Most people with amputations should not experience pain that interferes with their quality of life or requires regular medication more than 6 months following the amputation surgery. In fact, most people with amputations do not experience significant pain more than 3 months following the amputation. However, the clinician must specifically define what these patients mean when they relate that they have pain. The pain must be carefully differentiated to treat it properly. Most problematic pain that is present more than 6 months after amputation is related to a poorly fitting prosthesis and should be labeled as residual limb pain.
Key points
- •
The clinician must specifically define what patients with amputations mean when they relate that they have pain.
- •
The most common causative factor for residual limb pain is with the prosthetic fit.
- •
Standard pain medications can be useful in the acute postoperative period to control the postsurgical pain.
- •
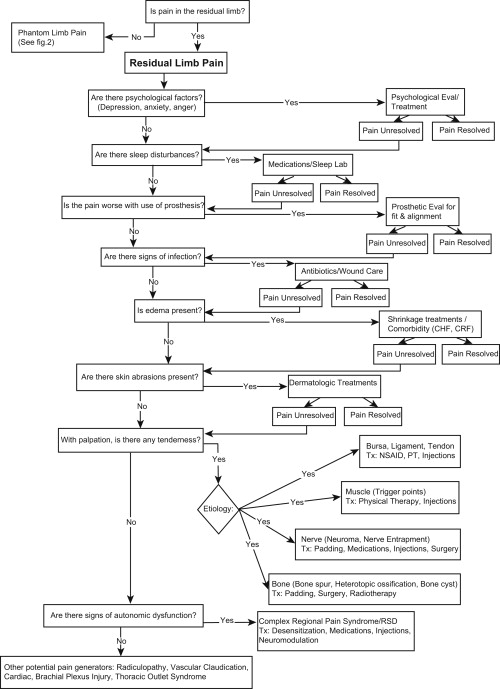
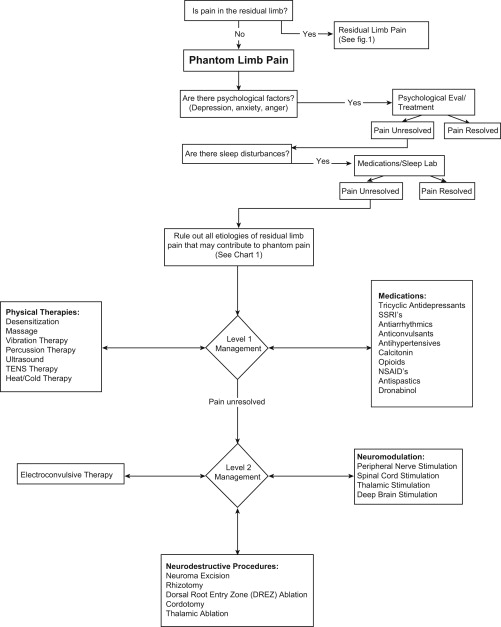
The use of a pain treatment algorithm for the person with an amputation who is experiencing pain can provide a rational guide for the progression of treatment options.
Most people with amputations should not experience pain that interferes with their quality of life or requires regular medication more than 6 months following the amputation surgery. In fact, most people with amputations do not experience significant pain more than 3 months following the amputation.
However, the clinician must specifically define what patients with amputations mean when they relate that they have pain. The pain must be carefully differentiated to treat it properly. By far, most problematic pain that is present more than 6 months after the amputation is related to a poorly fitting prosthesis and should be properly labeled as residual limb pain. This practice gets the treating physician to differentiate between nociceptive versus neuropathic pain. The most commonly used treatments can fit into 5 general categories: (1) medications, (2) prosthetic changes, (3) psychosocial treatments, (4) noninvasive therapies (ie, physical therapy, pain modalities), and (5) surgery.
Most people with acquired amputations experience phantom limb pain, at least in the acute postoperative period. This pain is carefully defined as pain that is present in the part of the limb that has been removed and not in the tissues of the limb that is remaining. Most often, this pain subsides but may be present for a split second on occasion throughout the life of people with amputations. Usually, however, it significantly decreases and does not require treatment beyond 3 months after the amputation surgery. It is also important that the phenomenon of phantom sensation be differentiated from phantom pain. Most people with acquired amputations will experience some phantom sensation throughout their lives. However, the amount of phantom sensation will usually diminish over time. This experience is described as feeling that the amputated portion of the limb is still present. With time, the distal end of the limb (hand or foot) will move closer to the end of the residual limb, which is called telescoping . It is important to explain this experience to the patients with new amputations so they better understand that it is a real phenomenon that is to be expected and that will change over time.
Residual limb pain is defined as pain that is present in some part of the limb that remains following the amputation. There are a variety of potential causes of this type of pain, and these require a careful history and investigation in order to provide a treatment approach that is likely to decrease the pain and not result in chronic medication use or opiate addiction.
One of the presently confounding things in pain treatment are the number of medications and modalities that are available for use to try to diminish the pain experience. Sherman wrote about many of these modalities in the 1970s and 1980s. Most of these treatments are in use today, but now we have many more treatment options to try. One of the problems in treatment is the physicians themselves. We now have a subspecialty in pain management, and many of these physicians do not have extensive knowledge in musculoskeletal anatomy, kinesiology, proper prosthetic fitting techniques, or the mechanics of prosthetic function or gait analysis. All of these areas enter into the proper assessment and treatment of people with amputations who have pain. Another issue in pain treatment is the need for careful follow-up and treatment coordination. There is a tendency to shotgun treatment rather than take time to carefully try one modality before adding another treatment or several treatments at a time. Thus, the pain treatment algorithm for the person with an amputation has been developed ( Figs. 1 and 2 ).
In addition to specific treatment modalities, there are several lifestyle changes that will assist to diminish the pain experience. These changes can be more difficult to achieve than simply providing a medication or a transcutaneous electrical stimulation (TENS) unit. These changes include the following: (1) cessation of smoking, (2) decrease in stress, (3) decrease in depression, (4) control of edema, (5) distraction from the pain, and (6) increasing activity level.
Residual limb pain
The most common causative factor for residual limb pain is with the prosthetic fit. In an amputation with prosthetic restoration, pressures are put on tissues of the remaining leg or arm that were not designed to be pressure bearing. Most sockets require an intimate fit to provide maximum function and provide pressure points that can often be uncomfortable or painful. For the people with transtibial leg amputations, these points are often the fibular head or the distal anterior kick point. In people with transfemoral amputations, this point is usually the distal lateral area where the distal femur comes in contact with the lateral socket wall. This point of contact is essential for keeping the pelvis as level as possible during the stance phase of the above-knee prosthesis. In the arm prostheses, it is often the distal ends of the radius and ulna for people with transradial amputations and the distal anterior end of the humerus for people with transhumeral amputations.
Residual limb pain may be caused when the socket exerts excess pressure on the residual limb soft tissues, especially on nerves or a neuroma that has formed at the cut end of a peripheral nerve.
In some cases, residual limb pain is a result of the underlying bone changes that could be bony overgrowth from the margins of the cut bone or the development of heterotopic bone within the soft tissues of the residual limb. These painful bone growths may require surgical removal.
An additional consideration for pain generation in the person with an amputation should be musculoskeletal imbalance. All people with amputations have an alteration in their usual body mechanics. Often this results in a musculoskeletal imbalance that is often seen in a change in their posture. It is common that myofascial pain becomes a secondary source of pain in the affected extremity or the contralateral extremity.
Last but not least as a cause for residual limb pain is the presence of the pathophysiology that caused the amputation. Is there a peripheral neuropathy that is causing the pain? Was there a nerve insult during the traction injury that led to the amputation? Is there claudication because of the original dysvascular disease that caused the amputation? Has the tumor that required the amputation returned? Is infection brewing within the bone or soft tissues, which is causing the residual limb pain?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






