Open Repair of Anterior Shoulder Dislocations and Subluxations
Bertram Zarins
INDICATIONS/CONTRAINDICATIONS
Although Perthes (1) first proposed reattachment of an avulsed anterior shoulder capsule, this lesion has most commonly been named after Bankart (Bankart lesion) (2, 3). The Bankart procedure consists of reattachment of an avulsed anterior glenohumeral capsule, with or without its glenoid labrum, directly to the bone of the anterior glenoid rim. A modified Bankart repair is an anterior shoulder capsulorrhaphy in which a stretched capsule is overlapped and secured to a stable glenoid labrum (4). Perhaps more than anyone else, Rowe (4, 5, 6, 7) refined and popularized this technique and has shown that the results have stood the test of time.
The Bankart procedure is indicated for symptomatic recurrent anterior shoulder dislocations and subluxations that persist despite nonoperative measures. The operation is most clearly indicated for the shoulder in which the etiology of the instability is traumatic. Posttraumatic shoulder instability is commonly associated with an avulsion of the anterior glenoid labrum from the glenoid rim by the inferior glenohumeral ligament (8). The patient for whom this operation is ideal is the one who has unidirectional anterior shoulder instability.
A second indication for this procedure is in a patient who has had failed prior instability surgery, in which that prior surgery did not specifically address the presence of a Bankart lesion. Whatever the prior surgical procedure, if a persistent Bankart lesion exists, the patient may benefit tremendously by a direct repair of that lesion.
A third indication is a large fracture of the anterior-inferior glenoid rim (a large “bony Bankart lesion”) that is amenable to open reduction and internal (screw) fixation.
This surgical repair is not indicated in patients who have voluntary shoulder instability and who have emotional or psychological problems that contribute to their shoulder condition. These patients, of course, are not surgical candidates for any type of repair. A relative contraindication for this operation is the presence of multidirectional shoulder instability. The Bankart procedure effectively tightens the anterior capsule to the glenoid rim. In the patient who has multidirectional instability, failure to address the other directions of laxity can lead to persistent instability and, in fact, a fixed subluxation in the direction opposite the anterior repair. In the patient who has multidirectional instability, a Bankart repair may be combined with other capsular procedures to correct all directions of laxity.
Another relative contraindication to performing this procedure alone is the presence of significant glenohumeral arthritis. In a patient who has advanced glenohumeral arthritis, repair of the Bankart lesion would not be expected to provide significant benefit; however, the presence of severe degenerative changes in the glenohumeral joint is not commonly associated with symptomatic anterior shoulder instability.
PREOPERATIVE PLANNING
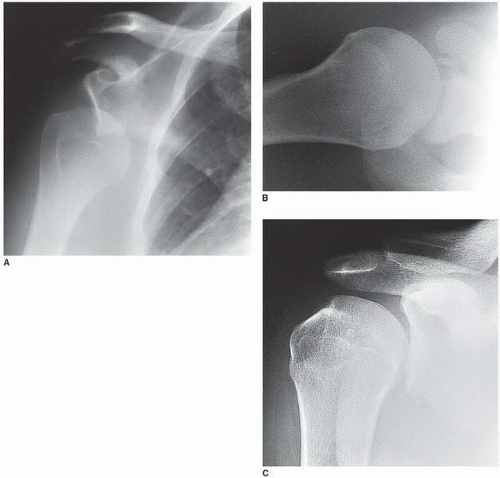
A Bankart lesion can be prepared as an open procedure or as an arthroscopically assisted operation (9, 10, 11, 12, 13). The principle is the same: to reattach the avulsed capsule to the anterior glenoid rim. This chapter describes the open approach. The most important component of preoperative planning is to correctly diagnose the direction of instability. It is easy to arrive at the correct diagnosis if radiographs document the shoulder in a dislocated state (Fig. 19-1A). Correctly diagnosing shoulder subluxation can be more difficult. A typical symptom of anterior subluxation is pain during forceful throwing or other overhead activities (4). Rowe (4) coined the term “dead arm syndrome” for recurrent transient subluxation of the shoulder. Positive physical findings in patients who have anterior subluxation are a positive apprehension sign when the shoulder is externally rotated in a position of 90 degrees of abduction and anterior translocation of the humeral head in this position of the arm. A momentary subluxation or click sometimes can be elicited.
A patient who has unidirectional instability may have a positive relocation test in which the pain or sense of apprehension is eliminated as posterior pressure on the humeral head centers the humeral head into the glenoid fossa. Although it is unusual to be able to elicit specific subluxation or dislocation of the shoulder on examination because of intense muscle guarding in the threatened position, subluxability may be present and painful when the arm is at the side if direct pressure is applied on the posterior humeral head increasing the translation in an anterior direction. Range of motion of the shoulder is typically not limited other than by apprehension. Strength of the rotator cuff and
deltoid is usually normal. The most helpful radiographs are an anteroposterior view in internal rotation, a Stryker notch view, and a West Point axillary view (Fig. 19-1B). The first two radiographs are most helpful in identifying the presence of an associated Hill-Sachs lesion (Fig. 19-1C), and the last view can show bone reaction, rounding off, erosion, or separation of the anterior glenoid rim. In addition, mild arthritic changes may be present on the humeral head.
deltoid is usually normal. The most helpful radiographs are an anteroposterior view in internal rotation, a Stryker notch view, and a West Point axillary view (Fig. 19-1B). The first two radiographs are most helpful in identifying the presence of an associated Hill-Sachs lesion (Fig. 19-1C), and the last view can show bone reaction, rounding off, erosion, or separation of the anterior glenoid rim. In addition, mild arthritic changes may be present on the humeral head.
Additional imaging studies have proven helpful in identifying the presence of a Bankart lesion. These include computed tomography arthrography, magnetic resonance imaging (MRI), and MRI arthrography. While plain MRI is of limited value, the addition of contrast material more clearly defines the pathology in the glenoid labrum area. In addition, all of these studies can show the presence of even small Hill-Sachs lesions.
However, if the presence or absence of a Bankart lesion is to be determined with a high degree of accuracy, diagnostic arthroscopy gives the best direct view of intra-articular pathology. The advantage of this is that it can be combined with a careful examination under anesthesia to ensure that the instability is truly unidirectional.
SURGERY
Patient Positioning
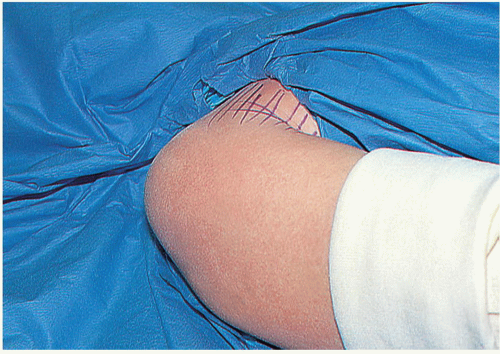
General anesthesia is induced and both shoulders are examined to determine excessive laxity. An intravenous dose of antibiotic is administered. The supine patient is positioned flat on the table (Fig. 19-2). Nothing is placed under the scapula. An arm board is placed close to the side of the operating room table so that the patient’s elbow is level with one end of the arm board. This allows the surgeon to stand close to the patient’s body and to place a large bolster under the patient’s elbow. The shoulder, hemithorax, and upper extremity up to the wrist are prepared and draped in a sterile manner (Fig. 19-3). Before a SteriDrape (3M Worldwide, St. Paul, MN) is applied over the skin, the arm is adducted across the body to define the natural axillary skin folds; these folds are marked using a skin marker (Fig. 19-4). Lines are drawn perpendicular to the skin marks (to act as guides for reapproximating the skin edges) and the Steri-Drape is applied to seal the skin. The surgeon stands at the patient’s side just distal to the flexed elbow that is supported by the large bolster.
Technique
Make a vertical skin incision in the anterior axillary fold along the line previously marked (Fig. 19-5). The proximal end of the incision is located near the coracoid process. The incision can be placed in the axilla if cosmesis is a concern. Infiltrate the subcutaneous tissues with a solution containing bupivacaine 0.25% and epinephrine 1:200,000. Dissect the superficial fascial layer to create skin flaps. Do not carry the dissections as deep as the deep fascial layer or the muscle. If the muscle is visible, the dissection is deep to the deep fascial layer and it will be difficult to find the deltopectoral interval. The deltopectoral interval is marked by a fine line of fat within the muscular layer just deep to the deep fascia (Fig. 19-6). The upper end of this line is close to the coracoid process, which should be palpated. Dissect in this fatty layer into the deltopectoral interval, retracting the cephalic vein and deltoid muscle laterally and the pectoralis major muscle medially (Fig. 19-7). Palpate the coracoid process and do not extend the dissection further proximally (unless the rotator cuff needs to be explored) or medially (to avoid injuring the musculocutaneous nerve). Retract the deltoid muscle laterally and the pectoralis major muscle medially using a self-retaining Kolbel retractor (Link Orthopaedics, Pinebrook, NJ) (Fig. 19-8). A single-spike retractor (Bankart Shoulder Repair Kit, Kirwan Surgical Products, Inc., Marshfield, MA) can be placed on the superior aspect of the humeral head below the coracoacromial ligament to improve visualization proximally. Incise the clavipectoral fascia, and identify the medial edge of the conjoined tendon. Do not mistake the edge of the tendon itself as the proper location to dissect: Several millimeters of coracobrachialis muscle are located lateral to the tendinous part of the conjoined tendon, and the lateral edge of the muscle is the proper site of dissection (Fig. 19-9). Move the Kolbel retractor deeper to retract the conjoined tendon medially. The subscapularis tendon is now exposed.
 FIGURE 19-3 The right shoulder is prepped and draped. A sterile towel covers the forearm and hand and is wrapped with a sterile gauze. |
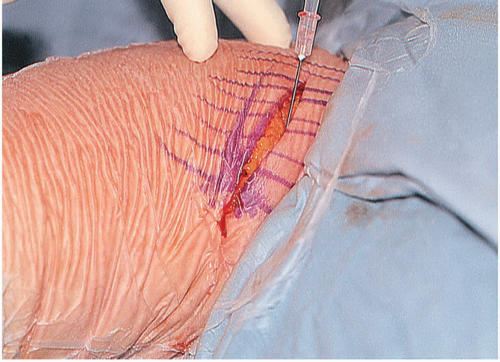 FIGURE 19-5 A sterile drape has been applied to the skin. A vertical skin incision is made along a line previously marked. Bupivacaine with epinephrine is being injected along the edges of the incision.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|