintaining a sterile surgical field.
The supine position is appropriate for most percutaneous intervention, but prone positioning is occasionally preferred for fracture patterns involving the posterior ilium, or if a retrograde posterior column screw is planned. The lateral position carries multiple disadvantages to percutaneous surgery, including greatly increased difficulty in obtaining necessary imaging, potential obstruction of hand position necessary for proper screw trajectory, accentuation of rotational deformity due to gravity forces, and limited or no access to contralateral hemipelvis. While the lateral position is familiar to surgeons, operating room personnel, and occasionally preferred by the anesthesia team, it should be avoided for most minimally invasive pelvic fixation procedures.
A fully radiolucent table is important to provide consistent and reproducible high-quality imaging. A close working relationship with the fluoroscopy technician can eliminate many of the potential frustrations during minimally invasive surgery, and is facilitated by utilizing a consistent set of terminology to describe c-arm positions. When planning percutaneous iliosacral screw insertion, elevating the patient on several folded blankets placed midline from the lumbar region and distal will permit proper trajectory when oblique screw orientation is called for, such as sacroiliac joint disruptions and patients with sacral dysmorphism. Without this moderate elevation on the table, the wire, drill, or screwdriver may abut the table, making proper insertion difficult or impossible (Fig. 8.1).
SURGICAL APPROACHES
Palpable bony landmarks can be used to orient and provide regional safe zones for incision placement. Virtual quadrants can be drawn on the flank, for example, when preparing for iliosacral screw insertion, using a line drawn parallel to the axis of the femoral shaft and another drawn straight posterior from the anterior superior iliac spine. The majority of safe screw insertions are placed in the posterosuperior quadrant. It is critical to recall that screw trajectory within the sacrum will dramatically alter the location of the correct skin incision. This is perhaps most clearly depicted when placing fixation in each of the two upper sacral segments in a dysmorphic sacrum. The caudal-to-cranial and posterior-to-anterior trajectory of the upper screw will have a skin incision that is more distal and posterior on the skin than the more horizontally inserted second sacral screw (Fig. 8.2).
Incision placements for Schanz pins are based in relation to subcutaneous landmarks. Incisions for screws placed down the gluteus medius pillar are placed using the palpable iliac crest as a guide. Although incisions may initially start very small, if the pelvic displacement is dramatic, then correction of displacement does not uncommonly require the incision to be extended quite a bit. This should be considered when making the incision and critical assessment should be made to determine the orientation of the incision as well. This wound extension may interfere with surgical incisions if open reduction is planned for definitive management. When utilizing the supraacetabular pin location, an incision approximately 2 cm distal to the ASIS is a good starting point, but given that appropriate trajectory can be dramatically influenced by existing displacement, it is again helpful to obtain a precise starting point on the AIIS with fluoroscopic guidance and a small diameter wire placed percutaneously prior to definitive incision.
For retrograde ramus screws, the incision is typically a centimeter or so across the midline on the contralateral side of the body from the fractured ramus. Variations in anatomy can make this insertion technique impossible. Varying pelvic obliquity, or relative flexion and extension of the pelvis, which may result in a symphysis that “sits low,” combined with the perineal structures in both males and females, can prevent safe creation of incisions that allow for the necessary screw trajectory. Special attention to prepping in a large surgical field and isolation of the perineum with adhesive drapes can help assure that the appropriate start point is not “prepped-out.” Taking advantage of the relative mobility of the skin and soft tissues in this region by drawing the skin distally with the opposite hand can help with this approach. Relaxation of this tension following screw insertion allows the incision to “retract” cranially.
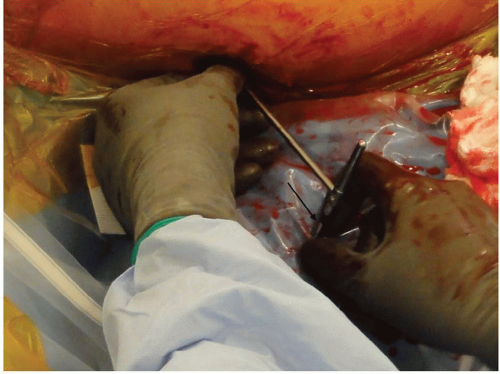
There is no fracture exposure utilized and the procedures are performed through 1.5- to 2-cm “stab” incisions. A common error is to try to make these incisions too small, precluding the insertion of the surgeon’s finger along with the screw. This is frequently helpful to “guide” the screw through the occasionally deep soft tissue envelope. The deep investing
muscle fascia can impede the precise adjustments in positioning, and special attention should be paid to incising this deep fascia with the blade to provide improved control of wires and drill bits passing through a single soft tissue “tunnel.” Specialized cannulated instrumentation is also available to facilitate instrument and implant placement.
muscle fascia can impede the precise adjustments in positioning, and special attention should be paid to incising this deep fascia with the blade to provide improved control of wires and drill bits passing through a single soft tissue “tunnel.” Specialized cannulated instrumentation is also available to facilitate instrument and implant placement.
Frequently, the percutaneous incisions utilized for minimally invasive fracture fixation in the extremities are planned along the line of a traditional exposure, and can easily be incorporated into the full approach in the event that it is deemed necessary intraoperatively. The limited available pathways for fixation in the pelvis necessitate precise trajectory, placing the stab incisions fairly remote from traditional approaches to the pelvis. It should be noted, however, that traditional exposures could still be safely used, without need for modification, should minimally invasive techniques be abandoned intraoperatively.
Imprecise placement of the stab incisions can be frustrating, as the surgeon needs to “fight” the interfering tissues. A small diameter long smooth K-wire or Steinmann pin can be used percutaneously prior to incision to more accurately position the surgical incision. This can be used with fluoroscopy to find the desired starting position on the bone, and is easily withdrawn and repositioned several times with very minimal insult to skin and soft tissue.
IMAGING
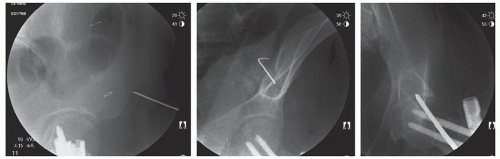
As previously stated, adequate intraoperative imaging is critical to the success of any minimally invasive stabilization procedure for pelvic disruptions. Several reproducible fluoroscopic images are routinely used during these procedures. In addition to AP hip and pelvis, inlet and outlet views, and traditional Judet oblique views, merging these views to provide an “obturator-outlet,” or “tee-pee” view helps to guide implants into the columns of bone available for fixation (Fig. 8.3). Making subtle modifications to these images is typically used to most accurately represent the patient’s anatomy.8 For example, the inlet view can be modified slightly to enhance the anterior cortical border of different sacral segments, and adding varying obliquity to the outlet view can bring the posterior iliac lateral cortex into profile, which can be particularly helpful to avoid washer cortical intrusion during iliosacral screw insertion (Fig. 8.4), and slight outlet tilt on an oblique view can enhance the cortical projection of the anterior column.
REDUCTION TECHNIQUES
Disruptions of the pelvic ring produce several recognizable and reproducible patterns of fracture, dislocation, and displacement. These patterns have been well described and studied.9, 10 and 11 Closed reduction techniques are utilized in relation to these concepts, and utilize large
diameter Schanz pins placed strategically into each hemipelvis. These screws function as “joysticks” for reduction maneuvers, and can easily be removed or incorporated into an external fixator as part of definitive fixation.
diameter Schanz pins placed strategically into each hemipelvis. These screws function as “joysticks” for reduction maneuvers, and can easily be removed or incorporated into an external fixator as part of definitive fixation.
Resuscitative external fixation frames have taken many forms over the years. Attempts to improve the stability imparted to the posterior pelvic ring have resulted in some fairly complex configurations, none of which ultimately reliably control the posterior ring, or have proven more effective than a simple, two-pin design.12,13 While acknowledging the shortcomings of this type of fixation, it can still play a role in temporary stabilization of the unstable patient and pelvis, although far less frequently at major trauma centers today than in the past.
While external fixation lacks ideal biomechanics,14 it is very effective as a manipulative device for mobilizing both hemipelves.13 For widely displaced pelvic fractures, long Schanz pins act as joysticks to grossly realign the pelvic ring and decrease overall pelvic volume. Historically, these Schanz pins have been placed from the subcutaneous iliac crest directed down the column of bone referred to anatomically as the gluteus medius pillar. One, two, or three pins can be placed between the cortical “tables” on each ilium, distributing the forces over a greater portion of the iliac bone. This technique can be used without fluoroscopy if necessary, by using smooth K-wires slid extraosseously on the medial and lateral cortex of the ilium to guide the Schanz pins. This increases the likelihood of a pin obtaining solid purchase in bone without cortical extrusion. This scenario should be unusual, however, as c-arm imaging should be routinely available.
Another two-pin technique involves placing Schanz pins into the dense supraacetabular bone with a trajectory from the AIIS toward the PSIS, or slightly more caudally directed toward the sciatic notch. This technique is slightly more technically demanding, and is safest with good imaging, since the entry point is not palpable subcutaneously, and carries a risk of inadvertent violation of the hip joint. Frames constructed in this manner are particularly effective at closing pelvic volume when some posterior stabilizing structures remain functional, minimizing vertical instability.
For widely displaced pelvic fractures with both vertical and rotational displacement, combining external fixation with skeletal traction to the limb ipsilateral to the posterior ring injury can dramatically improve alignment and allows patient to be further resuscitated until stable for definitive pelvic fixation can be safely performed. One benefit over a circumferential sheet is the unobstructed access to abdomen, which can be helpful when patients have undergone exploratory laparotomy.
Reduction of pelvic disruptions is focused on restoration of its ring-like architecture, more than anatomical repositioning of fracture fragments. Sometimes restoring the ring mandates anatomical reduction of fractures, but fractures throughout the cancellous bone of the
sacrum generally tolerate minor residual displacements with reliable healing provided gaps can be eliminated and stable fixation can be achieved.
sacrum generally tolerate minor residual displacements with reliable healing provided gaps can be eliminated and stable fixation can be achieved.
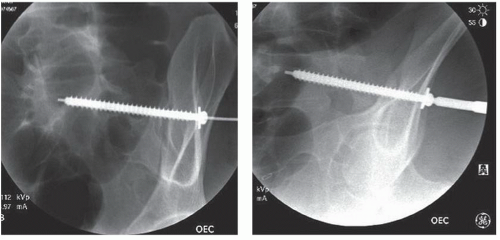
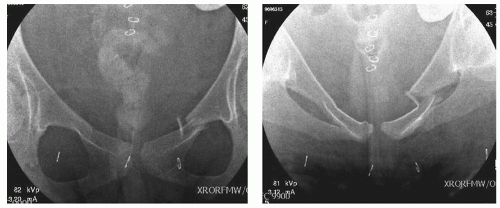
Many sacral fractures present minimally displaced, and are best characterized on CT scanning. While the exact indications for operative fixation of these injuries remain a topic of considerable controversy among surgeons, most agree that complete vertical fractures through the sacrum have some intrinsic potential to displace as patients mobilize. Addition of an examination under anesthesia to radiographic interpretation of stability found occult instability warranting internal fixation in 35% of ring disruptions from lateral compressive mechanisms which were initially classified as stable based on radiographs and computed tomography alone.1 While the decision to operate should be individualized based on a critical analysis of the fracture characteristics and clinical examination, minimally invasive techniques are particularly useful if operative treatment is deemed proper (Fig. 8.5).
Impacted sacral fractures commonly occurring from lateral impact will occasionally be associated with an internal rotation deformity of the entire affected hemipelvis. Often this is well visualized on an inlet view, but critical assessment of the outlet view may better characterize the deformity. This deformity can be rather dramatic, often with little measurable sacral fracture displacement. This pattern can be effectively reduced with Schanz screws. These are placed percutaneously in various positions, but are effective and unobtrusive to posterior ring fixation when placed from the region of the AIIS toward the PSIS or slightly more caudal toward the region of the greater sciatic notch. This can be used to manipulate the hemipelvis, but is a much more powerful instrument when combined with an additional Schanz screw in the contralateral hemipelvis and incorporated into an external fixator or used with a universal distractor, which adds the ability to compress or distract in an angular stable manner. Additional injury to the contralateral hemipelvis, sometimes occult, can diminish the effectiveness of this technique and should be aggressively sought out, as the surgeon would no longer have a “stable segment” to provide a counterforce. A purely external rotational force can be very efficiently applied via these pins and has the additional benefit of being incorporated into a two-pin “distracting frame” to provide maintenance of reduction during implant insertion without obstructing necessary imaging. More dramatic internal rotation deformities occur in conjunction with other planes of displacement, commonly flexion of the hemipelvis. This pattern of displacement is effectively reduced by altering the pin position with the pin in the stable hemipelvis being inserted from the iliac crest down the gluteus medius pillar bone (Fig. 8.6). Distraction along the trajectory created by connecting this pin to the AIIS pin either with a universal distractor or external fixation bar generates a combined extension-external rotation moment for reduction. Some also advocate the use of a table-skeletal fixation apparatus that can effectively stabilize the hemipelvis to the operating table and assist in reduction of the ring displacement.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree