Pediatric Tibial Fractures
Craig P. Eberson
DEFINITION
Fractures of the tibia are common in children.
Severity ranges from nondisplaced “toddler’s” fracture to high-energy open injury.
Open growth plates at the ends of the tibia preclude standard adult treatment options such as solid interlocked nails.
Many cases can be managed nonoperatively, but orthopaedists need to maintain familiarity with operative techniques.
ANATOMY
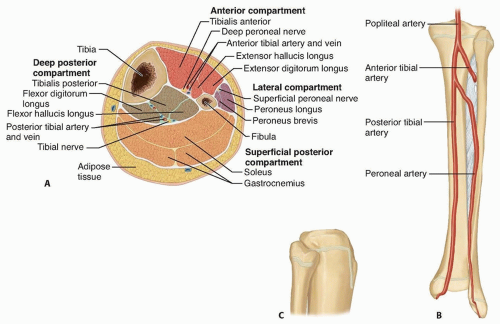
Relevant anatomy includes muscle compartments (anterior, posterior, superficial, and deep posterior), cross-sectional shape, and growth plates (FIG 1).
Neurovascular structures are at risk from direct trauma or compartment syndrome.
Understanding the anatomy of the growth plates is crucial when planning fixation techniques.
PATHOGENESIS
The most common injury scenarios are either low-energy injuries, such as those sustained during sports (twisting injury), or high-energy ones, such as seen in car versus pedestrian accidents (direct blow, comminuted fracture).
Many injuries fall somewhere along the spectrum.
High-energy injuries often are seen with concomitant injuries, such as ipsilateral femoral injuries (the so-called floating knee), compartment syndromes, and intra-articular injuries of the proximal or distal tibia.11
Occasionally, the fracture may be pathologic through an underlying bone lesion (eg, nonossifying fibroma, aneurysmal bone cyst, osteomyelitis, osteosarcoma).
As in all fractures in young children, child abuse must be suspected if the history is unclear or multiple fractures are present.
NATURAL HISTORY
Because of the significant remodeling potential in young children, most patients heal without sequelae.
Morbidity from associated injuries, however, may be significant (ie, compartment syndrome), so a thorough evaluation is of paramount importance.
General guidelines are available to define acceptable healing alignment (Table 1).
Table 1 Acceptable Deformity for Fractures of the Tibia | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||
PATIENT HISTORY AND PHYSICAL FINDINGS
The history should include mechanism of injury, antecedent pain, neurologic symptoms, and other areas of pain (eg, femur, abdominal pain, headache).
A high-energy injury should also prompt a full trauma workup using standard Advanced Trauma Life Support protocols.
The physical examination should focus on assessing initial displacement and skin condition (ie, open injury) as well as swelling of the compartments.
The limb should be splinted, in the case of gross deformity, before obtaining films using a material that permits high-quality radiographs.
A thorough neurovascular examination is needed to assess for vascular injury or compartment syndrome.1
Pulses should be palpated or obtained with Doppler assistance.
Sensation in the deep and superficial peroneal nerve and tibial nerve distributions should be assessed as well as motor function (toe flexors-extensors).
Pain with passive motion of the toes may represent an evolving compartment syndrome. More specifically, increasing pain, or pain out of proportion to the injury, is often the first early warning sign and should be taken seriously. Splitting or removal of casting material should be performed if any question exists. In young children, anxiety and fearfulness may be the presenting feature.
Compartment pressure measurements should be obtained in cases of concern (FIG 1A).
Compartment syndrome is signaled by tense swelling of the compartment, pain with gentle squeezing of the compartment, pain with passive extension-flexion of toes, and paresthesias in involved nerve distributions. Loss of pulse is a late finding.
Patients with any of these signs should be considered at risk.
A low threshold should be present for measuring compartment pressures and performing fasciotomy as needed.
Vigilance is required to prevent permanent sequelae due to missed compartment syndrome.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard anteroposterior (AP) and lateral radiographic views should be obtained.
For complex fractures, dedicated knee and ankle films can be helpful to evaluate for extension into the physeal or articular regions.
Computed tomography can be helpful to assess these regions if radiographs do not provide sufficient clarity.
Contralateral full-length films are helpful for determining length in comminuted fractures.
DIFFERENTIAL DIAGNOSIS
Isolated tibial fracture
Floating knee
Pathologic fracture
Intra-articular or intraphyseal injury
Compartment syndrome
Child abuse
NONOPERATIVE MANAGEMENT
Most tibial fractures can be managed with closed reduction and cast immobilization in an above-the-knee cast.
The cast should be molded to the anatomy of the tibia.
A supracondylar “squeeze” mold above the knee and 15 to 20 degrees of knee flexion can prevent cast slippage.
To truly avoid weight bearing, however, the cast must be flexed at least 70 to 80 degrees (if appropriate for a specific fracture).
In cases of acute fracture, the cast can be univalved or bivalved to allow for swelling. It can then be overwrapped before initiating weight bearing.
Weekly radiographs are obtained for the first 3 weeks, with the cast being wedged or changed as needed for loss of alignment.
Weight bearing is dictated by patient comfort.
The cast is changed to a short-leg or patellar-bearing cast after 4 to 6 weeks, and immobilization is continued until healing is complete.
Surgical management is required for inability to maintain satisfactory alignment (see Table 1).
SURGICAL MANAGEMENT
Indications for surgical treatment of tibial fractures in children include open injuries, compartment syndrome, multiple injuries, and fractures for which closed treatment fails.
Treatment in mature adolescents is the same as for adults with reamed, locked intramedullary nails.
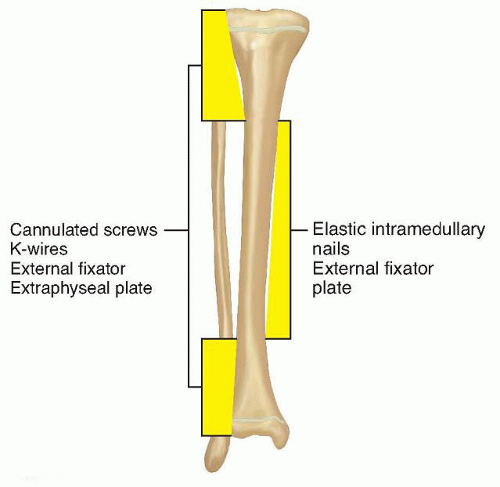
Younger children’s open physes require techniques that avoid the proximal and distal tibia, such as external fixation, plate fixation, and elastic intramedullary nailing.
Traditionally, external fixation was used primarily for fractures with significant comminution or soft tissue injury, where intramedullary fixation was considered impractical. However, recent work challenges this paradigm for surgeons experienced with elastic nailing.12
Plate fixation is a helpful technique for fractures not amenable to elastic nail fixation.
It is particularly helpful in patients who present with late loss of reduction and require an open approach to remove callus and align the fracture.
It is used at our institution primarily for distal-third fractures.
Preoperative Planning
Full-length radiographs of the tibia and fibula should be obtained.
Views of the contralateral side can be helpful to determine proper length in comminuted fractures.
A clinical examination of the well side can guide the surgeon in determining rotational alignment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree