Osteoarthritis of the Spine
Sanford E. Emery
Vytautas M. Ringus
Cervical Spine
Pathoanatomy
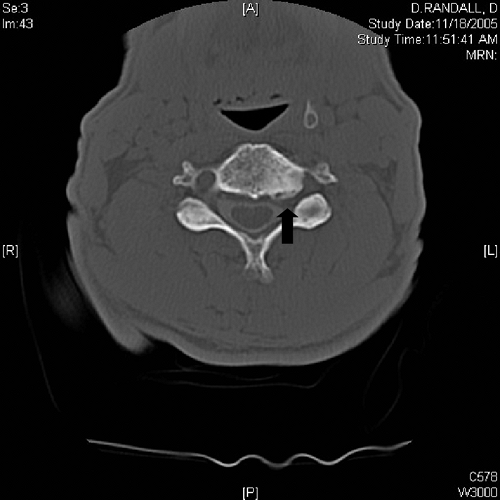
Osteoarthritis (OA) of the cervical spine is primarily a result of aging changes related to disk degeneration.1,2 Progressive loss of proteoglycans, particularly chondroitin sulfate, leads to slow desiccation of the disk. Small microfissures or frank herniation of the nucleus pulposus occurs with resultant settling and alteration of the biomechanical environment of that motion segment. The osseous structures respond with spur formation where the annular fibers insert near the end plate, in the facet joints, and importantly, at the uncovertebral joints. Chondro-osseous spurs at these uncovertebral regions narrow the foramen and commonly cause nerve root impingement. These degenerative changes of the cervical spine are termed cervical spondylosis. Other pathoanatomic changes that can be associated with cervical spondylosis are herniated disks, dynamic instability, and kyphosis, all of which can be important clinically (Fig 22-1A, B).
Clinical Syndromes
Cervical Radiculopathy
The most common clinical manifestation of OA in the cervical spine that may require surgical consideration is termed cervical radiculopathy. This denotes nerve root compression, typically from hard disk and osteophytic changes, although soft disk herniations certainly occur in the arthritic neck (Fig. 22-2). The hallmark of cervical radiculopathy is arm pain. This is often associated with neurologic symptoms, such as weakness or paresthesias. In most patients, cervical root impingement produces axial neck pain as well. Neck tenderness and limited range of motion are typically found on physical examination. A full neurologic examination should be performed, looking for motor weakness and sensory findings as well as evidence of hyporeflexia.3 Symptoms and signs may suggest a specific root involvement, but neuroradiologic corroboration is necessary. The C5-6 disk and C6-7 disk are most commonly involved with cervical spondylosis, probably because these two segments have the greatest range of motion and sustain the highest loads in the cervical spine.
Cervical Myelopathy
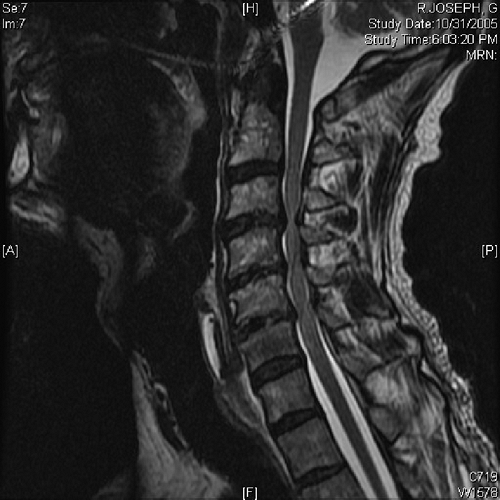
If disk herniations, osteophytes, kyphosis, or instability causes spinal cord compression, myelopathy can result (Fig. 22-3).4,5 Chronic cord compression can lead to demyelinization and ultimately cell death. This occurs first in the central gray matter where the small transverse end-arterioles provide less blood supply and only later in the white matter tracts. The earliest symptoms of cervical myelopathy are often subtle changes in gait or balance. Subjective arm or leg weakness as well as global numbness of the arms or hands is common in more moderate to severe cases. Although most patients do have neck and often arm pain, one series documented an approximately 15% incidence of no pain in patients with cervical myelopathy, so this should not confuse the clinician in the diagnostic work-up.6
Physical examination should include full neurologic testing to look for motor weakness, sensory changes, and long tract signs (Hoffmann, Babinski, and clonus). Gait and balance should also be tested, such as toe-walking, heel-walking, and toe-to-heel tandem gait (walking a tightrope). An isolated reflex may be decreased because of anterior horn cell necrosis or concomitant root impingement, but patients with myelopathy are generally hyperreflexic with the pathologic reflexes noted before.
 Figure 22-1A A lateral radiograph of a normal cervical spine. There is normal disc height at each level and no evidence of osteophytic changes. |
Neck Pain Alone
Many patients with cervical spondylosis have neck pain without symptoms or signs of radiculopathy or myelopathy. In patients with cervical spondylosis, this axial neck pain is usually from degenerative disks or facet arthritis. At times, patients with moderate to severe cervical stenosis from spondylotic changes have significant neck pain
but no evidence of myelopathy or radiculopathy on examination.7 This is a reason to consider neuroradiologic investigation of patients with significant, debilitating neck pain alone because if stenosis is present, it can be surgically addressed with good results.
but no evidence of myelopathy or radiculopathy on examination.7 This is a reason to consider neuroradiologic investigation of patients with significant, debilitating neck pain alone because if stenosis is present, it can be surgically addressed with good results.
Diagnostic Evaluation
Plain radiographs remain the cornerstone of the diagnostic work-up for OA of the cervical spine.8 Disk space narrowing, posterior osteophytes, and size of the spinal canal can be determined from a plain lateral radiograph. Oblique films can visualize foraminal spurring, although they are not routinely necessary. Flexion and extension lateral views are helpful and can pick up instability that may not be evident on a neutral lateral view.
The next diagnostic study in symptomatic patients is magnetic resonance imaging (MRI). This modality provides excellent visualization of the soft tissues, including disks and the neural elements.9,10,11 Bone detail, such as osteophytic ridging, can be seen but not to the extent that computed tomographic (CT) imaging allows. Plain CT scans do not show the neural structures adequately, so if further evaluation is needed, myelography plus CT-myelography is recommended. A well-done myelogram can demonstrate root impingement that may not be appreciated on MRI. CT-myelography delineates cord compression as well; often these more invasive studies are obtained to decide which levels need to be included in multilevel fusion procedures.
Electrodiagnostic studies can be helpful in confirming cervical radiculopathy or clarifying peripheral nerve entrapment syndromes, such as carpal tunnel or thoracic outlet syndrome. Brachial plexopathy is another entity that can mimic acute cervical radiculopathy in which evaluation by electromyography and nerve conduction velocity studies is useful. In straightforward cases of cervical radiculopathy or stenosis, however, electrodiagnostic studies are not necessary. These tests are of little or no value in the diagnostic work-up of cervical myelopathy.
Nonoperative Treatment
For patients with cervical radiculopathy or neck pain alone, there are three main nonoperative treatment measures: 1) soft collar immobilization, 2) anti-inflammatory medication, and 3) physical therapy modalities including traction.
A soft collar limits extremes in range of motion and rests the overworked paraspinal musculature. Nonsteroidal medications are initially used, and a short steroid taper can be effective for pinched nerve symptoms. Physical therapy methods of heat, ultrasound, and massage may relieve some muscle symptoms as well; traction can sometimes promote resolution of radicular symptoms, particularly in younger patients. With home traction kits, care should be taken to instruct patients to “face the door” in traction with use of a rope and water bag; this ensures slight flexion of the neck rather than extension, the latter of which closes down the spinal canal and usually exacerbates the symptoms. Epidural steroid injections are performed at some centers, but the physician must be well trained in this technique given the proximity of the spinal cord; patients with a narrow spinal canal should probably avoid injection treatments in the cervical spine.
Patients with cervical myelopathy are more difficult to treat nonoperatively because frank spinal cord compression is present. A soft collar and nonsteroidal anti-inflammatory medications may be used for pain flare-ups, but traction or manipulation should be avoided. Symptoms and documented cord impingement consistent with moderate to severe myelopathy are generally treated operatively.
Indications for Surgery
Patients with neck pain alone from spondylotic changes are preferably managed with anti-inflammatory medications and physical therapy measures as needed. At times, however, patients without radiculopathy or myelopathy but with significant, intractable neck pain have cervical stenosis. This subset of patients with neck pain only responds well to anterior decompression and fusion, provided that months of nonoperative treatment efforts have failed.12
Symptoms of radiculopathy from a soft disk herniation or spondylosis usually resolve in 2 to 3 months with (or often without) treatment. If pain persists longer than this and if nonoperative measures have failed, and the symptoms are not tolerable for the patient, surgery is indicated.13 Mild weakness can be observed closely and often resolves as well. Moderate to severe weakness with substantial pathologic changes on neuroradiologic studies may need decompression to optimize neural recovery. Patients with mild cervical myelopathy may remain stable for years and can be observed. They should have long-term follow-up, however, because the natural history of myelopathy in the majority of patients is slow, stepwise deterioration.14,15 If moderate to severe myelopathy is present with cord compression evident on studies, surgical decompression is indicated to at least stabilize and usually improve the neurologic status of the patient.
Surgical Treatment
Anterior Approach
For many spine surgeons, the anterior surgical approach is the preferred method for operative treatment of degenerative conditions of the neck.6,16,17,18,19 Because most spinal cord or nerve root compression is anterior as a result of ridging of the vertebral end plates, disk herniations, or uncovertebral hypertrophy, the anterior approach is a direct way of removing the pathologic process and relieving compression. It is useful for patients with radiculopathy, myelopathy, instability, and deformities such as kyphosis.20
The most commonly performed procedure is the anterior cervical discectomy and fusion (ACDF). This technique can well address pathologic changes limited to the disk space or adjacent end plates. The operative approach is through the fascial planes of the anterior neck and is straightforward.21 After decompression of the neural elements, the
end plates are abraded with a burr to provide a raw bleeding surface, which increases the fusion rate.22 A horseshoe- shaped tricortical iliac crest bone graft is harvested from the patient’s iliac crest and carefully fitted into place after some gentle distraction of the disk space. With successful arthrodesis, that segment is stabilized and foraminal height is maintained. Autograft has superior healing properties;23 however, many surgeons use allograft in one-level ACDF procedures or in instrumented cases; good results have been reported with allograft material.24,25,26,27
end plates are abraded with a burr to provide a raw bleeding surface, which increases the fusion rate.22 A horseshoe- shaped tricortical iliac crest bone graft is harvested from the patient’s iliac crest and carefully fitted into place after some gentle distraction of the disk space. With successful arthrodesis, that segment is stabilized and foraminal height is maintained. Autograft has superior healing properties;23 however, many surgeons use allograft in one-level ACDF procedures or in instrumented cases; good results have been reported with allograft material.24,25,26,27
Anterior Plate Fixation
Anterior instrumentation of the cervical spine for degenerative conditions has increased in popularity during the past 10 years. Initially developed for use in traumatic injuries, anterior plates can help stabilize the grafted segments in degenerative disease and promote a higher fusion rate for multilevel ACDF procedures (Fig. 22-4).28,29,30,31,32 Their use may also decrease the need for rigid postoperative bracing. Anterior instrumentation is typically used for two- or three-level ACDF procedures. One-level anterior cervical ACDF operations have a high union rate, and though many surgeons use a plate in these cases, in the absence of other circumstances such as adjacent fused levels,33 history of a pseudarthrosis, or smoking, a plate is probably unnecessary.34 As with any instrumentation, there is some increased risk of loosening and malposition or the need to remove the plate on rare occasions.35
Anterior Cervical Corpectomy and Strut Graft Fusions
For many patients with severe degenerative conditions, particularly those with spinal cord compression and myelopathy, ACDF techniques alone may not address all the compressive disease. Many patients with cervical spondylotic myelopathy or ossified posterior longitudinal ligament may need one or more corpectomies followed by a longer strut graft placement.6,36,37,38,39
Corpectomy procedures are designed to remove compressive disease behind the vertebral bodies. The initial exposure and technique are similar to those for ACDF. For a corpectomy, the middle portion of the vertebral body is removed. This is often done over two or three levels, because many patients with severe spondylosis have multilevel disease. This long channel is then spanned with a strut graft. Anterior instrumentation is useful for one-level corpectomy and strut grafting procedures; however, longer constructs become biomechanically unfavorable for long anterior plates,40,41 and patients with these long reconstruction procedures need rigid bracing to protect the graft and maximize healing. Concomitant posterior fusion may be performed to maximize stability with circumferential arthrodesis (Fig. 22-5).42 These are often complex procedures in patients with severe myelopathy and should be performed by spine surgeons with experience in this area and with significant ancillary backup, such as spinal cord monitoring.
Posterior Approach
The simplest posterior approach is that for a lateral soft disk herniation.43,44,45 A keyhole laminotomy is performed by thinning a lamina with a burr. Then, using a Kerrison rongeur to perform a foraminotomy, the surgeon visualizes the takeoff of the nerve root. Epidural veins need to be controlled, and the disk can be incised by gently retracting the nerve root cephalad. If most of the facet joint has been preserved, no fusion is needed and the patient can use a soft collar postoperatively for comfort. If there is any cord deformation, the posterior laminotomy approach is typically avoided because the herniated disk is more safely accessible from an anterior approach.
For multilevel spondylotic disease with cervical stenosis, a laminectomy can be performed.46,47 This procedure should be reserved for patients without deformity or pre-existing instability and for those with severe anterior cord impingement.48 Because of the difficult problem of postlaminectomy kyphosis in some patients who have had multilevel laminectomies, a technique called laminoplasty has evolved in the last 20 years. This was developed in Japan to address severe cord compression in patients with continuous ossified posterior longitudinal ligament. Its indications have expanded to include patients with cervical spondylotic myelopathy. Laminoplasty is a canal-expanding procedure in which the posterior laminae are hinged open and held there by bone grafts or suture until healing occurs (Fig. 22-6).49,50,51,52,53 The spinal canal is then enlarged and cervical stenosis thus relieved. Laminoplasty is a satisfactory technique for patients with normal lordosis (so the spinal cord can float posteriorly),54,55 with no instability, and without significant neck pain. Because the soft tissues can heal to a residual bone roof, the incidence of postoperative kyphosis has decreased. A laminoplasty is not as technically demanding as long anterior corpectomy and strut graft procedures are, and does not require a fusion. Both laminoplasty and anterior decompression and strut graft methods have had satisfactory neural recovery rates.36,56 Corpectomy and strut grafting procedures can correct deformity and stabilize the neck; they seem to have better pain results than those suggested by laminoplasty reports.6,57
Results
Both anterior and posterior decompression procedures have been demonstrated to provide satisfactory neurologic recovery.55 Patients with cervical spondylosis and radiculopathy can achieve particularly good results with anterior cervical ACDF techniques.16,58,58,60 Patients with cervical spondylotic myelopathy often require longer, more extensive decompression procedures, either anterior or posterior.61 Improvement can be expected in most of these patients with myelopathy, resulting in increased strength, improved gait, and better overall function.6,37,39,62 Neurologic recovery in patients with myelopathy largely depends on the degree of myelopathy existing preoperatively as well as other factors, including degree of cord compression on preoperative studies and duration of symptoms.
Pain relief for patients undergoing cervical spine procedures for degenerative disorders is most consistent for arm pain. For patients with significant arthritic changes in the neck, we prefer anterior decompression and fusion for best relief of pain, although posterior laminotomy and discectomy with or without a foraminotomy can provide good results for radiculopathy as well. Whereas radicular pain is relieved in approximately 90% of patients, axial neck pain can be expected to be relieved in approximately 80% of patients.16,63,64 In the older population, certainly other degenerative levels can contribute to persistent axial symptoms. Patients with recurrent pain after fusion procedures should be evaluated to rule out a pseudarthrosis or problems at adjacent levels.
Thoracic Spine
Due to the rib cage, the thoracic spine is more stable and has less range of motion than the other regions of the spine. This added stability results in less degenerative changes and less clinical problems than seen in the cervical or lumbar areas. Certainly degenerative disc disease does occur in thoracic levels and some facet changes can occur, however, these aging changes are usually well tolerated. There are two main clinical syndromes that result from degenerative changes of the thoracic spine: thoracic disc herniations and thoracic spinal stenosis.
Thoracic Disc Herniations
Presumably due to less motion and lower loads, thoracic disc herniations are less frequent than those in the lumbar or even cervical regions. Clinicians have become more
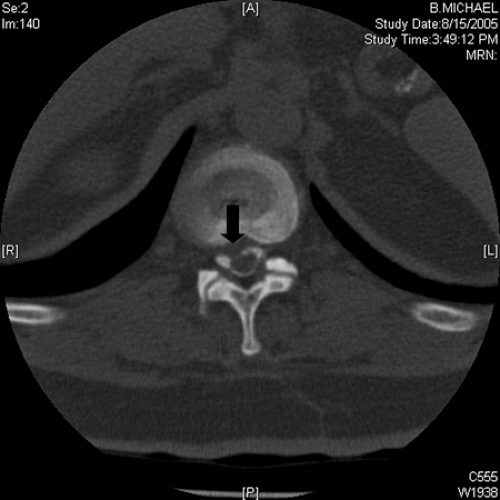
aware of thoracic disc pathology, however, since the introduction of MRI technology and the ability to easily image this area (Fig. 22-7). As with disc herniations anywhere in the spine, thoracic disc herniations are usually asymptomatic. Whether or not they will cause symptoms depends primarily on size and location.65 Because of the kyphotic nature of the thoracic spine, the spinal cord will usually rest against the posterior aspect of the vertebral body when patients are upright. A central disc herniation in the thoracic region can more easily produce cord deformation, even though the protrusion itself may not be terribly large. Cord compression can cause pain that is typically in the midline of the back. Patients may also describe a boring type pain that radiates through the chest to the sternal area. Other reasons for thoracic pain, such as thoracic or intra-abdominal visceral causes, must be kept in mind. Pain, however, may be minimal or nonexistent, yet enough cord compression can cause thoracic myelopathy. These patients present with gait imbalance, weakness of the lower extremities, and/or numbness of the lower extremities. Severe compression may cause sphincter dysfunction as well. The pattern would be that of an upper motor neuron lesion since the spinal cord is involved. Posterolateral disc protrusions in the thoracic spine may not cause cord compression at all, but if large enough can pinch the exiting nerve root and cause radicular pain radiating around the rib cage at the level of the herniation.
aware of thoracic disc pathology, however, since the introduction of MRI technology and the ability to easily image this area (Fig. 22-7). As with disc herniations anywhere in the spine, thoracic disc herniations are usually asymptomatic. Whether or not they will cause symptoms depends primarily on size and location.65 Because of the kyphotic nature of the thoracic spine, the spinal cord will usually rest against the posterior aspect of the vertebral body when patients are upright. A central disc herniation in the thoracic region can more easily produce cord deformation, even though the protrusion itself may not be terribly large. Cord compression can cause pain that is typically in the midline of the back. Patients may also describe a boring type pain that radiates through the chest to the sternal area. Other reasons for thoracic pain, such as thoracic or intra-abdominal visceral causes, must be kept in mind. Pain, however, may be minimal or nonexistent, yet enough cord compression can cause thoracic myelopathy. These patients present with gait imbalance, weakness of the lower extremities, and/or numbness of the lower extremities. Severe compression may cause sphincter dysfunction as well. The pattern would be that of an upper motor neuron lesion since the spinal cord is involved. Posterolateral disc protrusions in the thoracic spine may not cause cord compression at all, but if large enough can pinch the exiting nerve root and cause radicular pain radiating around the rib cage at the level of the herniation.
Diagnostic Evaluation
Radiographic imaging is the basis of evaluation for these patients. Plain films may show evidence of thoracic disc disease which will not be terribly helpful.66,67 However, fractures or evidence of bone destruction such as with neoplastic disorders or infection will often be readily visible on plain x-rays. The next study of choice is MRI. This allows for excellent visualization of soft tissue such as disc herniations and a good view of bone pathology as well.68,69,70 A good quality image can detect disc protrusions and cord deformation if present. At times, signal changes within the cord are visible, suggesting acute injury with edema or more commonly chronic compression causing histologic changes termed myelomylacia. The predictive value of signal changes while in the spinal cord itself and of degenerative conditions is debatable at this time.
Plain CT scans are typically not helpful for evaluation of thoracic disc pathology. CT myelography does give an excellent outline of the spinal cord and is still helpful for preoperative planning. Electromyography (EMG) nerve conduction studies are not helpful for the diagnosis of thoracic disc herniation in order to evaluate myelopathy or radiculopathy; however, it may be of use for differential diagnosis considerations such as Guillain-Barré syndrome, peripheral neuropathy, or amyotrophic lateral sclerosis. Evoked potential studies in these authors’ opinion have been of little diagnostic or prognostic value for thoracic disc pathology.
Nonoperative Treatment
Nonoperative treatment of thoracic disc herniations will follow similar guidelines for low back pain. Mild to moderate symptoms can be treated with nonsteroidal anti-inflammatories, narcotic pain medicine for short periods, and muscle relaxers. Passive modalities such as heat, ice, ultrasound, and electrical stimulation have all been used and may promote short-term relief. Thoracic strengthening exercises plus aerobic conditioning may promote pain relief in the longer term. These authors would not recommend epidural steroid injections for a central disc herniation with cord compression; however, intercostal root blocks may give some relief for a more posterolateral disc herniation with radicular symptoms radiating around the rib cage.
Operative Treatment
Indications for surgery include intolerable pain unresponsive to conservative measures and evidence of thoracic myelopathy from cord compression.71 Because the surgical treatment of thoracic disc herniations requires a fairly large operation, most surgeons will allow for many months or even years for pain symptoms to resolve on their own before recommending operative intervention.72
Because thoracic disc herniations usually produce anterior cord compression, the anterior surgical approach is typically favored.73,74 This allows for a no-touch technique such that the disc herniation is pulled away from the dura thus relieving the anterior compression on the cord without manipulation of the neural structures. Many, but not all, spine surgeons perform an arthrodesis of that motion segment after the discectomy, though there are no hard data to
suggest that fusion is necessary.75,76 Usually this anterior approach to the spine requires an open thoracotomy, which is not without morbidity including late incisional pain. Some spine surgeons have more recently pioneered thorocoscopic surgical treatment of thoracic disc herniations.77,78 This also requires an anterior approach but through much smaller incisional portals with thoracoscopic instruments. The steep learning curve and questions regarding ultimate improvement in outcomes compared to standard open techniques have kept this technique from becoming mainstream.
suggest that fusion is necessary.75,76 Usually this anterior approach to the spine requires an open thoracotomy, which is not without morbidity including late incisional pain. Some spine surgeons have more recently pioneered thorocoscopic surgical treatment of thoracic disc herniations.77,78 This also requires an anterior approach but through much smaller incisional portals with thoracoscopic instruments. The steep learning curve and questions regarding ultimate improvement in outcomes compared to standard open techniques have kept this technique from becoming mainstream.
Thoracic Spinal Stenosis
Unlike thoracic disc herniations, the pathoanatomy for thoracic stenosis arises from the posterior elements. Posterior facet hypertrophy and occasionally ossification of the ligamentum flavum produce dorsal compression.79,80,81,82,83 Circumferential canal compromise can occur if there are associated bulging discs or endplate osteophytes (Fig. 22-8). Typically this occurs over several levels and is more common in the lower thoracic spine. These degenerative changes occur slowly over time and significant compression may be present before clinical symptoms arise. Presentation usually develops as a gait disturbance, weakness in the lower extremities, or numbness. Sphincter dysfunction is a late sign usually associated with severe compression. Hyperreflexia and pathological reflexes consistent with upper motor neuron pathology will be present in moderate to severe myelopathy.
Diagnostic Imaging
MRI is the study of choice for initial evaluation of suspected thoracic spinal stenosis. Because the pathology is often bony in nature with hypertrophic osteoarthritic facet changes, CT myelography may allow better visualization of the pathoanatomy, which can be useful for preoperative planning.
Because of the difference in pathoanatomy, thoracic spinal stenosis is typically treated by a posterior approach as opposed to anterior surgery for thoracic disc herniations as described earlier.84 A laminectomy at the appropriate number of pathological levels will typically decompress the spinal cord and allow for neural recovery or at least stop the neurologic deterioration.85 Many surgeons will add a posterior instrumented fusion over the decompressed levels if there are instability, kyphotic deformity, or obesity issues.86,87,88
Lumbar Spine
Introduction
For many patients and physicians alike, problems related to the lumbar spine may be considered the bane of human existence. Low back pain and degenerative conditions of the lumbar region are ubiquitous, with symptoms ranging from a minor annoyance to incapacitating pain. Though imaging techniques have certainly given us better anatomic views of the lumbar spine and associated pathological conditions, there is often a disconnect between patient symptoms and radiographic findings.89,90,91 Add this variability to a plethora of nonoperative and operative treatment options with less than clear-cut outcomes, and one is left with a difficult area in health care. This section will attempt to provide clarity and acknowledge the limitations in both knowledge and clinical practice.
Incidence
It is estimated that 50% to 80% of the adult population will at some time suffer from low back pain.92,93 One study documented a true incidence of 34% of men and 37% of women will develop new onset of low back pain over a 1-year period of the study.94 Not only is low back pain common but it can also be functionally limiting, leading to significant time lost at work.95,96,97,98,99 Twelve and a half percent of all illness-related absent days during a 10-year period were due to back pain in a Swedish study.100 This has a huge socioeconomic impact on the economy. Using 1996 data, the total annual productivity losses from chronic back pain were estimated to be $28 billion in the United States alone.101 More recently, the total annual direct and indirect costs for chronic low back pain were $2,900 and $16,600, respectively.102 Spine disorders were the most frequent main cause of work limitation in adults in 1998, followed by heart disease, OA, and respiratory diseases.96 In 1999, six large U.S. employers were evaluated for conditions generating the largest health and productivity cost burdens; it was found that for physical diseases, low back pain ranked fourth behind angina pectoris, essential hypertension, and diabetes mellitus.103
Risk Factors
Certain factors have been shown to contribute to the development of disorders of the lumbar spine.104,105,106,107,108 One study demonstrated earlier radiographic degenerative changes in masonry workers doing heavy labor as compared to house painters.109 There is also some evidence, however, that people who are sedentary may have a greater incidence of degenerative disc disease.106,110 People who drive a bus or truck for a living have also been shown, in some studies, to have a higher incidence of low back disorders, perhaps because of vibrational stress—although other studies seem to show no correlation.111,112,113,114
Other factors such as obesity115,116 and smoking117 have been associated with a higher risk of degenerative disc disease. As in any clinical disorders, genetics is also believed to play a role.118,119,120 A study comparing monozygotic and dizygotic twins121 suggests that a strong genetic influence on intervertebral disc degeneration. A defect in collagen IX was recently reported in certain patients with lumbar disc herniations.122,123 Additional studies found that the Trp 3 allele acted synergistically with obesity to increase disc bulging and height loss in the lumbar spine.124 Elevated levels of collagen II degradation may also play a role in postmenopausal women.125,126
Pathoanatomy
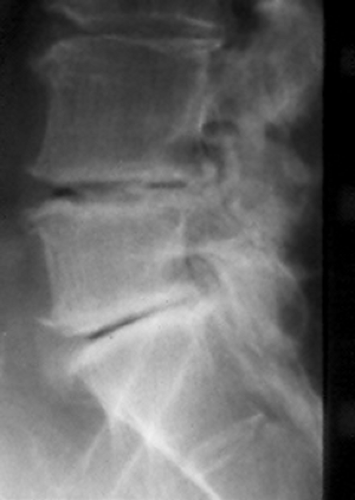
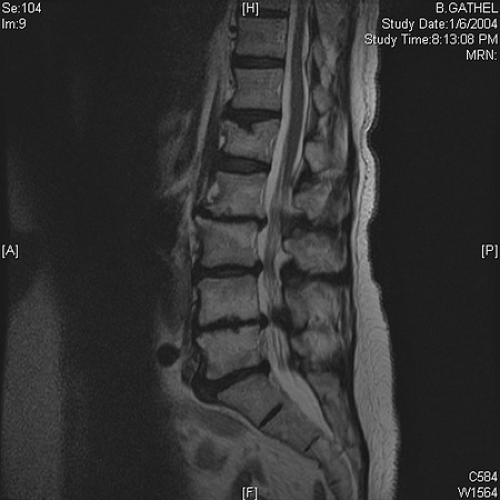
The underlying cause of degenerative conditions in the lumbar spine is due to aging of the intervertebral disc (Fig. 22-9A, B, C).127,128 Normal discs are excellent shock
absorbers and allow motion at multiple segments in the entire spine. The center of the disc is the nucleus pulposus, which consists of proteoglycans, type II collagen, and water, with small contributions from type IX and other collagens. The nucleus is concentrically surrounded by the multilayered annulus fibrosis. This is composed of strong type I collagen that is attached to the end plates of the vertebral body above and below. Biochemical changes occur within the nucleus pulposus primarily with loss of water content and a relative shift of chondrotin sulfate to keratin sulfate which makes up the proteoglycan matrix.129,130,131 Loss of hydrostatic pressure and fluid-like properties of the nucleus compromises the ability of the disc to resist compression and shear forces.132,133 Bulging of the disc occurs and the annulus develops tears or fissures.134,135,136 When the nucleus pulposus protrudes posteriorly, either elevating the annulus or penetrating through it, a disc herniation has occurred. Though many disc herniations occur in young individuals with seemingly healthy discs, most disc herniations occur in slightly degenerative discs where the annulus cannot contain the herniation of nucleus pulposus material.
absorbers and allow motion at multiple segments in the entire spine. The center of the disc is the nucleus pulposus, which consists of proteoglycans, type II collagen, and water, with small contributions from type IX and other collagens. The nucleus is concentrically surrounded by the multilayered annulus fibrosis. This is composed of strong type I collagen that is attached to the end plates of the vertebral body above and below. Biochemical changes occur within the nucleus pulposus primarily with loss of water content and a relative shift of chondrotin sulfate to keratin sulfate which makes up the proteoglycan matrix.129,130,131 Loss of hydrostatic pressure and fluid-like properties of the nucleus compromises the ability of the disc to resist compression and shear forces.132,133 Bulging of the disc occurs and the annulus develops tears or fissures.134,135,136 When the nucleus pulposus protrudes posteriorly, either elevating the annulus or penetrating through it, a disc herniation has occurred. Though many disc herniations occur in young individuals with seemingly healthy discs, most disc herniations occur in slightly degenerative discs where the annulus cannot contain the herniation of nucleus pulposus material.
 Figure 22-9A A lateral radiograph of the lumbar spine showing normal disc height, normal alignment, and lack of osteophyte changes. |
Simple bulging of the disc with loss of height will slightly alter the biomechanics of that motion segment.137,138 This will directly affect the facet joints posteriorly over the long term. These joints are true synovial joints and here is where true OA can occur, with hypertrophic bony changes and loss of cartilage.139,140,141,142,143,144,145 These degenerative changes can lead to thickening of the soft tissues with hypertrophic capsule and ligamentum flavum developing. These posterior element changes, in conjunction with bulging (or herniated) discs, can compromise the volume of the spinal canal and the neural elements leading to lumbar spinal stenosis. Facet arthritis and capsular changes can lead to incompetence of the facet joints as stabilizing structures.139 If the disc is unable to control shear forces, then a degenerative spondylolisthesis can slowly develop. This is very common in the older population at the L4-5 level, more so in females than males. Asymmetric degenerative changes in the lumbar spine structures can lead to degenerative scoliosis.
Clinical Syndromes
Mechanical Low Back Pain
Low back pain is a general term that includes many pathologic conditions and spans many patient age groups. It is well known that low back pain can occur with totally normal radiographic studies including MRI. This is believed to be due to soft tissue strain on muscle, ligament, or capsular tissues.146 Tears of the outer annulus fibrosis can at times be seen on MRI. This is felt to be a possible cause of low back pain in some individuals, but the correlation of symptoms with these radiographic findings are limited.147 There is reasonably good evidence, however, that degeneration of the intervertebral discs is responsible for mechanical back pain in many patients. One study148 documented that in a group of 20-year-old patients, one or more lumbar discs were abnormal in 57% of those with low back pain symptoms versus only 35% of asymptomatic patients. However, the incidence of radiographic disc degeneration is certainly much higher than that of symptomatic lumbar disorders.149,150 In a study of asymptomatic patients using MRI, approximately one third of subjects were found to have substantial abnormalities. In patients 60 years of age or more, abnormal findings were present on 57% of these MRI scans.151 Even patients younger than 40 years of age showed a 19.5% incidence of disc degeneration or other radiographic abnormalities.152
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree