Abstract
Objective
The objective is to study the rehabilitation management and to assess autonomy in daily life activities as well as walking recovery in patients with complicated Pott’s disease.
Patients and methods
Retrospective study in nine patients over a period of 8 years extending from 2000 to 2008, collated in the Department of Physical Medicine and Functional Rehabilitation, CHU Sahloul, Sousse, Tunisia.
Results
The mean age of our patients was 43.8 years; sex ratio was 5/4. The spine involvement of tuberculosis was dorsal in seven cases, dorso-lumbar in one patient, and multiple (cervical, dorsal and lumbar) in one case. All patients were paraplegic with a neurological involvement of the bladder. They had prior antituberculosis chemotherapy for at least 8 months. Decompression surgery was performed in six cases. Two female patients presented disorders of spinal posture during treatment requiring surgical revision with osteosynthesis. All patients received additional rehabilitation care. Following a mean duration of hospitalisation in the Rehabilitation department of 47 days with twice-daily sessions of tailored physiotherapy, three patients remained in complete paraplegia, autonomous in wheel-chair and with vesical and sphincter incontinence. The measure of functional independence (MFI) was at admission/discharge 71/92.
Conclusion
Rehabilitation takes an important place in the medico-surgical management in Pott’s disease, to limite or compensate the disabilities and handicap related to this pathology.
Résumé
Objectif
L’objectif est d’étudier la prise en charge en rééducation et évaluer l’autonomie dans les activités de la vie quotidienne et la récupération de la marche chez les patients atteints de mal de Pott compliqué.
Patients et méthodes
Étude rétrospective de neuf patients sur une période de huit ans étendue de 2000 à 2008, colligée au service médecine physique et de réadaptation fonctionnelle, CHU Sahloul, Sousse, Tunisie.
Résultats
L’âge moyen de nos patients était de 43,8 ans, le sex-ratio est 5/4. La localisation vertébrale de la tuberculose était dorsale dans sept cas, dorso-lombaire chez un patient et étagée (cervicale, dorsale et lombaire) dans un cas. Tous les patients étaient paraplégiques avec une vessie neurologique. Ils ont eu une chimiothérapie antituberculeuse pendant au moins huit mois. La chirurgie de décompression a été réalisée pour six cas. Deux patientes ont présenté au cours du traitement des troubles de la statique rachidienne ayant nécessité une reprise chirurgicale avec ostéosynthèse. Tous les patients ont eu un complément de prise en charge en rééducation. Après une durée moyenne d’hospitalisation en milieu de rééducation de 47 jours avec des séances biquotidiennes de kinésithérapie adaptée, trois malades sont restés en paraplégie complète, autonomes au fauteuil roulant et incontinents sur le plan vésicosphincterien. La mesure de l’indépendance fonctionnelle moyenne (MIF) était à l’admission/sortie (71/92).
Conclusion
La rééducation prend une place importante dans la prise en charge médicochirurgical du mal de Pott permettant de limiter ou de compenser les incapacités et l’handicap lié à cette pathologie.
1
English version
1.1
Introduction
Tuberculosis (TB) of the spine or Pott’s disease is a public health problem in underdeveloped or developing countries , representing 3 to 4% of the tuberculoses and 15% of the extrapulmonary tuberculoses . It is considered as severe because of the frequency of neurological disorders and of the importance of bone destruction, all the more since in about 80% of cases the effects are localized in the lower thoracic spine and/or in the upper lumbar spine . The diagnosis must be early in order to avoid the neurological complications and to limit infectious extension. The therapeutic management of Pott’s disease is multidisciplinary, based on a specific medical treatment, on-demand surgery and a tailored rehabilitation protocol. Few works have studied the functional result of the treatment in patients with Pott’s disease complicated with neurological lesions. The objective of our work is to study the management of rehabilitation and to assess autonomy in daily life activities and walking recovery in patients with Pott’s disease aggravated by neurological disorders after an 18 months delay.
1.2
Patients and methods
This is a retrospective study on nine patients treated for Pott’s disease in the Department of Physical Medicine and Rehabilitation of CHU Sahloul, Sousse, Tunisia, collated over 8 years, from 2000 to 2008. All our patients had neurological deficit and their etiological diagnosis was based on anatomopathological examination and positive Koch bacillus (KB) cultures. All patients have had additional ambulatory rehabilitation. A data collection sheet was designed to record information about patients’ characteristics: age, sex and socioeconomic level (low, average and high). A clinical examination was performed, indicating the neurological level reached and the micturition mode, as well as imaging including thorax, cervical and dorso-lumbar spine radiography, and magnetic resonance imaging (MRI) of the spine. The American Spinal Injury Association (ASIA) classification was used to indicate the neurological level of the patients at admission and at 18 months. Tuberculosis was histologically proven by the existence of a granulomatous tissue with caseous necrosis on biopsy of the lesions. All patients were treated by antituberculosis chemotherapy according to usual modalities and based on the use of several antituberculosis treatments among which rifampicin (10 mg/kg), isoniazid (5 to 10 mg/kg), pyrazinamid (20 to 40 mg/kg), and ethambutol (15 to 25 mg/kg) . The duration of the medical treatment and of hospitalization was indicated. Surgery was complementary, including decompression by laminectomy and evacuation of compressive abcess in case of appearance of neurological complications. In the case of surgical treatment, rehabilitation is maintained over a long period going together with the process of bone remodelling .
The rehabilitation programme was adapted according to the location of the lesion and the degree of neurological deficit as well as the functional possibilities. The spine syndrome required the help of antalgic physiotherapy and rigid adapted immobilization with corset and/or cervical collar ( Table 2 ). The management of the neurological deficit was the same as that of a patient with medulla injury and included:
- •
prevention measures of the complications of confinement to bed with adapted supports, position changes, nursing, and early verticalization on an inclined plane according to the patients’ tolerance. These measures were associated with a preventive anticoagulant treatment;
- •
global articulary work through passive, helped active or active mobilizations, and alternated postures;
- •
athletization of the upper limbs associated with breathing exercises;
- •
postures of inhibition of spasticity;
- •
management of the vesico-sphincter disorders with vesical drainage adapted to the vesical profile.
In late phase, exercises of respiratory capacity increase were started. Rehabilitation of walking ability was set up according to muscular recovery. When bone consolidation became complete, exercises aiming to increase the cardiovascular endurance were performed.
Following discharge from the department, an outpatient rehabilitation programme was started and complemented by exercises at home. The results of the neurological examination and of the autonomy of each patient were noted at admission and at the end of the rehabilitation programme. Autonomy was assessed by the Measure of Functional Independance (MFI) score. Among the 18 items, 13 were used (self care: eight, mobility and transfer: three, locomotion: two) ( Table 3 ) .
In parallel, the micturation mode of each patient was studied at admission and at discharge. A micturation calendar and intermittent sounding were used when necessary.
1.3
Results
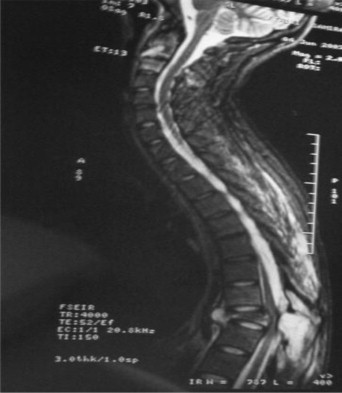
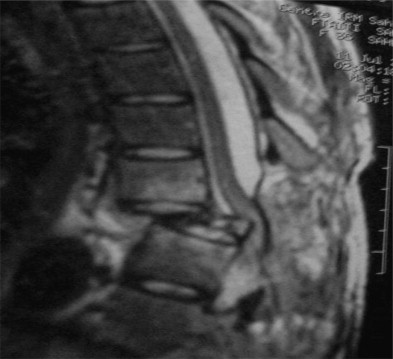
The mean age of our patients was 43.8 years, ranging from 31 to 72 years; sex ratio was 5/4. The socioeconomic level of all patients was low. The diagnosis of Pott’s disease was suspected on clinical elements: chronic sub-febrile state, inflammatory rachialgias resistant to symptomatic treatments with biological inflammatory syndrome. Radiographies ( Fig. 1 ) and medullar MRI allowed to suspect spondylodiscitis ( Figs. 2 and 3 ). Pott’s disease was confirmed by cytobacteriological and/or anatomo-pathological examination ( Table 1 ). The spine localization of the tuberculosis was dorsal in seven cases, dorso-lumbar in one case, and multiple (cervical, dorsal and lumbar) in one case. From the neurological point of view, four patients were paraplegic complete (ASIA “A”), five incomplete (one patient ASIA “B” and four others ASIA “C”) ( Table 1 ). All patients had previous antituberculosis chemotherapy, quadritherapy during two months, then bitherapy during at least ten months. Laminectomy through posterior route was performed in seven cases. Arthrodesis with secondary osteosynthesis was performed in the two patients presenting with disorders of spinal postures ( Figs. 1 and 3 ).

| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Age | 31 | 47 | 49 | 72 | 67 | 35 | 60 | 54 | 63 |
| Sex a | F | F | M | F | M | F | M | M | M |
| Level/illness | D8-D10 Paraparesis | D6-D8 Paraplegia | D10-D11 Paraplegia | D6-D7 Paraparesis | D4-D5 Paraplegia | D9, C1-C2, L2-L5 Paraparesis | D12-L1 Paraparesis | D7-D8 Paraparesis | D9-D10 Paraplegia |
| ASIA classification (admission) | B Level D8 | A level D6 | A level D10 | C level D12 | A level D4 | C level C5 | C level L3 | C level L4 | A level D9 |
| ASIA classification (after 18 months) | D | A level D6 | A level D10 | D | A level D4 | C level C5 | D | D level L4 | A level D9 |
| MRI | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Surgical treatment | No | Laminectomy with arthrodesis | Laminectomy | Laminectomy | Laminectomy | Laminectomy with arthrodesis | No | No | No |
| Cytobacteriological examination and anatomopathology | BK positive with tuberculoid granuloma b | BK positive with inflammatory granuloma | BK positive with inflammatory granuloma | BK positive with tuberculoid granuloma | BK positive with tuberculoid granuloma | BK positive with inflammatory granuloma | BK positive with tuberculoid granuloma | BK positive with tuberculoid granuloma | BK positive with tuberculoid granuloma |
| Medical treatment | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Duration of hospitalization (days) | 42 | 35 | 63 | 70 | 45 | 32 | 34 | 50 | 54 |
All patients had a neurogenic bladder ( Table 2 ). Resorting to intermittent sounding (IS) was noted in seven cases. Two patients out of nine refused resorting to IS. Three patients recovered spontaneous micturation, two patients remained on IS, and two other patients stopped IS for intolerance. The mean duration of hospitalization was 47 days. Three patients were still paraplegic, autonomous in wheel chair. Six patients had recovered walking ability, three of whom with the help of a walking frame. Three patients were autonomous in their daily life activities and had resumed work. The mean MFI at admission was 71, and at discharge, 92 ( Table 3 ).
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Micturition mode | |||||||||
| At start | IS | IS | IS | IS | IS | Peniflow | IS | Peniflow | IS |
| After 18 months | Complete autonomy | IS | Peniflow | Complete autonomy | Permanent sounding | Peniflow | Complete autonomy | Peniflow | IS |
| Immobilization | Neofract dorsal corset | Neofract dorsal corset | Neofract dorsal corset | Neofract dorso-lumbar corset | Neofract dorsal corset | Neofract dorso-lumbar corset + C4 cervical collar | Neofract dorso-lumbar corset | Neofract dorso-lumbar corset | Neofract dorsal corset |
| Walking ability admission/discharge | Paraparesis/Walking | Paraplegia/Wheel chair | Paraplegia/Wheel chair | Paraparesis/Walking | Paraplegia/Walking with frame | Paraparesis/Walking with frame | Paraparesis/Walking | Paraparesis/Walking with frame | Paraplegia/Wheel chair |
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | |
|---|---|---|---|---|---|---|---|---|---|
| MFI (admission/discharge) | 86/112 | 70/73 | 72/78 | 72/108 | 68/94 | 74/92 | 82/104 | 72/94 | 60/70 |
| Self care (56 points) (admission/discharge) | 25/50 | 20/22 | 21/23 | 20/46 | 18/34 | 23/32 | 21/42 | 20/33 | 12/19 |
| Mobility, transfer (21 points) (admission/discharge) | 18/17 | 9/10 | 10/12 | 10/17 | 9/15 | 10/15 | 18/17 | 11/16 | 8/10 |
| Locomotion (14 points) (admission/discharge) | 7/10 | 6/6 | 6/8 | 7/10 | 6/10 | 6/10 | 7/10 | 6/10 | 5/6 |
1.4
Discussion
Tuberculous spondylodiscitis or Pott’s disease corresponds to the infection of the intervetebral disc of the adjacent vertebrae . It is on the increase on some specific grounds (immunodepression). The onset of this pathology is most often misleading with an insidious clinical picture possibly resulting in a delayed diagnosis. This explains the collapse of the vertebrae, the kyphoses sometimes encountered as well as the disorders of spinal posture it may generate . We performed an arthrodesis in two patients for spinal posture disorders.
Neurological examination must be the most complete possible, exploring all sub-lesional metameres, since the neurological signs are variable .
The neurological deficit depends on the extension of the infectious process, the body collapse and the epidural extension . These elements are in direct relation with delay of the diagnosis; the importance of the spinal and neurological injuries in our patients could be explained by delays in diagnosis. Vesical and sphincter disorders must be looked for. They are of urinary incontinence type, dysuria, or even isolated pollakiuria. Resorting to a calendar of micturation and to intemittent sounding was important to clear the urine and preserve the upper urinary tract . In our series, three patients recovered vesical and anal autonomy. This improvement went together with early recovery of the global neurological deficit.
Standard radiographies may be normal at initial stage . MRI allows suspecting the diagnosis at an early stage by precising the localization of the infection, unique or multiple, its bone, vertebral, discal, epidural or paravertebral extension . MRI can detect potential complications (abcess) likely to benefit from decompression surgery or percutaneous drainage gesture . It finally allows guiding towards biopsy for an anatomopathological and cytobacteriological examination .
Initial immobilization of the injured spinal segment, by corset, cervical collar or even sometimes strict rest in bed is recommended. In the Yilboudo series, a plaster corset was associated in seven patients to prevent graft expulsion . Surgery was not systematic and was indicated for neurological disorders or for disorders of spinal posture . It consisted in posterior decompression by laminectomy and a posterior arthrodesis aiming to stabilize the deformities and especially the local kyphosis. Some authors resorted to surgery in view of some voluminous pottic abcesses and fistulated abcesses . The initial immobilization in bed is indicated in the dorsal and lumbar forms. Attention must be given to the appearance of complications of the decubitus, which may aggravate the prognosis, especially at the starting phase . In case of important neurological complications, the programme of specific rehabilitation is that of a patient with medullary injury, aiming to acquire optimal autonomy according to the remaining functional capacities depending on the level of medullar lesion and on the complete, incomplete, spastic or flabby characteristics of the paraplegia . MFI is therefore important , in order to assess the level of functional recovery. Rehabilitation must be soft and adapted to the functional and recovery level. The verticalization must be early and progressive. The physiotherapy aims to prevent the decubitus complications, as well as to keep the articular, muscular, trophic, respiratory functions operational, and to work on the transfers. The muscular reinforcement of the four limbs, of the cervical, lumbar spine, is associated with an axial counter-resistance self-extension . Some patients need an equipment like a wheel-chair, a walking frame and crutches. This programme is completed with work on walking ability and proprioception according to the neurological damage and the recovery, with posture reprogramming and re-training to effort. Ergotherapy participates to a gain of optimal autonomy, adaptation to environment and to daily life . The patient attends training on healthy life conditions.
According to Yilboudo et al. , the functional recovery level varied between 50 and 60% after surgical treatment, but autonomy was not specified. Other authors report a recovery level of 87% for Moon and 88% for Rezai . In the Benzagmout series , out of 37 patients with Pott’s disease, 6 had neurological signs, seven had surgery of whom 6 for medullary compression signs, and one for a bilateral psoas abcess. All patients who had surgery recovered walking ability. In our series, surgical treatment was indicated in five cases out of nine, walking recovery was of 60% vs. 75% in the patients without surgery. This difference is probably explained by the fact that our patients often present at an advanced stage of anatomo-clinical lesions with insidious clinical symptoms and a low socio-economical level, and surgery takes a long time to be performed. Earliness of the diagnosis appears essential for decreasing the complications, decreasing the recourse to surgical treatment and speeding up the recovery of a good autonomy. The recourse to that surgery could be beneficial, but it is dependant on the technical capacity, the intensive care means, and the surgeon’s experience. Finally, the surgical approach is not universally standardized. Prospective studies are necessary to define the steps of this surgical approach.
1.5
Conclusion
Vertebral tuberculosis is still a widespread illness in the developing countries. The complications of the illness may be devastating on the ground of its capacity to cause bone destruction, spine deformity and paraplegia or tetraplegia. Hence, an early diagnosis and the set up of a treatment are necessary to hope for a good result.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
La tuberculose (TBC) de la colonne vertébrale, ou mal de Pott, constitue un problème de santé publique dans les pays sous-développés et en voie de développement . Elle représente 3 % à 5 % des tuberculoses et 15 % des tuberculoses extra pulmonaires . Elle est considérée comme grave à cause de la fréquence des troubles neurologiques et de l’importance de la destruction osseuse d’autant plus que l’atteinte siège dans environ 80 % des cas au rachis thoracique bas et/ou rachis lombaire haut . Le diagnostic doit être précoce à fin d’éviter les complications neurologiques et de limiter l’extension infectieuse. La prise en charge thérapeutique du mal de Pott est multidisciplinaire. Elle est basée sur un traitement médical spécifique, une chirurgie à la demande et un protocole de rééducation adapté. Peu de travaux publiés ont étudié le résultat fonctionnel du traitement des patients atteints de mal de Pott compliqué de lésions neurologiques. L’objectif de notre travail est d’étudier la prise en charge en rééducation et évaluer l’autonomie dans les activités de la vie quotidienne et la récupération de la marche chez les patients atteints de mal de Pott avec atteintes neurologiques après un délai de 18 mois.
2.2
Patients et méthodes
Il s’agit d’une étude rétrospective portant sur neuf patients traités pour mal de Pott dans le service de médecine physique rééducation et réadaptation fonctionnelle du CHU Sahloul de Sousse en Tunisie, colligée sur une période de huit ans de 2000 à 2008. Tous nos patients avaient un déficit neurologique et leurs diagnostics étiologiques étaient basés sur un examen anatomopathologique et des cultures de bacille de Koch (BK) positif. Tous les patients avaient eu un complément de rééducation en ambulatoire. Une fiche de recueil des données était élaborée pour relever les informations concernant les caractéristiques des patients : âge, sexe, niveau socioéconomique (bas, moyen et haut). Un examen clinique précisant, le niveau neurologique atteint et le mode mictionnel, une imagerie comprenant des radiographies du thorax, du rachis cervical, dorsolombaire et une imagerie par résonance magnétique du rachis(IRM). La classification « the American Spinal Injury Association (ASIA) » a été utilisé pour préciser le niveau neurologique des patients à l’admission et à 18 mois. La tuberculose a été prouvée histologiquement par l’existence d’un tissu granulomateux avec nécrose caséeuse à la biopsie des lésions. Tous les patients étaient traités par une chimiothérapie antituberculeuse, selon les modalités habituelles et basée sur l’utilisation de plusieurs antituberculeux parmi lesquels la rifampicine (10 mg/kg), l’isoniazide (5 à 10 mg/kg), le pyrazinamide (20 à 40 mg/kg) et l’éthambutol (15 à 25 mg/kg) . La durée du traitement médical et de l’hospitalisation ont été précisée. La chirurgie a été complémentaire, comportant une décompression par laminectomie et l’évacuation d’abcès compressifs devant l’apparition de complications neurologiques. Dans le cas où le traitement est chirurgical, une rééducation est poursuivie durant une longue période accompagnant le processus de remodelage osseux .
Le programme de rééducation a été adapté selon le siège de la lésion et le degré du déficit neurologique ainsi que les possibilités fonctionnelles. Le syndrome rachidien avaient nécessité le recours à des moyens de physiothérapie antalgiques et une immobilisation rigide adapté par corset et ou minerve ( Tableau 2 ). La prise en charge du déficit neurologique a été assimilée à celle d’un blessé médullaire et avaient comporté :
- •
des mesures de préventions des complications d’alitements avec des supports adaptés, des changements de positions, des soins de nursing et une verticalisation précoce sur plan incliné selon la tolérance des patients. Ces mesures ont été associées à un traitement anticoagulant préventif ;
- •
un entretien articulaire global par des mobilisations passives, actives aidés ou actives et des postures alternés ;
- •
une athléthisation des membres supérieurs associé à des exercices de gymnastiques respiratoires ;
- •
des postures d’inhibition de la spasticité ;
- •
une prise en charge des troubles vésicosphinctériens avec un drainage vésical adapté au profil vésical.
À la phase tardive, des exercices d’augmentation de la capacité respiratoire ont été démarrés. La rééducation de la marche a été entamée en fonction de la récupération musculaire. Quand la consolidation osseuse devenait complète, il était effectué des exercices pour augmenter l’endurance cardiovasculaire.
À la sortie du service, un programme de rééducation a été entamé en ambulatoire et complété par des exercices à domicile. Les résultats de l’examen neurologique et de l’autonomie de chaque patient étaient notés à l’admission et à la fin du programme de rééducation.
L’autonomie a été évaluée par l’étude du score mesure de l’indépendance fonctionnelle (MIF). On a utilisé 13 items parmi 18 items (soins personnels : huit, mobilité et transfert : trois ; locomotion : deux) ( Tableau 3 ) .
Parallèlement, le mode mictionnel de chaque patient était étudié à l’admission et à la sortie. Un calendrier mictionnel et un sondage intermittent (SI) ont été utilisés au besoin.
2.3
Résultats
L’âge moyen de nos patients était de 43,8 ans avec des extrêmes entre 31et 72 ans, le sex-ratio est 5/4. Le niveau socioéconomique de tous les patients était bas. Le diagnostic de mal de Pott a été suspecté sur des éléments cliniques ; un état subfébril chronique, des rachialgies inflammatoires résistantes aux traitements symptomatiques avec un syndrome inflammatoire biologique. Les radiographies ( Fig. 1 ) et l’IRM médullaire permettaient d’évoquer une spondylodiscite ( Fig. 2 et 3 ). Le mal de pott était confirmé par un examen cytobactériologique et/ou anatomopathologique ( Tableau 1 ). La localisation vertébrale de la tuberculose était dorsale dans sept cas, dorso-lombaire chez un patient et étagée (cervicale, dorsale et lombaire) dans un cas. Sur le plan neurologique, quatre malades étaient paraplégiques complets (ASIA « A ») et cinq incomplets (un patient ASIA « B » et quatre autres ASIA « C ») ( Tableau 1 ). Tous les patients avaient eu une chimiothérapie anti tuberculeuse, une quadrithérapie pendant deux mois puis bithérapie pendant au moins dix mois. Une laminectomie par voie postérieure a été réalisée pour sept cas. Une arthrodèse avec ostéosynthèse secondaire a été réalisée chez les deux patients qui ont présenté des troubles de la statique rachidienne ( Fig. 1 et 3 ).









