The open operative management of pelvic and acetabular fractures in the obese is technically demanding, with a significantly higher rate of complications compared with patients who are nonobese. The decision to perform surgery should involve a thorough understanding of risks, and patients should be counseled. Careful attention should be paid to patient factors; coexisting systemic conditions and patient positioning to reduce complications. Wound complications are most commonly seen, and techniques to reduce risk should be incorporated. When complications occur, aggressive management can result in successful salvage. Future areas of study should include methods to reduce risk of surgical site infections and improving our understanding of the physiologic alterations that occur with obesity. This article summarizes the current literature on open treatment of pelvic and acetabular fractures in the obese patient, reviews the physiologic adaptations of obesity as they relate to pelvic surgery, highlights risk factors for complications, and provides recommendations to reduce the incidence of complications.
Pelvic and acetabular fractures most frequently result from high-energy motor vehicle trauma or falls. Open reduction and internal fixation of these fractures requires an extensive surgical approach that is often associated with long operative times, high blood loss, and a significant risk of postoperative complications. The prevalence of obesity in the United States currently exceeds 25% and is projected to exceed 40% by 2025. Recent reports have noted a higher rate of complications after the operative treatment of pelvic and acetabular fractures compared with patients of normal weight. This article summarizes the current literature on open treatment of pelvic and acetabular fractures in the obese patient, reviews the physiologic adaptations of obesity as they relate to pelvic surgery, highlights risk factors for complications, and provides recommendations to reduce the incidence of complications.
Once the decision has been made to proceed with operative treatment of a pelvic or acetabular fracture, the method of definitive treatment may need to be modified based on patient factors such as associated injuries, status of the soft tissue in and around the zone of injury, or medical comorbidities. Obesity has been associated with a wide spectrum of comorbidities that affect nearly every organ system, including cardiac, pulmonary, endocrine, and neurologic systems. The orthopedic surgeon needs to be aware and understand the altered physiology of an obese patient and that adjustments may need to be made preoperatively, intraoperatively, and postoperatively in the management of the obese patient with an operative pelvic or acetabular fracture.
Initial evaluation
The initial assessment and evaluation of a pelvic and acetabular fracture in the patient who is obese is more difficult than for a patient who is not obese. These injuries may result in life-threatening hemorrhage, and prompt recognition of these injuries is critical. Standard advanced trauma life support evaluation and resuscitation protocols should be followed. Fluid resuscitation and the use of blood are critical because the cardiac system of patients who are obese may already be stressed by adaptations made as it attempts to perfuse the increased tissue mass. The orthopedic examination of the pelvis and extremities can be more difficult secondary to the body habitus. A visual inspection should be made for signs of hemorrhage or open wounds. All skin folds, including the panniculi, need to be examined because they can hide wounds. Anterior pelvic injuries should increase suspicion for urethral injuries. Careful inspection of the groin, perineum, buttocks, and posterior pelvis should be performed for possible wounds or blood at the urethral meatus. A speculum examination should be performed in women with anterior pelvic injuries. The increased soft tissue can make soft tissue swelling less obvious and bony palpation more difficult. The sensory and motor examination can be more challenging in the obese patient because abnormalities related to diabetes or vascular disease are common. A thorough examination must include palpation and examination of all extremities to identify any other injuries. The morbidly obese patient has a baseline decreased range of motion of the hips, knees, and other joints, so the examiner should be alert to any asymmetries on examination.
Before the definitive treatment plan can be made, a complete radiographic assessment of the pelvis and acetabulum is required. This radiographic evaluation of the obese patient can be more challenging because the increased adipose tissue can lead to inadequate penetration of the x-rays, resulting in increased noise and low image contrast. In addition, an increase in the time required for penetration results in motion artifact, further degrading the quality of plain films. To improve image quality, reacquisition and postacquisition adjustments can be made, including the use of a Bucky grid to minimize scatter, increasing the kilovolts peak and milliamperes to improve penetration and increasing the film development speed.
Computed tomography (CT) is routinely performed in trauma patients to assess for visceral injuries. Bony cuts and reconstructions can be helpful in delineating fracture patterns and for preoperative planning. The weight or size of the obese patient needs to be considered, because it may exceed the limits for the CT scanner available in the hospital. Most institutions have CT scanners with table weight limits of approximately 200 kg and an available gantry diameter limit of 52 to 55 cm. In a recent national survey of hospitals, it was estimated that only 10% of emergency departments and 34% of trauma centers have access to these large weight capacity CT scanners. Veterinary schools and some zoos have access to larger-capacity CT scanners that could theoretically be used.
For some acetabular fractures with an associated posterior dislocation or central protrusion, the femoral head may not remain concentrically reduced under the roof of the acetabulum without skeletal traction. Typically, the amount of weight used for skeletal traction is 1/10 to 1/6 of the patient’s body weight (between 10 and 15 kg for a patient weighing 90 kg), which would result in significantly larger amounts of weight in the obese patient. Any larger amount of weight should be applied gradually and with caution because there is an increased risk of soft tissue or nerve injury with higher weights. The larger soft tissue envelope in the obese patient may not allow the standard traction pin to clear the soft tissues, decreasing the working length of the pin, and requiring the use of larger pins. A larger pin can lead to greater soft tissue damage during insertion, further increasing the risk of a pin tract infection. For the largest patients, it has been necessary to use the starting guidewire for a femoral nails to traverse the mass of the lower thigh. Larger tension bows might also be required and, if used, should be adequately padded to prevent compression on the anterior tibial skin, which can lead to skin necrosis or pressure ulcers.
Perioperative considerations
Obesity is an independent risk factor for cardiovascular disease, which increases the risk of perioperative complications. The cardiac system of an obese patient has several differences from a patient of normal weight. Morbid obesity is often associated with left ventricular enlargement, systolic and diastolic dysfunction (risk factors for acute ischemia or infarction), congestive heart failure, and sudden death. In addition, hypertension, hyperlipidemia, and diabetes mellitus are more common in the obese and are associated with the development of coronary artery disease. More specifically, the patient who is obese has an increased total blood volume because of the increased requirement from the greater body mass. The cardiac output of obese patients increases proportionally and can be 40% greater than that of patients with normal body weight. Pelvic and acetabular fractures are frequently associated with significant blood loss. This blood loss, combined with preexisting increased work demand, can overload the heart and increase the mortality risk. For this reason, obese patients must be adequately resuscitated before undergoing operative repair and may require the use of invasive hemodynamic monitoring to maintain cardiac index.
In addition to the physiologic adaptations to the cardiac system, the obese patient also experiences alterations to the pulmonary system. Patients who are obese have decreased chest wall compliance because of increased adipose tissue in the abdomen and chest wall. The lung compliance may be only 35% of a patient who is not obese. Also, patients who are obese have inefficient respiratory muscles, with an increased work of breathing. The increased metabolic activity of the excess fat and soft tissue results in greater oxygen consumption and carbon dioxide production. Compared with individuals of normal weight, patients who are obese have greater intra-abdominal pressures, caused by the increased weight, which decreases functional residual capacity, expiratory reserve volume, and total lung capacity. The patient who is obese requires more diaphragmatic excursion to have the same ventilation as a patient of normal weight. The changes that are present in an obese patient at baseline are exacerbated when the patient is given anesthesia and positioned for surgery. Obese patients are at increased risk for pulmonary aspiration and pneumonitis because they have higher gastric residual volumes with lower gastric pH. Combining these factors with poor ventilation places the obese patient at higher risk for atelectasis and pneumonia.
Type II diabetes mellitus is strongly associated with obesity, and similarly is an independent risk factor for postoperative complications. Some of the deleterious effects of obesity have been believed to be attributable, at least in part, to derangements in metabolic function. Insulin resistance is a major factor and plays a large role in obesity-related metabolic derangements. The lack of insulin results in hyperglycemia, decreased protein synthesis, increased protein degradation, increased susceptibility to infection, and reduced antiapoptotic (prosurvival) and antiinflammatory actions of insulin. The stress response from the trauma and pain during the perioperative period can lead to release of catecholamines that can increase blood glucose levels in patients with or without history of diabetes. This hyperglycemia can negatively effect wound healing by inhibiting the inflammatory response, impairing immunity, and interfering with collagen synthesis. Diabetes mellitus, alone, leads to impaired immune responses with impaired chemotaxis, phagocytosis, and bactericidal ability of the neutrophils, monocytes, and macrophages. Strict perioperative glycemic control has been shown to reduce morbidity and mortality, and to reduce postoperative infections.
Perioperative considerations
Obesity is an independent risk factor for cardiovascular disease, which increases the risk of perioperative complications. The cardiac system of an obese patient has several differences from a patient of normal weight. Morbid obesity is often associated with left ventricular enlargement, systolic and diastolic dysfunction (risk factors for acute ischemia or infarction), congestive heart failure, and sudden death. In addition, hypertension, hyperlipidemia, and diabetes mellitus are more common in the obese and are associated with the development of coronary artery disease. More specifically, the patient who is obese has an increased total blood volume because of the increased requirement from the greater body mass. The cardiac output of obese patients increases proportionally and can be 40% greater than that of patients with normal body weight. Pelvic and acetabular fractures are frequently associated with significant blood loss. This blood loss, combined with preexisting increased work demand, can overload the heart and increase the mortality risk. For this reason, obese patients must be adequately resuscitated before undergoing operative repair and may require the use of invasive hemodynamic monitoring to maintain cardiac index.
In addition to the physiologic adaptations to the cardiac system, the obese patient also experiences alterations to the pulmonary system. Patients who are obese have decreased chest wall compliance because of increased adipose tissue in the abdomen and chest wall. The lung compliance may be only 35% of a patient who is not obese. Also, patients who are obese have inefficient respiratory muscles, with an increased work of breathing. The increased metabolic activity of the excess fat and soft tissue results in greater oxygen consumption and carbon dioxide production. Compared with individuals of normal weight, patients who are obese have greater intra-abdominal pressures, caused by the increased weight, which decreases functional residual capacity, expiratory reserve volume, and total lung capacity. The patient who is obese requires more diaphragmatic excursion to have the same ventilation as a patient of normal weight. The changes that are present in an obese patient at baseline are exacerbated when the patient is given anesthesia and positioned for surgery. Obese patients are at increased risk for pulmonary aspiration and pneumonitis because they have higher gastric residual volumes with lower gastric pH. Combining these factors with poor ventilation places the obese patient at higher risk for atelectasis and pneumonia.
Type II diabetes mellitus is strongly associated with obesity, and similarly is an independent risk factor for postoperative complications. Some of the deleterious effects of obesity have been believed to be attributable, at least in part, to derangements in metabolic function. Insulin resistance is a major factor and plays a large role in obesity-related metabolic derangements. The lack of insulin results in hyperglycemia, decreased protein synthesis, increased protein degradation, increased susceptibility to infection, and reduced antiapoptotic (prosurvival) and antiinflammatory actions of insulin. The stress response from the trauma and pain during the perioperative period can lead to release of catecholamines that can increase blood glucose levels in patients with or without history of diabetes. This hyperglycemia can negatively effect wound healing by inhibiting the inflammatory response, impairing immunity, and interfering with collagen synthesis. Diabetes mellitus, alone, leads to impaired immune responses with impaired chemotaxis, phagocytosis, and bactericidal ability of the neutrophils, monocytes, and macrophages. Strict perioperative glycemic control has been shown to reduce morbidity and mortality, and to reduce postoperative infections.
Intraoperative considerations
Patient Positioning
The weight of the patient needs to be considered when determining whether the operating room table will be secure and safe for the patient. Most standard operating room tables have a safe weight limit of 200 to 225 kg, but some manufacturers offer newer operating tables that can accommodate up to 450 kg. If the high-capacity table is not available, 2 tables can be secured head to head or side by side. However, this 2-table arrangement can make intraoperative fluoroscopic imaging more difficult. Lifts can be placed under the table for additional support. Surgical patients who are obese are prone to falling off during positioning, and bean bags and straps should be placed to secure the patient to the table and prevent falls during table position changes.
Because obese patients who have a pelvic or acetabular fracture may present with borderline physiology (as discussed previously), careful consideration of surgical positioning must be made because intraoperative positioning can affect the patient’s ability to tolerate the procedure. Although patient positioning is most commonly determined by fracture pattern and surgical approach, the surgeon should recognize that positions that restrict chest and abdominal motion can compromise ventilation and are poorly tolerated by obese patients. The supine and prone positions can result in compression of the vena cava and the aorta as well as compression of the diaphragm, making ventilation more difficult. The lateral decubitus is best tolerated by obese patients, because the weight of the panniculus adiposus is off the abdomen, allowing for greater diaphragmatic excursion. The lateral position may also allow for posterior soft tissues to fall away, improving access to the acetabulum.
Authors’ preferred practice: patient positioning
Supine Position
Patients are positioned on a radiolucent table on a lumbosacral support placed in the midline of the back from the inferior angle of the scapula distally to the proximal aspect of the anal crease. This position allows for the soft tissues to be elevated off the bed and also allows for the panniculi to fall posteriorly instead of pushing laterally where the exposure is to be made. Rolled sheets or blankets are used to allow for intraoperative fluoroscopic imaging. The chest is stabilized with a padded belt. Another precaution is to securely stabilize the nonoperative extremities, particularly the lower extremities. Because the obese patient is wide compared with the radiolucent table, it is easy for the nonoperative lower extremity to roll off the table. The authors have used Ace wraps over foam padding to secure the lower extremities.
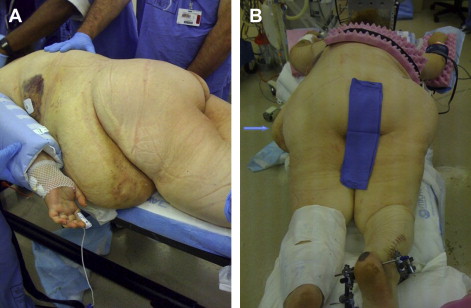
Positioning the abdominal panniculus may prove challenging. If the panniculus is especially large it may have to be secured to provide access to the operative field. The most common method is to tape the panniculus to the opposite side of the table from the operative field ( Fig. 1 ). An adhesive is applied to the skin to allow the tape to stick well to the panniculus. The panniculus is then pulled under tension to allow visualization of the proposed operative site. Another method is to sew the panniculus with large sutures to the chest wall. This method obviates concern about losing adhesion of tape. When using these techniques, the authors recommend that the patient’s ventilatory status should be observed before initiating surgery, because the extra weight of the abdomen on the chest may obstruct ventilation of the patient, necessitating release of the pannicular strapping.
If pannicular strapping is not possible, one may take advantage of the mobile nature of the panniculus. The panniculus may be gently placed or rocked away from the operative field. The weight of the abdomen will often keep much of the panniculus away from the operative field. Although not as effective as pannicular strapping, this method allows for improved visualization. Rotating the surgical table away from the surgeon is an option, but patients who are obese are much more prone to roll off the table than patients who are lean.
Prone Position
Prone positioning is used frequently for stabilization of acetabular fractures and pelvic ring injuries. To avoid difficulties with ventilation in the prone position, it is imperative that the abdomen be allowed to hang free, preventing excessive intra-abdominal pressure that may contribute to ventilatory compromise. Longitudinal chest rolls are typically positioned on each side of the patient from the chest distally to the anterior superior iliac spine. The chest rolls must not be placed distal into the femoral canal because the patient’s weight against the roll may result in a femoral nerve palsy. If the patient has a particularly wide panniculus or protuberant abdomen, then transverse rolls are used. One roll is placed transversely across the chest and another transversely across the anterior superior iliac spines. Sheets or blankets are added to the rolls to ensure that the abdomen hangs free and the patient can be adequately ventilated ( Fig. 2 ). If the abdomen is markedly obese, then, in addition to transverse chest rolls, the abdomen may need to be folded under to the nonoperative side to allow the surgeon closer access to the operative site ( Fig. 3 ).
The knees are especially susceptible to pressure in the prone position and must be protected against pressure necrosis. Donut pads are used beneath the knees to protect the skin over the patellae. The legs are placed on a pillow to prevent the toes from contacting the surgical bed. The nonoperative limb is stabilized with an Ace wrap.
Lateral Position
Positioning devices or beanbags may be used to secure a patient in the lateral position. The authors prefer beanbags to positioning devises for better control of the abdomen. An extra-large beanbag is often required, but on the most obese patients, 2 beanbags taped together may be required ( Fig. 4 ). A positioning pillow originally designed for treatment of calcaneal fractures can be used to provide a flat, stable surface to support the operative limb distal to the operative site (Excel Medical Solutions, Plymouth MN) ( Fig. 5 ).


Once the patient is positioned, special care attention needs to be made to protecting pressure areas, because the risk of pressure sores and neural injuries is higher in the obese patient. The increased weight leads to increased pressure on contact points and makes it more difficult to properly position the unconscious obese patient safely. The table extensions and arm boards need to provide enough padding with sufficient size and strength to maintain proper positioning. Stretch injuries to the brachial plexus can occur during supine or prone positioning either from the arms being excessively abducted or from the weight of the patient’s outstretched arm. In the supine position, the arms need to be placed on adequately padded arm boards to prevent the dorsal extension of the arm, which can stretch the plexus or put pressure on the ulnar nerve at the elbow. Perioperative ulnar neuropathy has been associated with increased body mass index (BMI, calculated as weight in kilograms divided by the square of height in meters). Sciatic nerve palsies can occur from prolonged ischemic pressure associated with tilting the bed. When placing the patient into the lateral decubitus position, care needs to be taken to protect the peroneal nerve on the nonoperative lower extremity.
The additional weight of the obese patient also makes them prone to pressure ulcers. Pressure ulcers occur when the blood supply to the tissue is diminished, leading to ischemia, which can result in necrosis. The main causes of pressure ulcers are pressure, shearing, and friction. Any external pressure greater than 32 mm Hg can cause capillary occlusion, limiting oxygen distally. The use of blankets and sheets can increase pressures by almost 44 mm Hg. The increased mass from the obese patient creates more pressure because of their larger bodyweight loading on bony prominences, which in turn induces higher mechanical stress concentrations (ie, high forces per unit area of tissue) in their deep soft tissues ( Fig. 6 ). There are reports of compartment syndromes attributed to poor positioning of the obese patient. Surgical times as low as 2.5 to 4 hours have been shown to significantly increase the risk of postoperative pressure ulcer development. Intraoperatively, patient warmers have been associated with the development of fewer pressure ulcers. Avoiding hypotension and maintaining tissue perfusion and oxygenation further reduces the risk of pressure ulcer formation.

Antibiotic Prophylaxis
The bioavailability of prophylactic antibiotics and anesthetic medications is affected by the increased amount of adipose tissue present in the obese patient. The physiologic changes related to obesity can change the volume of distribution, the amount of protein binding, the metabolism, and the elimination of drugs. The volume of distribution of lipophilic drugs is altered by the increased adipose tissue, and hydrophilic medications can be affected by the increased organ mass, decreased lean body mass, and increased blood volume and cardiac content. These changes that occur with obesity can potentially lead to under- or overtherapeutic concentrations of medications. One study found in patients with a BMI greater than 50 kg/m 2 that 2 g of cefazolin only achieved therapeutic levels in 30% of tissues. Aminoglycosides have been shown to require a dosing adjustment in obesity because of these altered pharmacokinetics; however, it has also been shown that simply dosing based on weight can lead to increase risk of toxicity. To avoid overdosing in obesity, the change in the volume of distribution can be accounted for by a dosing weight correction factor. Similarly, obese patients have been shown to have increased volumes of distribution and clearance of vancomycin through the kidneys, thus requiring level monitoring and weight-based dosing. The available information for cephalosporins and other classes of antimicrobials suggests that dosages may need to be increased in obese compared with nonobese patients to attain similar effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




