Open Reduction and Internal Fixation of the Distal Femur
Animesh Agarwal
DEFINITION
Distal femur fractures are difficult, complex injuries that can result in devastating outcomes.
The distal part of the femur is considered the most distal 9 to 15 cm of the femur and can involve the articular surface. The intra-articular injury can vary from a simple split to extensive comminution.
Articular involvement can lead to posttraumatic arthritis.
These fractures constitute 4% to 7% of all femur fractures.
If the hip is excluded, they represent nearly one-third of all femur fractures.
There is a bimodal distribution defined by the mechanism of injury (see the following discussion).
ANATOMY
The supracondylar area of the femur is the zone between the femoral condyles and the metaphyseal-diaphyseal junction.
The metaphyseal bone has some important structural characteristics.
The predominant bone is cancellous.
The cortices are especially thin.
There is a wide intramedullary canal.
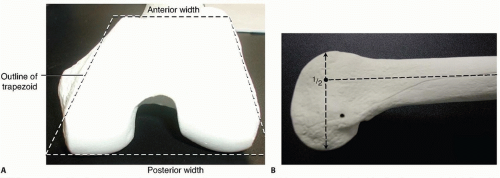
It is also important to understand the unique bony architecture of the distal femur (FIG 1).
It is trapezoidal in shape, and hence the posterior aspect is wider than the anterior aspect. There is a gradual decrease by 25% in the width from posterior to anterior.
The medial femoral condyle has a larger anterior to posterior dimension than the lateral side and extends farther distally.
The shaft is in line with the anterior half of the distal femoral condyles.
The normal mechanical and anatomic axes of the lower limb must be understood so that the alignment of the limb can be reestablished (FIG 2).
The mechanical femoral axis, which is from the center of the femoral head to the center of the knee, is 3 degrees off the vertical. The mechanical axis of the entire limb continues to the center of the ankle.
The anatomic femoral axis differs from the mechanical femoral axis in that there is 9 degrees of valgus at the knee. This results in an anatomic femoral axis of the lateral distal femur of 81 degrees or an anatomic femoral axis of the medial distal femur of 99 degrees.
The mechanical and anatomic axes of the tibia are for practical purposes identical, going from the center of the knee to the center of the ankle.
The treatment of distal femur fractures can be complicated by the various muscle attachments, which can impede or hamper proper fracture reduction.
The quadriceps and hamstrings result in fracture shortening; thus, excellent muscle paralysis must be obtained for proper reduction.
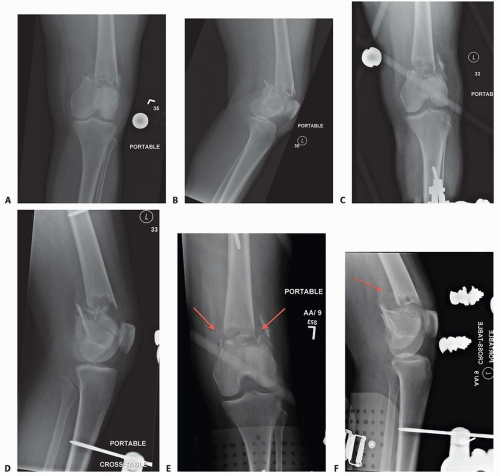
The medial and lateral gastrocnemius results in posterior angulation and displacement of the distal segment. The distal femur “extends,” resulting in an apex posterior deformity. If an intercondylar extension is present, rotational deformities of the individual condyles can occur (FIG 3A,B).
The adductors, specifically the adductor magnus, which inserts onto the adductor tubercle of the medial femoral condyle, can lead to a varus deformity of the distal segment (FIG 3C).
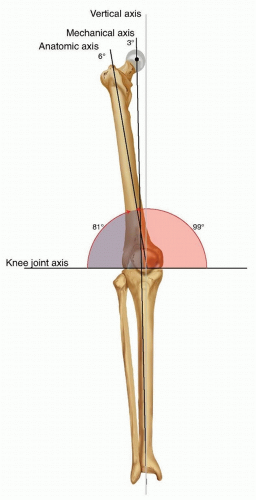
FIG 2 • Mechanical and anatomic axes of the lower extremity; the 9 degrees of valgus at the knee is noted.
The neurovascular structures about the knee are at risk when an injury of the distal femur occurs.
PATHOGENESIS
As mentioned, there is a bimodal distribution in terms of age in the epidemiology of distal femur fractures. This relates to the mechanism of injury.
High-energy and low-energy injuries occur.
High-energy injuries usually are from motor vehicle accidents and occur in the young patient. There is a direct impact onto the flexed knee, such as from the dashboard. These patients often have associated injuries such as a hip fracture or dislocation or vascular or nerve injury. These high-energy injuries generally result in comminuted fractures, mostly of the metaphyseal region. The comminution can be articular as well.
Low-energy injuries usually occur in the elderly patient who falls from a standing height. The axial loading is accompanied by either varus or valgus with or without rotation. The osteoporotic bone in these individuals leads to fracture. The fracture pattern can vary from the most simple extra-articular type to the most complex intra-articular injury. Owing to the gastrocnemius complex, an apex posterior deformity of the condyles occurs as the fragments are flexed because of the muscle attachment.
NATURAL HISTORY
Fractures of the distal femur that have intra-articular displacement can lead to severe posttraumatic arthritis if left untreated.
Operative treatment has led to a 32% decrease in poor outcomes.19
PATIENT HISTORY AND PHYSICAL FINDINGS
Direct physical examination of the knee with a distal femur fracture is limited primarily because of pain and the obvious nature of the injury.
The patient presents with a swollen and tender knee after either a fall or some high-energy trauma (motor vehicle or motorcycle accident).
A large hemarthrosis is present.
Any attempts at range of motion result in severe pain, and significant crepitus is usually noted with palpation.
If there is concern for an open knee joint, the joint can be injected after a sterile preparation to see whether the knee joint communicates with any wound.
The physical examination is directed primarily at ascertaining the neurovascular status of the lower limb and determining whether any associated injuries exist, especially the hip.
If there are any small wounds or tenting of the skin anteriorly, the fracture should be considered as being open.
It is important to check for pulses.
If diminished or absent, pulses should be assessed with Doppler.
The ankle-brachial indices should be obtained if there is a concern for arterial injury.
Any side-to-side difference or value less than 0.9 warrants an arteriogram.
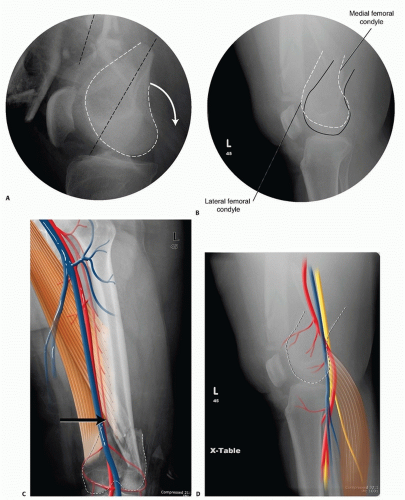
Computed tomography (CT) arteriogram has been used with increasing frequency as well in cases where there is concern (FIG 4).
Nerve function should be checked. Sensation and both active dorsiflexion and plantarflexion must be assessed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The initial imaging study is always plain radiographs. Anteroposterior (AP) and lateral radiographs of the knee should be obtained initially.
Traction films should be obtained if there is severe comminution of either the metaphysis or articular surface. This aids in the preoperative planning.
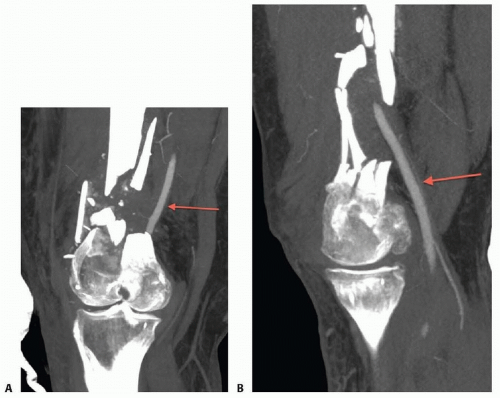
FIG 4 • A,B. Coronal and sagittal CT angiography images showing intact femoral artery in a severely comminuted distal femur fracture (red arrows).
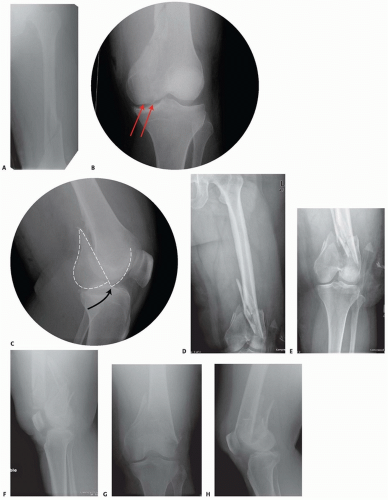
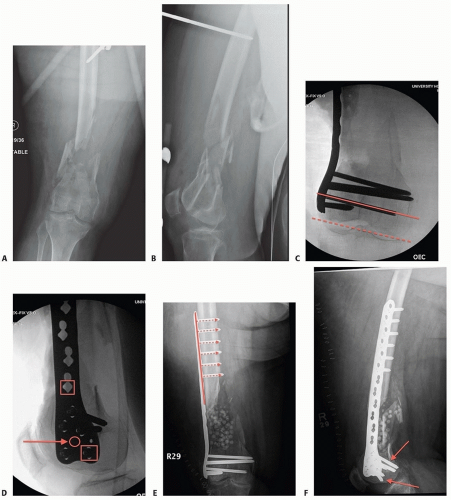
Dedicated knee films should always be obtained in the assessment of distal femur fractures. Additionally, the entire femur, to include the hip and knee, should be imaged to look for possible extension and associated injuries and to allow for preoperative planning (FIG 5).
In cases of severe comminution, radiographs of the contralateral knee can aid in preoperative planning as well.
A dedicated CT scan is an important adjunct to the preoperative planning when there is articular involvement (FIG 6).
Generally, extra-articular distal femur fractures do not require a CT scan. However, it has been shown that coronal fractures may be missed on plain films, and thus there is a low threshold for obtaining a CT scan for fractures of the distal femur.11
If the fracture pattern warrants a temporary bridging external fixator, it is best to obtain the CT scan after placement of such a fixator for better definition.
Coronal and sagittal reconstructions should be requested.
Three-dimensional images can be created from most CT scans. This can also aid in the preoperative planning (FIG 7A,B).
Subtle sagittal plane rotational malalignment between condyles can be assessed (FIG 7C).
If associated soft tissue injury is suspected, such as ligamentous tears or tendon ruptures, then magnetic resonance imaging (MRI) may be indicated. Routine use of MRI, however, is not needed.
DIFFERENTIAL DIAGNOSIS
Proximal tibia fracture
Femoral shaft fracture
Septic knee
Patella fracture
Anterior cruciate ligament rupture
Knee dislocation
NONOPERATIVE MANAGEMENT
There are few relative indications for nonoperative management of distal femur fractures:
Poor overall medical condition
Patient has severe comorbidities and is too sick for surgery.
Patient has extremely poor bone stock.
Spinal cord injury (paraplegia or quadriplegia)
Some special situations may warrant nonoperative care on case-by-case basis.
Nondisplaced or minimally displaced fracture
Select gunshot wounds with incomplete fractures
Extra-articular and stable
Unreconstructable
Lack of experience by the available surgeon or lack of equipment or appropriate facility to adequately treat the injury. Transfer is indicated in these situations; otherwise, nonoperative treatment may be the only option.
There are several methods for nonoperative treatment.
Skeletal traction
Cast bracing
Knee immobilizer
Long-leg cast
There are acceptable limits for nonoperative management:
Seven degrees of varus or valgus
Ten degrees of anterior or posterior angulation. A flexion deformity is less well tolerated than an extension deformity.
Up to 1 to 1.5 cm of shortening
Two to 3 mm of step-off at the joint surface
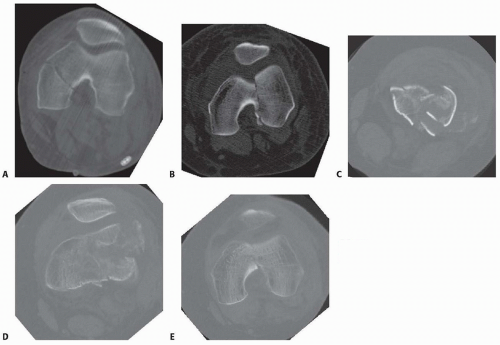 FIG 6 • A. Axial CT image of patient in FIG 5A-C confirming the type B3 fracture of the medial femoral condyle. B. Axial CT image of the patient in FIG 5D-F. C-E. CT images of the patient in FIG 5G,H show the nondisplaced intercondylar split as well as the low lateral fracture line and extensive posterior metaphyseal comminution (type C2). |
 FIG 7 • AP (A) and lateral (B) views of a three-dimensional (3-D) CT reconstruction of the patient in FIG 3B with a distal femur fracture. The fracture is well defined. C. An oblique 3-D CT reconstruction view showing the same patient and the rotational malalignment between condyles. |
SURGICAL MANAGEMENT
The goal of any treatment, nonoperative or operative, is to maintain or restore the congruity of the articular surface and restore the length and alignment of the femur and, subsequently, the limb.
Once surgery is deemed appropriate for the patient and the particular injury, the surgical technique options available are determined by the particular fracture pattern.
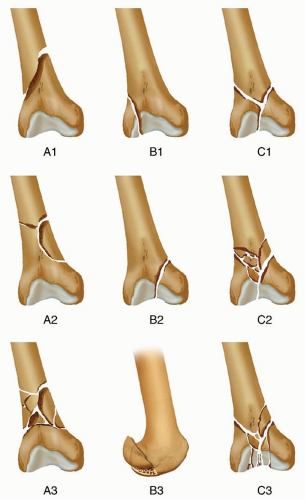
Distal femur fractures have been classified several ways.
Treatment also must be determined based on factors other than the classification alone.
The degree of comminution and injury to both the articular surface and bone
The amount of fracture displacement
The soft tissue injury
Associated injuries, other fractures, and injury to neurovascular structures
Table 1 OTA/AO Classification of Femoral Fractures
Classification
Description
Type A
Extra-articular
A1
Simple or two-part fracture
A2
Metaphyseal butterfly or wedge fracture
A3
Metaphysis is comminuted
Type B
Partial articular
B1
Sagittal plane fracture of the lateral femoral condyle
B2
Sagittal plane fracture of the medial femoral condyle
B3
Any frontal or coronal plane fracture of the condyle (Hoffa type)
Type C
Intra-articular
C1
Simple articular split and metaphyseal injury (T or Y fracture configuration)
C2
Simple articular split with comminuted metaphy-seal injury
C3
Comminuted articular with varying metaphyseal injury
Patient’s overall condition and injury to other organ systems. This may affect the timing of surgery or the positioning of the patient.
There are several principles for the surgical management of distal femur fractures.
The articular surface must be reduced anatomically, which usually requires direct visualization through an open exposure (arthrotomy). Simple intra-articular splits may be treated with closed reduction and percutaneous fixation.
The extra-articular injury should be dealt with using indirect reduction techniques as much as possible to maintain a biologic soft tissue envelope. Avoidance of stripping of the tissues, especially on the medial side, is ideal.
The surgeon must reestablish the length, rotation, and alignment of the femur and the limb.
The soft tissue injury and bone quality may dictate treatment decisions.
Fixation Choices
External fixation
A temporary bridging external fixator across the knee joint can be used if temporary stabilization is required before definitive fixation. This is usually the case where definitive open reduction and internal fixation (ORIF) is planned. This could be in cases where the soft tissues prevent immediate fixation.
Definitive management with bridging or nonbridging external fixation can be used for nonreconstructible joints, very severe soft tissue injuries, or severe osteopenia.
Bridging external fixation can be used when definitive ORIF is problematic in certain patient populations, such as Jehovah’s witnesses, where additional blood loss can lead to increased morbidity or mortality. This can be done temporarily until the patient’s condition improves or until healing (FIG 9).
Intramedullary nailing
This can be performed fairly acutely; temporary bridging external fixation is not necessary.
Antegrade intramedullary nailing has been described and can be used for distal fractures with a large enough distal segment to allow for two locking screws. Malalignment has been a problem, as has adequate fixation.4, 8
Retrograde intramedullary nailing can be used in the following cases (FIG 10):
All extra-articular type A fractures greater than 4 cm from the joint. This minimal length of the distal femur allows for multiplanar interlocking in the distal fragment.
Type C1 or C2 fractures where the articular fracture can be anatomically reduced closed or with limited exposure. Percutaneous screws are used for the articular injury.
Periprosthetic fractures around a total knee arthroplasty with an “open box” femoral component
Most surgeons prefer to use a long nail, but short supracondylar nails are available as well. Multiple-hole short supracondylar nails have fallen out of favor.
Plate fixation
ORIF with plates can be used for all types A and C fractures but is ideal for the following injuries:
Very distal type A fractures within 4 cm of the knee joint
All articular type C fractures, but always for C3 types
Periprosthetic fractures about a “closed box” femoral component of a total knee arthroplasty
The partial articular type B1 or B2 if an antiglide plate is needed
Plate options (preferred to least preferred; fixed-angle devices preferred)
Fixed-angle locking plates (percutaneous jigs are advantageous and allow for minimally invasive techniques)
Variable-angle (polyaxial) locking plates—allow for “fixed variable locking” within a defined range. It is useful for distal fractures and allows for increased screw
trajectories to gain additional locked fixation in short segments, which may not be feasible with fixed-angle trajectory plates (FIG 11).
Ninety-five-degree condylar screw
Ninety-five-degree blade plate
Nonlocking plates with or without medial support (medial plate or external fixation)
Limited internal fixation
Limited fixation with screws only can be used for partial articular type B, especially type B3.
The amount of open reduction required depends on the adequacy of closed reduction techniques and obtaining an anatomic reduction of the joint surface.
Headless screws are useful for type B3 fractures in which the screws have to penetrate the joint surface (FIG 12).
Countersinking the screw heads can also be performed.
Biomechanics of fixation: implant considerations
There has been concern that the newer locking plate constructs are too stiff, resulting in inconsistent and asymmetric callus formation.9
Some clinical evidence show less callus formation with stainless steel plates versus titanium plates.9
Conversely, a biomechanical study has not shown a significant difference mechanically between constructs of stainless steel LISS plates with bicortical screws or titanium LISS plate with unicortical screws.1
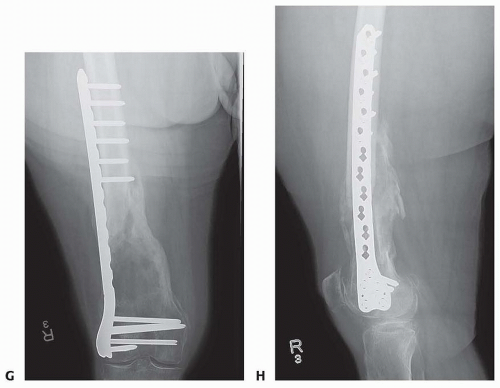
FIG 11 • (continued) G,H. Five-month follow-up films showing replacement of the calcium sulfate beads with successful consolidation of the metaphyseal comminution.
The flexibility of fixation constructs can be increased by the use of a technique referred to as far cortical locking. Specialized screws are used, in which the screw locks into the plate and only engages the far cortex. This has been thought to improve fracture healing.5
Preoperative Planning
Surgical timing can be affected by the following:
Soft tissue issues
Medical condition of the patient
Adequacy of available operative team
Availability of implants
The approach must take the following issues into consideration:
The ability to incorporate lacerations in open fractures into the incision (FIG 13) can be useful and should be considered. However, this is not always necessary or possible.
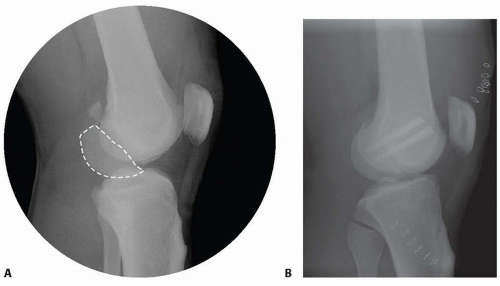
FIG 12 • A. Lateral radiograph of patient with a grade II open distal medial femoral condyle fracture (type B3). The Hoffa fragment is outlined. B. Postoperative radiograph after fixation with headless screws, buried underneath the subchondral bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access