Open Reduction and Internal Fixation of the Mature Ankle
Sanjit R. Konda
Kenneth A. Egol
DEFINITION
The ankle is a modified hinge joint, which relies on a congruently reduced mortise to provide optimal function.
Maintenance of normal tibiotalar contact is essential if one is to maintain function.
Surgical treatment of displaced, unstable ankle fractures centers on anatomic restoration of the bony and ligamentous relationships that make up the ankle mortise.12
This chapter will focus on the treatment of a specific pattern of injury to the ankle, specifically, the bimalleolar fracture pattern.
ANATOMY
The anatomy of the distal tibia and ankle joint must be taken into account when considering ankle fractures. As the tibial shaft flares in the supramalleolar region, the dense cortical bone changes to metaphyseal cancellous bone (FIG 1A).
The shape of the tibial articular surface is concave, with distal extension of the anterior and posterior lips.
This surface has been called the tibial plafond, which is French for ceiling.
The talar dome is wedge-shaped and sits within the mortise. It is wider anteriorly than posteriorly.
The medial end of the tibia is the medial malleolus.
The medial malleolus is composed of the anterior and posterior colliculi, separated by the intercollicular groove (FIG 1B).
The anterior colliculus is the narrower and most distal portion of the medial malleolus and serves as the origin of the superficial deltoid ligaments.
The intercollicular groove and the posterior colliculus, which is broader than the anterior colliculus, provide the origin of the deep deltoid ligaments.
The insertions of the deltoid ligaments (medial tubercle of the talus, navicular tuberosity, and sustentaculum tali) can also be considered as part of the medial malleolar osteoligamentous complex.
The lateral malleolus is the distal end of the fibula. It extends about 1 cm distally and posteriorly compared to the medial malleolus.
The syndesmotic ligament complex unites the distal fibula with the distal tibia. The following ligaments make up the syndesmotic complex: the anteroinferior tibiofibular ligament, the posteroinferior tibiofibular ligament, the inferior transverse ligament, and the interosseous ligament (FIG 1C).
PATHOGENESIS
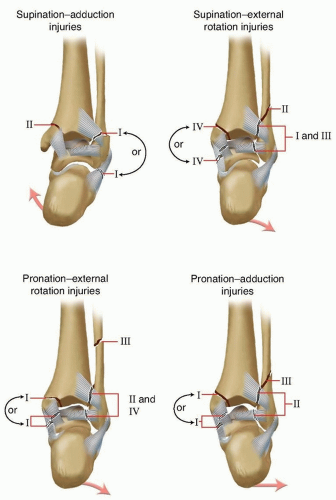
The majority of bimalleolar ankle fractures are secondary to rotation of the body about a supinated or pronated foot.8 They are best defined by the classification of Lauge-Hansen6 (FIG 2).
The supination-external rotation pattern of ankle fracture is divided into four stages.
The stage I injury is tearing of the anteroinferior tibiofibular ligaments.
As the external rotation force continues laterally, a spiral fracture of the fibula occurs. On lateral radiograph, the fracture line will pass from the anteroinferior cortex to the posterosuperior cortex.
The third stage occurs when the posteroinferior tibiofibular ligaments avulse or fracture off the posterior malleolus.
The final stage results in a medial malleolar osteoligamentous complex injury with either a deep deltoid ligament tear or a fracture of the medial malleolus.
The pronation-external rotation variant also has four stages. Because of the pronated position of the foot at injury, however, the medial structures are injured in the early stages.
The fibula fracture pattern seen with this mechanism is usually suprasyndesmotic, and the fracture pattern is an anterosuperior to posteroinferior fracture line as seen on the lateral radiograph.
The supination-adduction pattern is heralded by a low transverse fibular fracture and a vertical shearing pattern medially. This pattern is also associated with tibial plafond impaction.
Finally, the pronation-abduction pattern is identified by the avulsion of the medial malleolus and a transverse or laterally comminuted fibular fracture above the syndesmosis secondary to a direct bending moment.
PATIENT HISTORY AND PHYSICAL FINDINGS
Most patients who present with ankle pain following trauma will describe a twisting type of injury. Less frequently, they will report a direct blow to the ankle.
Proper medical history should include the patient’s current comorbid medical conditions, such as peripheral vascular disease, diabetes, or peripheral neuropathy.
Physical examination should center on inspection, palpation, and neurovascular examination.
It is important to note any gross deformity, which may signify dislocation. If dislocation is present, the ankle should be reduced and splinted as soon as possible to prevent skin tenting (and subsequent skin necrosis) and neurovascular compromise.
Inspection for any open wound about the ankle is critical as well. Open fractures imply a surgical urgency. Swelling, ecchymosis, and tenderness about the malleoli should be recorded.
For patients with a supination-external rotation pattern isolated fibula fracture who present with an intact mortise, the gravity stress examination can be revealing. More than
5 mm of medial clear space widening in association with a lateral malleolus fracture signifies an unstable pattern.7, 9
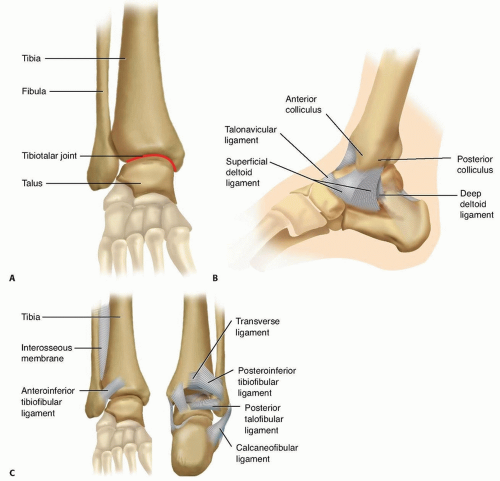
FIG 1 • A. Bony anatomy in the supramalleolar region of the distal tibia. B. Anatomy of the medial aspect of the ankle joint. C. Ligamentous anatomy about the ankle joint.
Pain at the ankle along the syndesmosis during a squeeze test implies injury to the syndesmosis.
The proximal fibula, knee, and tibia should also be examined. Palpation of pulses, detection of capillary refill, and a careful neurosensory examination must be documented prior to manipulation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographic examination includes the ankle trauma series: anteroposterior (AP), lateral, and mortise view (FIG 3A-C).
In patients with isolated lateral malleolar fractures with clinical signs of medial injury, or if there is any question of ankle stability in a supination-external rotation fracture pattern, a manual external rotation stress radiograph should be obtained to assess for instability.2, 7
The tibia is held internally rotated 15 degrees with the ankle in dorsiflexion to produce a gentle external rotation moment at the ankle under fluoroscopy (FIG 3D).11
If clinically warranted, full-length tibia-fibula radiographs should be obtained.
Restoration of medial ankle stability depends on the size and location of the medial malleolar fragment.
The size of the medial fragment is key to stability.
Anterior collicular fractures only have the superficial deltoid attached. In about 25% of supination-external rotation type 4 injuries, there will be an associated deep deltoid rupture.10 Thus, fixation of this fragment will not enhance stability.
The lateral radiograph is the key. If the fragment is greater than 2.8 cm wide (supracollicular fracture), the deep deltoid will be attached and stability is restored after fixation. If the fragment is less than 1.7 cm wide (anterior collicular or intercollicular fracture), then stability is not restored with fixation. For fractures in between, an intraoperative external rotation stress examination should be performed following malleolar fixation.16
Computed tomography (CT) scanning may be helpful in assessing posterior malleolar fragment size in rotational ankle fractures.
Magnetic resonance imaging (MRI) may have some use if there is an isolated lateral malleolus fracture with signs of medial injury and an equivocal stress examination.
DIFFERENTIAL DIAGNOSIS
Ankle sprain
Lateral malleolus fracture
Medial malleolus fracture
Maisonneuve fracture
Bimalleolar ankle fracture
Trimalleolar ankle fracture
Lateral process talus fracture
Anterior process calcaneus fracture
Subtalar dislocation
NONOPERATIVE MANAGEMENT
Ankle fractures in which the ankle mortise remains stable can be treated nonoperatively.
Isolated lateral malleolus fractures without evidence of medial-sided injury are considered supination external rotation type 2 injuries and can be treated with functional bracing and weight bearing as tolerated.
Unstable patterns, such as supination-external rotation type 4, either ligamentous or a true bimalleolar or trimalleolar ankle fracture, can also be treated nonoperatively in patients who are poor surgical candidates (eg, insulin-dependent diabetics), who have severe soft tissue problems, or who do not wish to undergo surgical stabilization.
If nonoperative treatment is chosen, it is crucial to ensure anatomic mortise reduction throughout treatment until healing.
Unstable injuries should be treated in a well-molded short-leg cast and checked on a weekly basis to ensure continued mortise reduction.
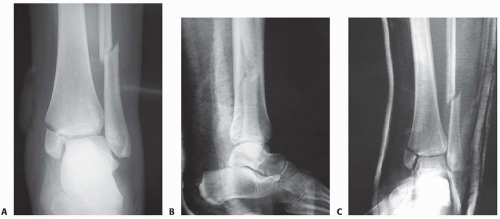 FIG 3 • Radiographic evaluation with an ankle trauma series: AP (A), lateral (B), and mortise (C) views. (continued) |
SURGICAL MANAGEMENT
Any fracture of the ankle in which there is residual talar tilt or talar subluxation such that the ankle mortise is not anatomically reduced is an indication for surgical stabilization.
Preoperative Planning
Surgical anatomy should be reviewed prior to entering the operating room, including the bony and ligamentous structures.
The neurovascular anatomy about the ankle should be reviewed, including the course of the saphenous vein medially and the superficial peroneal nerve laterally.
Equipment to be used includes a small fragment plate and screw set, large pelvic reduction clamps, small-diameter Kirschner wires, and 3.5- to 4.0-mm cannulated screw sets. If the nature of the fracture is still in question, radiographic stress examination may be performed under anesthesia.
Positioning
The patient is positioned supine with a small bump under the ipsilateral hip to ease access to the fibula.
A pneumatic tourniquet can be applied to the affected thigh if desired for use during the surgical procedure. The affected limb is prepared and draped free (FIG 4).
The bump may be removed after lateral fixation for easier access to the medial side.
If a posterior approach is chosen, the patient may be placed in the prone position to allow access to the posterior tibia via the posterolateral approach.
Approach
The fibula is approached via a direct lateral incision.
The medial malleolus is approached via a gently curved anteromedial incision.
Direct access to the posterior malleolus can be obtained through a posterolateral approach to the fibula.