Pediatric Hip Fractures
Ernest L. Sink
Benjamin F. Ricciardi
DEFINITION
Pediatric hip fractures comprise less than 1% of all pediatric fractures; however, appropriate management of these injuries is essential to avoid proximal femoral deformity and maintain hip joint integrity.14
ANATOMY
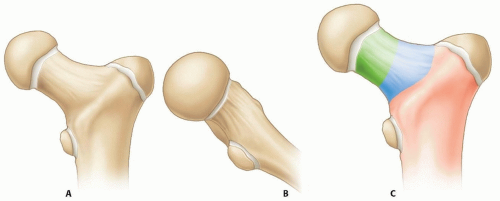
Pediatric hip fractures can occur through the physis, but more commonly, they occur through the femoral neck or intertrochanteric region. Therefore, they may be intraarticular or extra-articular (FIG 1).
The femoral head is composed of the capital femoral epiphysis, the subcapital physis, and the most proximal portion of the femoral neck
The capital femoral epiphysis begins to ossify at around 6 months in boys and 4 months in girls. The trochanteric apophysis center of ossification appears at 4 years of age in both sexes. The proximal femoral physis and trochanteric apophysis fuse at age 14 years for females and 16 years for males.
Vascular anatomy: Metaphyseal blood supply to the femoral head persists until approximately 4 years of age with primary contributions from both medial and lateral circumflex femoral branches. After 4 years of age, the lateral epiphyseal vessels, derived primarily from posteroinferior and posterosuperior branches of the medial circumflex femoral artery, are the predominant blood supply to the epiphysis of the developing hip.12
The lesser trochanter is an apophysis in the child and the insertion for the iliopsoas.
Much of the greater trochanter is apophyseal and is the insertion for many of the abductors.
NATURAL HISTORY
Pediatric hip fractures are rare injuries in children and account for less than 1% of all pediatric fractures.2
Pediatric hip fractures tend to result from high-energy trauma such as motor vehicle accident or fall from height. High rates of concomitant injury have been reported with these injuries.8
Low-energy mechanisms of injury should raise suspicion for pathologic fracture due to underlying metabolic bone disease, benign or malignant lesions, or prior trauma.15
PATIENT HISTORY AND PHYSICAL FINDINGS
History should include age, mechanism of injury (rule out child abuse in patients younger than 2 years old), locations of pain to rule out concomitant injury, and relevant medical history or family history especially in low-energy mechanism fractures suspicious for underlying pathology.
Physical examination reveals shortening and rotational deformity of the affected extremity with painful range of motion.
Infants and newborns can be challenging patients to diagnose with hip fractures due to limited ossification of the proximal
femur, and differential diagnosis may include infection and congenital dislocation of the hip. After excluding infectious etiologies, pseudoparalysis and shortening in this age group should increase suspicion of a fracture.
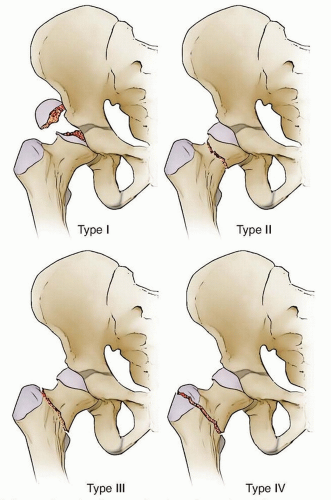
FIG 2 • Delbet classification of pediatric femoral neck fractures: type I, transphyseal; type II, transcervical; type III, cervicotrochanteric; and type IV, intertrochanteric.
Concomitant injury should be ruled out because pediatric hip fractures usually represent high-energy injuries in many cases and can be associated with neurologic, visceral, and other musculoskeletal trauma.
IMAGING AND OTHER DIAGNOSTIC STUDIES
An anteroposterior (AP) radiograph of the pelvis provides a view of the contralateral hip for comparison.
A cross-table lateral radiograph of the injured side should be considered to avoid further displacement and unnecessary discomfort from an attempt at a frog-leg lateral view.
Any break or offset of the bony trabeculae near Ward triangle is evidence of a nondisplaced or impacted fracture.
Magnetic resonance imaging (MRI) can be useful in suspected minimally displaced fractures, pathologic fractures, or stress fractures due to their improved delineation of soft tissue structures, fluid within the hip joint, and ability to assess bone marrow edema signal for nondisplaced fractures or avascular necrosis (AVN).
Ultrasound can be used to detect epiphyseal separation in infants. Additionally, it can also evaluate for a hip joint effusion in cases of suspected infection and allow concomitant aspiration.
In a patient with posttraumatic hip pain without evidence of a fracture, complete blood count, erythrocyte sedimentation rate, C-reactive protein, and temperature are helpful to evaluate for infection.
NONOPERATIVE MANAGEMENT
For patients younger than 1 year old with nondisplaced or minimally displaced fractures, management can consist of Pavlik harness or abduction brace.
For children younger than 5 years old with nondisplaced type II or III fractures, spica casting extended distal to the knee can be considered.
Contraindications
All displaced fractures
Type I fractures in children older than 2 years old
Type II or III fractures in children older than 5 years old. In children older than 5 years even without fracture displacement, internal fixation will help prevent nonunion and fracture displacement.
SURGICAL MANAGEMENT
Early operative anatomic reduction with stable internal fixation and selective use of external immobilization (spica casting) is the treatment of choice for pediatric hip fractures in the majority of patients in order to minimize rates of AVN, nonunion, and coxa vara, which are more likely to occur with nonoperative treatments.1, 3, 6, 7, 10, 14
Open reduction with stable internal fixation should be performed for any residual displacement after attempted closed reduction in order to minimize nonunion, malunion, and AVN.1, 3, 4, 6, 7, 11, 13, 14, 15
Urgent (<24 hours) reduction and decompressive capsulotomy with successful closed reductions may help reduce rates of AVN.4, 6, 11, 13, 14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree