Nontraumatic Osteonecrosis of the Femoral Head
Kristofer J. Jones
Charles L. Nelson
CLINICAL PRESENTATION
Osteonecrosis, also referred to as avascular necrosis, of the femoral head is a term used to refer to a pathologic process that results in osteocyte death with subsequent structural changes that result in femoral head collapse and secondary arthritic changes at the hip joint. While the incidence and prevalence of osteonecrosis of the femoral head varies with the populations from which the data are derived, it has been estimated to develop in 10,000 to 20,000 new patients each year in the United States with an approximated male to female ratio of 4:1. The pathogenesis of osteonecrosis remains poorly understood, and there is no current consensus regarding a specific pathologic event that causes cellular (osteocyte) death. At present, the most commonly accepted mechanism of cellular death is impairment of circulation to the affected areas of bone with potential underlying causes including intravascular coagulation, increased intraosseous pressure, hyperviscosity, venous stasis, or fat emboli occlusion. Given the wide array of etiologic factors contributing to nontraumatic osteonecrosis, it is appropriate to consider the condition as a multifactorial, heterogenous group of disorders that lead to an irrevocable common pathology typified by mechanical collapse of the femoral head.
Patients with nontraumatic osteonecrosis typically present in their third through fifth decades of life. If the hip is involved, typical complaints include pain localized to the groin, although occasional radiation of symptoms to the knee or buttock is not uncommon. The pain is usually characterized as a deep, throbbing pain that may be insidious in nature but then becomes more severe over time. Patients frequently report the pain is exacerbated with ambulation, and they frequently describe mechanical symptoms (catching or popping sensation) with hip range of motion. When obtaining the patient’s history, it is important to identify any risk factors that may predispose the patient to nontraumatic osteonecrosis (Table 12-1), as these underlying disorders will also need to be addressed.
PHYSICAL FINDINGS
Initial assessment of patients with osteonecrosis should include a comprehensive examination of the musculoskeletal system, as the systemic nature of contributing disorders may lead to involvement of other joints (e.g., shoulder, knee, etc.). Upon initial observation, patients typically exhibit an antalgic limp or Trendelenburg gait. Focused examination of the
involved hip should begin with an assessment of passive and active range of motion. Limitation of hip flexion as well as internal rotation is common, and most patients demonstrate tremendous pain with passive internal rotation. As 40% to 80% of cases are bilateral, evaluation of patients with osteonecrosis should focus on both hips.
involved hip should begin with an assessment of passive and active range of motion. Limitation of hip flexion as well as internal rotation is common, and most patients demonstrate tremendous pain with passive internal rotation. As 40% to 80% of cases are bilateral, evaluation of patients with osteonecrosis should focus on both hips.
TABLE 12-1 Risk Factors for Development of Nontraumatic Osteonecrosis | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
STUDIES (LABS, X-RAYS)
Plain Radiography
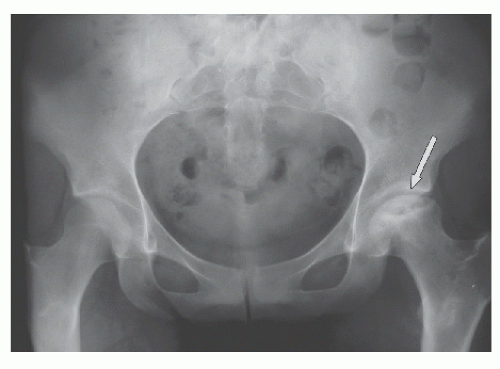
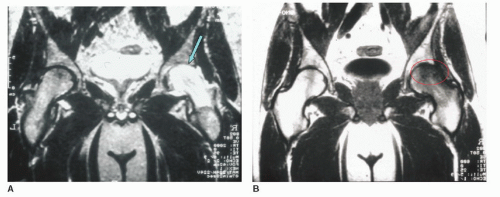
Initial diagnostic imaging should begin with anteroposterior (AP) and frog-leg lateral radiographs of the involved hip. These radiographs should be scrutinized for any abnormalities in the femoral head, including the crescent sign (Fig. 12-2), which may indicate impending structural collapse of the femoral head. Additionally, lesion size, osteophyte formation, joint congruity, and joint space should be characterized (Fig. 12-3). Frog-leg lateral radiographs can be particularly helpful in the detection of any pathology in the anterior segment of the femoral head, which is commonly the initial area to exhibit early structural collapse. If radiographic evaluation demonstrates changes consistent with osteonecrosis, no additional tests are necessary, and this information can be used to stage femoral head osteonecrosis according to the Ficat-Arlet classification (Table 12-2). However, it is important to note that radiographs may not always reveal abnormalities in the early phase of disease. Unfortunately, because plain radiography is designed to identify bone density changes related to remodeling, clear evidence of areas of necrosis may not be noticed for months to years after the initial development of the disorder. Ultimately, there must be a high index of suspicion for osteonecrosis in any patient who complains of pain in the hip, has negative radiographic findings, and has any identifiable risk factors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree